Introduction

Are you meticulous, detail-oriented, and looking for a stable, in-demand career in the healthcare industry that doesn't involve direct patient care? If so, the world of medical billing and coding might be your perfect fit. This crucial field forms the backbone of the healthcare revenue cycle, ensuring that medical providers are properly compensated for their services. For those residing in the Sunshine State, the prospects are particularly bright. A career in this field offers not just a steady job but a competitive medical billing and coding salary in Florida, with significant room for growth and specialization.
The financial landscape for this profession in Florida is robust. While entry-level positions offer a solid starting wage, experienced and certified professionals can command impressive salaries, often exceeding the national average. On average, you can expect to earn anywhere from $45,000 to over $75,000 annually, depending on a confluence of factors we will explore in detail. This isn't just a job; it's a career path with a clear trajectory for advancement and increased earning potential.
I was once reminded of the profound importance of this role when helping a family member decipher a complex hospital bill. The string of alphanumeric codes and medical jargon was utterly impenetrable, leading to confusion and anxiety. It was a certified medical coder who, in a brief phone call, translated the "medical-ese" into plain English, identified a minor coding error, and saved my family member hundreds of dollars. That experience crystallized for me that these professionals aren't just data entry clerks; they are financial navigators and detectives of the healthcare world, bringing clarity and precision to a system that desperately needs it.
This guide is designed to be your definitive resource for understanding everything about a medical billing and coding career and salary in Florida. We will dissect salary expectations, explore the factors that can maximize your income, and provide a clear, step-by-step roadmap to get you started.
### Table of Contents
- [What Does a Medical Biller and Coder Actually Do?](#what-do-they-do)
- [Average Medical Billing and Coding Salary in Florida: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors)
- [Job Outlook and Career Growth in Florida](#job-outlook)
- [How to Get Started in a Medical Billing and Coding Career](#how-to-start)
- [Conclusion: Is a Medical Billing and Coding Career in Florida Right for You?](#conclusion)
What Does a Medical Biller and Coder Actually Do?

While often spoken of in the same breath, medical billing and medical coding are two distinct, yet deeply interconnected, functions. Think of them as two sides of the same coin, both essential for the financial health of any medical practice, clinic, or hospital.
Medical Coding: The Language Translators of Healthcare
At its core, medical coding is a process of translation. A medical coder takes a patient's medical chart—which includes the doctor's notes, lab results, diagnoses, and descriptions of procedures—and translates every piece of information into a set of universal alphanumeric codes. These aren't random numbers and letters; they are part of highly regulated, standardized systems that are understood by healthcare providers, insurance companies, and government agencies worldwide.
The primary code sets used are:
- ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification): This massive library of codes is used to classify every possible diagnosis, symptom, and cause of injury. If a patient has the flu, a broken arm, or diabetes, there is a specific ICD-10-CM code for it.
- CPT (Current Procedural Terminology): Maintained by the American Medical Association (AMA), these codes describe every medical, surgical, and diagnostic service rendered to a patient. An office visit, an X-ray, and a complex surgery each have their own CPT code.
- HCPCS Level II (Healthcare Common Procedure Coding System): These codes are used for products, supplies, and services not included in CPT, such as ambulance services, durable medical equipment (like walkers or wheelchairs), and specific drugs.
A coder's job is to read the medical record with an almost forensic level of detail, ensuring they select the most accurate and specific codes to represent the patient's visit. This requires a strong understanding of anatomy, physiology, and medical terminology.
Medical Billing: The Financial Navigators
Once the coder has translated the visit into a set of codes, the medical biller takes over. The biller uses these codes to create a "superbill" or claim, which is essentially an invoice sent to the patient's insurance company for reimbursement.
The biller's role is multifaceted and requires a blend of administrative skill and tenacity. They are responsible for:
- Claim Creation and Submission: Creating accurate claims with patient demographic information, insurance details, and the codes provided by the coder. These are then submitted electronically to the insurance payer.
- Payment Posting: Once the insurance company processes the claim, the biller posts the payment details into the system, noting what was paid, what was adjusted, and what remains as the patient's responsibility (deductibles, co-pays, co-insurance).
- Denial Management and Appeals: This is where a great biller truly shines. Insurance companies often deny claims for a variety of reasons—a simple data entry error, a lack of pre-authorization, or a dispute over medical necessity. The biller must investigate the reason for the denial, correct any errors, and often write and submit a formal appeal to get the claim paid.
- Patient Invoicing and Collections: The biller is also responsible for sending statements to patients for their portion of the bill and managing the collections process for outstanding balances.
> ### A Day in the Life of a Medical Coder in Florida
>
> Meet "Isabella," a Certified Professional Coder (CPC) working remotely for a large orthopedic group based in Tampa, FL.
>
> * 8:30 AM: Isabella logs into the Electronic Health Record (EHR) system and her coding software. Her queue is populated with patient charts from the previous day's appointments and surgeries.
> * 8:45 AM: She opens her first chart: a patient who underwent an arthroscopic knee surgery. She meticulously reads the surgeon's operative report, the anesthesiologist's notes, and the pre-op diagnosis. She identifies the primary procedure, any additional repairs made, and the post-operative diagnosis.
> * 9:30 AM: She assigns the appropriate CPT codes for the surgery and the ICD-10-CM codes for the patient's condition (e.g., a torn meniscus). She cross-references her choices using her coding manuals and software to ensure accuracy and compliance with payer rules.
> * 11:00 AM: Isabella moves on to a series of simpler office visit charts, coding for conditions like carpal tunnel syndrome, follow-up appointments, and injections. This requires less investigation but just as much attention to detail.
> * 1:00 PM: After lunch, she joins a brief virtual team meeting where the lead coder discusses a recent update from a major insurance payer regarding new documentation requirements for spinal fusions.
> * 2:00 PM: She tackles a complex chart that a new physician documented. The notes are slightly ambiguous, so she flags the chart and sends a secure, HIPAA-compliant message to the physician requesting clarification on a key detail. This proactive communication prevents a likely claim denial down the line.
> * 4:30 PM: Isabella has cleared her queue for the day, having coded over 50 different patient encounters. She spends the last 30 minutes on continuing education, reading an article from the AAPC to stay current on the latest industry trends before logging off.
Average Medical Billing and Coding Salary in Florida: A Deep Dive

Understanding your potential earnings is a critical step in evaluating any career path. For medical billing and coding, the salary landscape is promising, particularly in a high-demand state like Florida. Let's break down the numbers from national averages to state-specific data, looking at the full compensation picture.
### National Salary Benchmarks
To set a baseline, it's helpful to first look at the national data. The U.S. Bureau of Labor Statistics (BLS) is the gold standard for occupational data. The BLS groups medical billers and coders under the broader category of "Medical Records Specialists."
- According to the most recent data from the BLS Occupational Outlook Handbook (published May 2023), the median annual wage for medical records specialists nationally was $48,780. This means half of the workers in the field earned more than that amount, and half earned less.
- The lowest 10 percent earned less than $34,570.
- The highest 10 percent earned more than $84,850.
This wide range highlights the significant impact that factors like experience, certification, and location have on earnings.
### Florida-Specific Salary Data
Now, let's zoom in on the Sunshine State. Florida's large and growing population, particularly its significant senior demographic, creates a massive demand for healthcare services, which in turn fuels the need for skilled billing and coding professionals. This demand often translates into more competitive salaries compared to other regions.
Authoritative salary aggregators provide a more granular look at the medical billing and coding salary in Florida:
- Salary.com reports that the average salary for a Medical Biller/Coder in Florida is approximately $59,033 as of late 2023/early 2024, with a typical range falling between $51,694 and $67,994.
- Payscale.com indicates a slightly broader range, with the average base salary for a Medical Coder in Florida sitting around $52,000 per year, but this can vary widely based on the specific city and years of experience.
- Indeed.com aggregates data from job postings and user-submitted information, showing an average base salary of approximately $50,210 per year for Medical Coders in Florida.
It's important to note the slight variations between these platforms. Salary.com often reflects employer-reported data for established roles, while Indeed and Payscale can include more entry-level positions and user-reported figures. The most realistic expectation is that the true average lies somewhere within the intersection of these data points, confirming that a range of $50,000 to $60,000 is a very reasonable expectation for a certified professional with a few years of experience in Florida.
### Salary Progression by Experience Level
Your salary is not a static number; it's a dynamic figure that will grow substantially as you gain experience and expertise. Here is a typical salary trajectory for a medical billing and coding professional in Florida, compiled from industry data.
| Experience Level | Typical Years of Experience | Typical Annual Salary Range (Florida) | Key Characteristics & Responsibilities |
| :--- | :--- | :--- | :--- |
| Entry-Level / Apprentice | 0 - 2 years | $38,000 - $48,000 | Recently certified, often working under supervision. Focuses on data entry, simple office visit coding, payment posting, and learning specific software and payer rules. |
| Mid-Career / Professional | 2 - 7 years | $49,000 - $65,000 | Holds at least one core certification (e.g., CPC). Can handle a variety of coding scenarios, including outpatient procedures. May begin to handle claim denials and light appeals. |
| Senior / Specialist | 8 - 15+ years | $66,000 - $80,000+ | Holds multiple certifications (e.g., in a specialty like surgery or risk adjustment). Audits other coders' work, handles complex appeals, trains junior staff, and may manage a small team. |
| Management / Auditing | 10+ years | $75,000 - $95,000+ | Manages a department, oversees revenue cycle integrity, conducts high-level audits, develops coding policies, and liaises with physicians and hospital administration. |
*(Salary ranges are estimates compiled from BLS, Salary.com, and AAPC salary survey data and are subject to change based on the specific factors discussed in the next section.)*
### Beyond the Base Salary: The Total Compensation Package
Your base salary is only one part of the equation. When evaluating a job offer, it's crucial to consider the full compensation package, which can add significant value. Common components in Florida include:
- Bonuses: Many larger healthcare organizations and billing companies offer performance-based bonuses. These can be tied to individual productivity (e.g., coding accuracy rate, number of claims processed) or departmental financial goals (e.g., reducing the claim denial rate). These can range from a few hundred to several thousand dollars annually.
- Profit Sharing: Some private practices or physician-owned groups may offer profit-sharing plans, where a portion of the company's profits is distributed among employees.
- Health Insurance: Given the industry, healthcare employers typically offer comprehensive health, dental, and vision insurance plans. The value of an employer-subsidized plan can be worth thousands of dollars per year.
- Retirement Savings: Access to a 401(k) or 403(b) plan, especially with an employer match, is a critical long-term financial benefit. An employer matching 3-5% of your salary is essentially a 3-5% raise dedicated to your retirement.
- Paid Time Off (PTO): This includes vacation days, sick leave, and personal days. A generous PTO policy is a valuable part of work-life balance.
- Continuing Education Stipend: Top-tier employers understand the importance of ongoing education in this field. They may offer a stipend to cover the cost of maintaining your certifications, attending conferences, or purchasing coding books and resources. This is a huge perk that supports your career growth.
When you combine a competitive base salary with these benefits, the true value of a medical billing and coding position in Florida becomes even more attractive.
Key Factors That Influence Your Salary
While we've established a solid baseline for a medical billing and coding salary in Florida, your individual earning potential is not set in stone. It is influenced by a dynamic interplay of several key factors. Mastering these elements is the secret to not just starting a career, but actively managing it toward higher income levels. This is where you move from being a passive employee to the CEO of your own career.
### `
` Geographic Location Within Florida: The Sunshine State's Micro-Economies
Florida is a large and diverse state, and salary expectations can vary significantly from one metropolitan area to another. This variance is typically driven by the local cost of living and the concentration of major healthcare systems. High-cost-of-living areas with numerous large hospitals and specialty clinics will almost always offer higher wages to attract and retain talent.
Here's a comparative look at estimated average salaries in major Florida cities:
| Metropolitan Area | Estimated Average Annual Salary | Local Market Dynamics |
| :--- | :--- | :--- |
| Miami-Fort Lauderdale-West Palm Beach | $60,000 - $68,000 | Highest cost of living in the state. Home to major hospital networks like Baptist Health South Florida and Memorial Healthcare System. High demand for bilingual (English/Spanish) coders and specialists. |
| Orlando-Kissimmee-Sanford | $55,000 - $63,000 | A rapidly growing region with major players like AdventHealth and Orlando Health. A competitive market with many opportunities in both large hospitals and specialized clinics. |
| Tampa-St. Petersburg-Clearwater | $54,000 - $62,000 | A robust healthcare hub with institutions like Tampa General Hospital and BayCare Health System. Strong demand across various specialties. |
| Jacksonville | $53,000 - $61,000 | Home to renowned medical centers like the Mayo Clinic and UF Health Jacksonville. A slightly lower cost of living than South Florida, but still a very strong market for healthcare professionals. |
| Gainesville | $52,000 - $59,000 | Dominated by the University of Florida and UF Health Shands Hospital, creating a concentrated demand for academic and complex medical coding. |
| Tallahassee / Panhandle Region | $48,000 - $55,000 | Lower cost of living translates to slightly lower salary ranges. Opportunities are often centered around regional hospitals and state government-related health agencies. |
| Rural Areas | $42,000 - $50,000 | Fewer large employers and lower cost of living result in the most modest salary expectations. However, remote work opportunities are changing this dynamic, allowing rural residents to access higher-paying jobs. |
*(Source: Data compiled and synthesized from Salary.com, Glassdoor, and Indeed city-specific salary reports.)*
Key Takeaway: If maximizing your salary is the primary goal, targeting positions in the major metropolitan hubs of South Florida, Tampa, or Orlando is your best strategy. However, the rise of remote work is a game-changer, potentially allowing you to live in a lower-cost area while earning a salary competitive with a major metro market.
### `
` Certifications: Your Golden Ticket to Higher Pay
In the medical billing and coding field, professional certification is not just a suggestion—it is the single most important factor in unlocking your earning potential and professional credibility. An uncertified coder is often limited to the most basic, lowest-paying roles. Certification demonstrates a standardized level of knowledge, a commitment to the profession, and proficiency in the complex rules of coding.
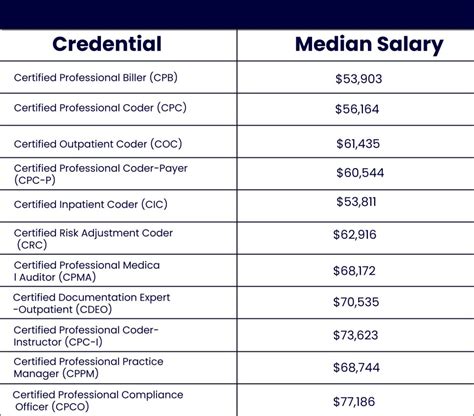
According to the AAPC's annual salary survey, certified coders earn, on average, 20-30% more than their non-certified counterparts.
Here are the most influential certifications and their impact:
- CPC (Certified Professional Coder): Offered by the AAPC, this is the most recognized and sought-after certification for physician-based (outpatient) coding. It is the gold standard for most coding jobs and is the essential first step for any serious professional.
- CCS (Certified Coding Specialist): Offered by AHIMA (American Health Information Management Association), this certification is highly respected for hospital-based (inpatient) coding. Inpatient coding is generally more complex than outpatient coding and often commands a higher salary.
- RHIT (Registered Health Information Technician): Also from AHIMA, this certification requires an associate's degree from an accredited program. It provides a broader knowledge of health information management, including coding, data analytics, and compliance, often leading to supervisory or health informatics roles.
- Specialty Certifications: Once you have a core certification like the CPC, earning specialty certifications can significantly boost your value. These demonstrate expertise in a specific, often complex, area of medicine. Examples include:
- COC (Certified Outpatient Coder) - For hospital outpatient facilities
- CIC (Certified Inpatient Coder) - For hospital inpatient coding
- CRC (Certified Risk Adjustment Coder) - A high-demand, high-paying specialty focusing on coding for patient risk scores.
- Surgical Specialties (e.g., CASCC for Ambulatory Surgery, CGSC for General Surgery) - Surgical coding is intricate and commands premium pay.
Key Takeaway: Do not treat certification as optional. Plan to get your CPC or CCS as soon as possible after your training. Then, strategically pursue additional certifications in high-demand or high-complexity areas to maximize your career-long earnings.
### `
` Years of Experience: The Climb to Senior-Level Earnings
As shown in the salary progression table earlier, experience is a direct driver of income. In your early years, you are building speed, accuracy, and familiarity with different medical scenarios and payer-specific rules. As you accumulate experience, you become a more valuable asset capable of handling more complex tasks.
- 0-2 Years: You are an investment. Your employer is training you and getting you up to speed. Your focus should be on learning, absorbing information, and achieving high accuracy.
- 2-7 Years: You are a reliable engine. You can work independently, handle a full workload, and may start to mentor newer coders. This is where you see the most significant jump from entry-level pay.
- 8+ Years: You are an expert and a problem-solver. You are the go-to person for difficult cases, complex appeals, and auditing. You may be involved in training physicians on documentation improvement. This level of expertise commands the highest salaries in non-management roles.
### `
` Type of Work Environment: Where You Work Matters
The setting in which you work has a direct correlation with salary, primarily due to the complexity of the work involved.
- Hospitals (Inpatient & Outpatient): Hospitals generally offer the highest salaries. Inpatient coding (CCS credential) is particularly lucrative because it involves complex, high-dollar cases like major surgeries and extended stays. Hospital outpatient departments also require specialized knowledge and often pay very well.
- Large Multi-Specialty Clinics: These environments offer exposure to a wide variety of medical fields and often have compensation structures that are competitive with hospitals.
- Physician's Offices (Single Specialty): While the work might be less complex than in a hospital, a coder in a specialized practice (like oncology, cardiology, or orthopedics) can become an invaluable expert and earn a high salary.
- Third-Party Billing Companies: These companies handle billing and coding for multiple clients. The pace can be fast, and while entry-level pay might be standard, experienced coders who can manage multiple accounts and complex denials are highly valued.
- Remote Work: The ability to work from home is one of the most significant perks in the industry. While salaries for remote positions are competitive, they are often based on the employer's location or a national average rather than the employee's. This can be a huge advantage for someone living in a low-cost area of Florida working for a company based in a high-cost area like Miami or even New York.
### `
` Area of Specialization (Coding Specialty)
Just as doctors specialize, so can medical coders. Developing deep expertise in a specific area of medicine is one of the most effective ways to increase your salary and job security. Complex specialties require a higher level of knowledge and skill, and employers are willing to pay a premium for that expertise.
High-Paying Specialties Include:
- Interventional Radiology & Cardiology: Coding for these intricate, minimally invasive procedures requires a deep understanding of anatomy and complex procedural guidelines.
- Oncology: Cancer treatment involves complex coding for chemotherapy, radiation, and numerous diagnostic tests, often spanning long periods.
- Risk Adjustment (CRC): This is one of the fastest-growing and highest-paying areas. Risk adjustment coders review patient charts to ensure all chronic conditions are accurately documented to determine a patient's risk score, which directly impacts payments from Medicare Advantage plans.
- Surgical Coding: Coding for complex surgical procedures requires dissecting operative reports and is a highly valued skill.
### `
` In-Demand Skills & Proficiencies
Beyond certifications and experience, a specific set of skills can make you a more attractive and higher-paid candidate:
- Software Proficiency: Expertise in major Electronic Health Record (EHR) systems like Epic, Cerner, or eClinicalWorks is a huge plus.
- Auditing and Compliance: Skills in auditing other coders' work for accuracy and compliance with federal regulations (like HIPAA) can lead to senior roles.
- Denial Management Expertise: A proven track record of successfully appealing and overturning claim denials is a highly valuable, revenue-generating skill.
- Bilingualism: In a diverse state like Florida, proficiency in Spanish is a significant advantage, particularly in the South Florida market.
- Soft Skills: Do not underestimate the power of strong communication (for querying physicians), critical thinking (for solving complex coding puzzles), and unwavering attention to detail.
Job Outlook and Career Growth in Florida
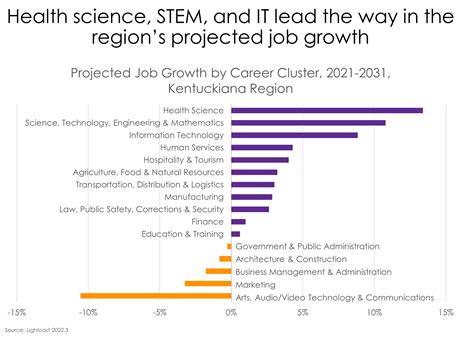
Choosing a career is not just about the starting salary; it’s about long-term stability and opportunities for advancement. For medical billing and coding, the future is exceptionally bright, both nationally and within the state of Florida.
### A Profession on the Rise: The BLS Projections
The U.S. Bureau of Labor Statistics (BLS) provides a robust forecast for the profession. For "Medical Records Specialists," the BLS projects a job growth of 7 percent from 2022 to 2032. This is more than twice the average growth rate for all occupations, which stands at 3 percent.
What does this mean in real numbers? The BLS anticipates the creation of approximately 14,900 new jobs in this field each year, on average, over the decade. This growth is driven by several powerful, long-term trends:
1. The Aging Population: As the massive baby-boomer generation ages, their need for medical services will continue to increase. More doctor visits, more diagnostic tests, and more medical procedures directly translate to a greater volume of medical claims that need to be coded and billed. Florida, as a top retirement destination, is at the epicenter of this demographic shift, amplifying the demand locally.
2. Increasing Complexity of Healthcare Regulation: The world of medical coding is constantly evolving. The transition from ICD-9 to ICD-10 drastically increased the number of codes, and updates are released annually. Furthermore, evolving payment models, such as value-based care, require more detailed and accurate data, making skilled coders more crucial than ever.
3. **Widespread Use of Electronic Health Records