For those driven by a passion to heal, to empower, and to witness firsthand the remarkable resilience of the human heart, a career as a cardiac rehabilitation specialist offers a profound sense of purpose. This is not merely a job; it is a vocation dedicated to guiding patients back from a life-altering cardiac event—a heart attack, a surgery, a diagnosis—towards a future of strength, confidence, and vitality. It's a role where your expertise in exercise science and patient care directly translates into someone else's second chance at life.
But passion, while essential, must be paired with practicality. As you consider this noble career path, a crucial question naturally arises: what is the earning potential? The cardiac rehab specialist salary is a key component of your decision-making process, reflecting the value of your skills, education, and dedication in the professional world. Nationally, cardiac rehab specialists can expect to earn an average salary ranging from approximately $60,000 to $78,000 per year, with top earners and those in management positions exceeding $95,000 annually.
I once had the privilege of speaking with a patient who, six months prior, had been terrified to walk up a flight of stairs after his heart surgery. He tearfully recounted how his cardiac rehab specialist not only rebuilt his physical strength but, more importantly, dismantled the fear that had imprisoned him. She gave him the tools and the confidence to not just live, but to thrive. It is this transformative impact—this blend of clinical science and compassionate coaching—that defines the essence of the profession and underpins its value.
This comprehensive guide will illuminate every facet of a cardiac rehab specialist's career, with a deep and authoritative focus on salary, career trajectory, and what it takes to succeed. We will dissect the numbers, explore the influencing factors, and provide a clear roadmap for you to embark on this fulfilling journey.
### Table of Contents
- [What Does a Cardiac Rehab Specialist Do?](#what-does-a-cardiac-rehab-specialist-do)
- [Average Cardiac Rehab Specialist Salary: A Deep Dive](#average-cardiac-rehab-specialist-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion: A Career with Heart and Financial Stability](#conclusion-a-career-with-heart-and-financial-stability)
What Does a Cardiac Rehab Specialist Do?

A Cardiac Rehabilitation Specialist is a certified healthcare professional, typically an Exercise Physiologist, Registered Nurse, or Physical Therapist, who specializes in helping patients recover from heart attacks, heart surgery (like bypass or valve replacement), angioplasty, or other serious cardiac conditions. Their work is a cornerstone of secondary prevention, aiming to stabilize, slow, or even reverse the progression of cardiovascular disease.
The role is multifaceted, blending clinical assessment, exercise science, patient education, and psychosocial support. These specialists work as part of a multidisciplinary team that may include physicians, cardiologists, dietitians, social workers, and psychologists to provide holistic patient care.
Core responsibilities are typically structured around the phases of cardiac rehabilitation:
- Phase I (Inpatient): This begins in the hospital shortly after a cardiac event. The specialist's role involves low-level ambulation, educating the patient and their family about their condition and the recovery process, and assessing their readiness for the next phase.
- Phase II (Outpatient): This is the most intensive phase and the primary focus for most cardiac rehab specialists. In a clinical setting, they develop, implement, and supervise medically monitored exercise programs tailored to each patient's specific needs and limitations.
- Phase III & IV (Maintenance): These are long-term maintenance programs, often with less intensive monitoring. The specialist helps patients transition to independent exercise, either at the facility or in a community setting like a gym, empowering them to maintain a heart-healthy lifestyle for the rest of their lives.
Breakdown of Daily Tasks:
- Patient Assessment: Conducting initial intake assessments, which include reviewing medical history, evaluating cardiovascular and pulmonary function, and assessing physical strength and flexibility.
- Exercise Prescription & Supervision: Designing individualized exercise plans (IEPs) that specify the type, frequency, duration, and intensity of physical activity. They continuously monitor patients during exercise sessions, tracking vital signs like heart rate, blood pressure, and EKG rhythm, and adjusting the plan as the patient progresses.
- Patient Education: Leading group and one-on-one education sessions on topics crucial for recovery, such as understanding heart medications, managing risk factors (like cholesterol and blood pressure), nutrition, stress management, and smoking cessation.
- Monitoring and Documentation: Meticulously documenting patient progress, vital sign responses, and any adverse events. This information is critical for communicating with the patient's cardiologist and the rest of the healthcare team.
- Emergency Response: Being prepared to respond to medical emergencies, such as arrhythmias or sudden cardiac arrest. All specialists are certified in Basic Life Support (BLS) and Advanced Cardiac Life Support (ACLS).
### A Day in the Life of a Cardiac Rehab Specialist
Imagine starting your day at 8:00 AM in a hospital's outpatient cardiac rehab center. The first hour is spent reviewing the charts of the day's scheduled patients, noting any recent medication changes or overnight concerns reported to their cardiologist. At 9:00 AM, the first group of Phase II patients arrives. You greet each one, help them get set up on telemetry monitors, and lead them through a warm-up. For the next hour, you circulate the gym, monitoring EKG strips on a central console while moving between patients on treadmills, stationary bikes, and resistance training equipment. You're correcting a patient's form on a bicep curl, checking the blood pressure of another post-exercise, and offering words of encouragement to someone who just surpassed a personal goal.
Between sessions, you might lead a 30-minute educational class on heart-healthy nutrition. The afternoon brings another group of patients, followed by administrative time. This involves charting each patient's progress, writing progress reports for referring physicians, and preparing for the next day. You might end your day with a team meeting, discussing a particularly complex patient case with a dietitian and the medical director to ensure the care plan is perfectly aligned. It's a day of constant interaction, clinical vigilance, and tangible impact.
Average Cardiac Rehab Specialist Salary: A Deep Dive
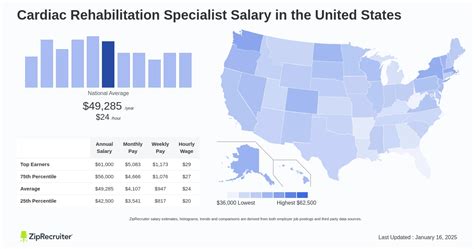
Understanding the financial landscape of a cardiac rehab specialist career requires looking at data from multiple authoritative sources. Since the U.S. Bureau of Labor Statistics (BLS) does not track "Cardiac Rehab Specialist" as a distinct profession, we analyze data for the roles that most commonly hold this specialization—primarily Exercise Physiologists—and supplement this with specific salary data from aggregators who do track the specialized title.
According to the BLS *Occupational Outlook Handbook* (last updated September 2023), the median annual wage for Exercise Physiologists was $54,860 in May 2022. However, this figure represents the entire field, including those in non-clinical or general wellness roles. Specialists in cardiac rehabilitation, due to the critical nature of their work and required certifications, often command higher salaries.
More targeted data provides a clearer picture of the cardiac rehab specialist salary specifically:
- Salary.com: As of November 2023, the average salary for a Cardiac Rehabilitation Specialist in the United States is $63,059, with a typical salary range falling between $56,584 and $70,391.
- Payscale: This platform reports a similar average base salary of approximately $61,080 per year. Their data shows a range from about $46,000 for entry-level positions to over $82,000 for experienced specialists.
- Glassdoor: Glassdoor estimates the total pay for a Cardiac Rehab Specialist to be around $78,579 per year in the United States, with an average base salary of $67,419. The "total pay" figure includes additional compensation like bonuses and profit sharing.
Collectively, these sources suggest a strong consensus that the core salary for a practicing cardiac rehab specialist falls in the $60,000 to $78,000 range, with significant variance based on the factors we will explore below.
### Salary by Experience Level
As with any profession, experience is a primary driver of earning potential. A specialist's value increases as they develop deeper clinical judgment, refine their patient management skills, and take on greater responsibilities.
Here is a typical salary progression based on years of experience, compiled from industry data:
| Experience Level | Typical Years of Experience |
| :--- | :--- |
| Entry-Level Cardiac Rehab Specialist | 0-2 Years |
| Mid-Career Cardiac Rehab Specialist | 3-9 Years |
| Senior/Lead Cardiac Rehab Specialist | 10-15+ Years |
| Cardiac Rehab Program Manager/Director| 15+ Years (with leadership duties) |
Entry-Level (0-2 Years):
At this stage, specialists are focused on applying their academic knowledge in a real-world clinical setting. They work under closer supervision, honing their skills in patient assessment, exercise prescription, and EKG monitoring.
- Typical Salary Range: $46,000 - $58,000
Mid-Career (3-9 Years):
With several years of experience, these professionals operate with greater autonomy. They can manage more complex patient cases, may take the lead on educational initiatives, and often act as mentors to new staff or interns. Their clinical judgment is well-developed.
- Typical Salary Range: $59,000 - $72,000
Senior/Lead (10-15+ Years):
Senior specialists are often the clinical experts in their department. They may handle the most challenging patient populations (e.g., those with multiple comorbidities, LVADs, or heart transplants), lead quality improvement projects, and contribute to program development.
- Typical Salary Range: $73,000 - $88,000
Program Manager/Director (15+ Years):
This is a leadership role that involves moving beyond direct patient care into an administrative capacity. Responsibilities include staff management, budget oversight, ensuring regulatory compliance (with organizations like the AACVPR), and strategic program growth.
- Typical Salary Range: $85,000 - $110,000+
### Beyond the Base Salary: Understanding Total Compensation
Your annual salary is only one piece of the financial puzzle. A comprehensive compensation package significantly enhances your overall earnings and quality of life. When evaluating a job offer, consider the full value proposition.
Common Components of Total Compensation:
- Bonuses: While less common than in corporate roles, some hospital systems or private clinics offer annual performance-based bonuses, often tied to patient outcomes, volume, or departmental financial health.
- Profit Sharing: In private practice settings, a profit-sharing plan may be offered, giving employees a small percentage of the company's profits.
- Retirement Plans: This is a crucial benefit. Most employers, especially hospitals, offer a 401(k) or 403(b) retirement savings plan, often with a valuable employer match (e.g., matching 50% of your contributions up to 6% of your salary).
- Health Insurance: Comprehensive medical, dental, and vision insurance is a standard and highly valuable part of any package in the healthcare industry.
- Paid Time Off (PTO): This includes vacation days, sick leave, and paid holidays. The amount typically increases with seniority.
- Professional Development: Many employers recognize the importance of continuing education. They may provide an annual stipend to cover the costs of attending conferences (like the AACVPR Annual Meeting), renewing certifications, or taking advanced courses. This is a key benefit for career growth.
- Tuition Reimbursement: Some larger hospital networks offer tuition assistance for employees pursuing advanced degrees (e.g., a Master's degree or a nursing degree) that will benefit the organization.
- Life and Disability Insurance: Employer-sponsored short-term and long-term disability insurance provides a crucial safety net in case of an illness or injury that prevents you from working.
When comparing job offers, it's essential to quantify these benefits. A job with a slightly lower base salary but an excellent retirement match and generous professional development fund may be the superior long-term financial choice.
Key Factors That Influence Salary

The national average salary provides a useful benchmark, but your individual earning potential as a cardiac rehab specialist will be determined by a combination of personal and external factors. Understanding these variables is key to negotiating your salary effectively and maximizing your lifetime earnings. This section provides a granular analysis of the most significant influences on your pay.
###
1. Level of Education and Professional Credentials
Your foundational education and specialized credentials are the bedrock of your career and a primary determinant of your starting salary and long-term growth potential.
- Bachelor's Degree: The minimum educational requirement for most cardiac rehab specialist positions is a Bachelor of Science (B.S.) in a related field. The most common and direct path is a degree in Exercise Science or Kinesiology. Other relevant degrees include Exercise Physiology, Health Sciences, or Physical Education. A bachelor's degree qualifies you for entry-level roles and allows you to sit for key professional certifications.
- Master's Degree: Pursuing a Master of Science (M.S.) in a field like Clinical Exercise Physiology or a related discipline can significantly boost your earning potential and career opportunities. A master's degree often leads to higher starting salaries (potentially a 5-15% increase over a B.S. alone) and is frequently a prerequisite for leadership or academic positions. It provides a deeper understanding of pathophysiology, research methods, and advanced clinical practices, making you a more valuable asset to an employer.
- Underlying Professional License (RN, PT, RRT): A significant portion of cardiac rehab specialists are Registered Nurses (RNs), Physical Therapists (PTs), or Registered Respiratory Therapists (RRTs) who have chosen to specialize. These licensed professionals often command higher salaries than those with only an exercise science background, as their scope of practice is broader (e.g., an RN can administer medications). A Cardiac Rehab RN, for instance, might see a salary that aligns more closely with general nursing salaries, which are often higher than those for exercise physiologists. According to the BLS, the median salary for RNs was $81,220 in May 2022, providing a higher baseline for specialists with this credential.
- Professional Certifications: Certifications are non-negotiable in this field and serve as the primary validation of your specialized expertise.
- BLS/ACLS: Basic Life Support (BLS) and Advanced Cardiac Life Support (ACLS) certifications from the American Heart Association are mandatory for anyone working directly with cardiac patients. They are a prerequisite for employment, not a salary booster, but are essential.
- ACSM-CEP: The American College of Sports Medicine Certified Clinical Exercise Physiologist (ACSM-CEP) is a prestigious and highly respected credential. It is designed for professionals who work with patients with a range of cardiovascular, pulmonary, and metabolic diseases. Holding the ACSM-CEP signals a high level of expertise and is often a preferred or required qualification, which can lead to higher pay.
- CCRP (formerly CCREP): The Certified Cardiac Rehabilitation Professional (CCRP), offered by the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR), is the gold standard certification specifically for cardiac rehab professionals. It demonstrates comprehensive knowledge of the entire field, including patient assessment, exercise training, education, and program management. Earning the CCRP is a significant career milestone that can unlock opportunities for advancement and higher salaries, particularly for leadership roles.
###
2. Years of Experience and Career Progression
As detailed in the previous section, experience is a powerful lever for salary growth. The trajectory is not simply about tenure; it's about the accumulation of skills, wisdom, and responsibility.
- Entry-Level (0-2 years; ~$46k - $58k): The focus is on foundational competence. You are mastering EKG interpretation in a real-world context, learning to build rapport with anxious patients, and becoming efficient with documentation and clinical protocols.
- Mid-Career (3-9 years; ~$59k - $72k): You transition from competence to proficiency. Your value lies in your ability to work independently, manage complex patient loads, and contribute to the team's effectiveness. You might be asked to precept students or new hires, demonstrating a level of trust and expertise that justifies higher pay.
- Senior/Lead (10+ years; ~$73k - $88k+): You are now an expert. Your value is strategic. You might be the go-to person for troubleshooting difficult EKG rhythms, developing new educational materials, or piloting new technologies in the clinic. Your deep experience reduces risk and improves patient outcomes, a contribution that organizations are willing to pay a premium for. Specialists at this level who take on formal leadership duties as a Program Coordinator or Manager will see the most significant salary jump, often moving into the $85,000 to $110,000+ range.
###
3. Geographic Location
Where you work has a dramatic impact on your salary. This variation is driven by factors like local cost of living, the demand for healthcare services (often tied to regional demographics), and the presence of unions or strong hospital networks.
High-Paying States and Metropolitan Areas:
States with a high cost of living and large, well-funded healthcare systems tend to offer the highest salaries.
- California: Cities like San Francisco, Los Angeles, and San Diego consistently rank among the highest-paying in the nation for healthcare roles. A cardiac rehab specialist in California can expect to earn 15-30% above the national average.
- New York: The New York City metropolitan area, along with other major cities in the state, offers highly competitive salaries to offset the steep cost of living.
- Washington & Oregon: The Pacific Northwest, particularly around Seattle and Portland, has robust healthcare markets and strong salaries.
- Massachusetts: Driven by Boston's world-class medical centers, Massachusetts offers excellent pay for specialized healthcare professionals.
- Alaska: While less populated, Alaska often pays a premium for healthcare workers to attract talent to the state.
Example Salary Comparison by City (Data from Salary.com, adjusted for title):
- San Francisco, CA: ~ $78,600
- New York, NY: ~ $75,500
- Boston, MA: ~ $71,100
- National Average: ~ $63,000
- Orlando, FL: ~ $60,400
- Oklahoma City, OK: ~ $57,800
Lower-Paying States:
Conversely, states with a lower cost of living, particularly in the Southeast and parts of the Midwest, tend to have salaries that are below the national average. While your paycheck may be smaller, your purchasing power might be comparable or even greater than in a high-cost area. States like Alabama, Mississippi, Arkansas, and South Dakota often fall into this category.
###
4. Work Setting and Employer Type
The type of organization you work for is a major factor in determining your salary and benefits package.
- Large Academic Medical Centers/Hospital Systems: These are often the highest-paying employers. They are typically located in major urban centers, may be unionized, and have large, well-established cardiac rehab programs. They offer structured salary scales (often called clinical ladders), excellent benefits, and ample opportunities for professional development and advancement.
- Community Hospitals: Salaries at smaller community or regional hospitals can be competitive but may lag slightly behind major academic centers. Benefits packages are usually robust. These settings can offer a strong sense of community and a chance to work closely with a consistent group of referring physicians.
- Outpatient Clinics (Physician-Owned or Private): These settings can have more variability. A successful, high-volume cardiology practice may pay very well to attract top talent. However, a smaller clinic might offer a lower base salary but potentially include performance-based bonuses. Benefits can be less comprehensive than at a large hospital.
- Corporate Wellness/Government (e.g., Veterans Affairs): Some large corporations hire exercise physiologists for their executive health or wellness programs, which can be lucrative. Government positions, such as those at a VA hospital, offer exceptional job security and federal benefits, with salaries determined by the General Schedule (GS) pay system. VA salaries are often competitive and publicly available.
###
5. Specialization within the Role
While "cardiac rehab" is already a specialty, further sub-specialization or moving into adjacent roles can influence earnings and career paths.
- Program Leadership & Management: As mentioned, the clearest path to a six-figure salary is to move into administration. A Cardiac Rehab Program Manager or Director oversees the entire service line, including budgets, staffing, marketing, and regulatory compliance. This requires a blend of clinical expertise and business acumen.
- Specialized Patient Populations: Developing expertise in niche areas can make you a more valuable asset. This could include working with:
- Heart Failure Patients: Managing rehab for patients with advanced heart failure and related devices.
- Post-Transplant Patients: Guiding the recovery of heart transplant recipients.
- Pediatric Cardiac Rehab: A highly specialized field working with children who have congenital heart defects.
- Pulmonary Rehabilitation: Many programs are combined cardiovascular and pulmonary rehab centers. Becoming dual-specialized in treating patients with COPD and other lung diseases significantly broadens your skill set and value.
###
6. In-Demand Skills (Hard and Soft)
Beyond your degrees and certifications, a specific set of skills will make you a more effective practitioner and a more attractive candidate, which can translate into better job offers and faster promotions.
High-Value Hard Skills:
- Advanced EKG/ECG Interpretation: The ability to not just recognize basic rhythms but to interpret complex 12-lead EKGs, identify signs of ischemia, and understand nuanced arrhythmias is a top-tier skill that instills confidence in referring cardiologists.
- Exercise Stress Testing: In some settings, cardiac rehab specialists assist with or conduct diagnostic exercise stress tests. This is an advanced skill that requires specific training and can command higher pay.
- Knowledge of Cardiac Devices: Proficiency in working with patients who have pacemakers, implantable cardioverter-defibrillators (ICDs), and Left Ventricular Assist Devices (LVADs) is increasingly critical as these technologies become more common.
- Data Management and Analytics: The ability to use electronic health record (EHR) systems effectively and to track and analyze patient outcome data for quality improvement reports is a highly valued administrative skill.
Essential Soft Skills:
- Empathy and Rapport-Building: Cardiac patients are often dealing with fear, anxiety, and depression. The ability to connect with them on a human level, listen to their concerns, and build a trusting relationship is paramount to their success.
- Motivational Coaching: You are not just a technician; you are a coach. The skill of motivating individuals to make difficult but necessary lifestyle changes is the art of cardiac rehab.
- Exceptional Communication: You must be able to explain complex medical concepts in simple terms to patients, collaborate effectively with a multidisciplinary team, and write clear, concise clinical notes.
- Problem-Solving and Critical Thinking: When a patient's blood pressure drops unexpectedly or they report unusual symptoms, you need to think quickly, assess the situation calmly, and make the right clinical decision.
Job Outlook and Career Growth

The career outlook for cardiac rehabilitation specialists is exceptionally positive, driven by powerful demographic and healthcare trends. For aspiring professionals, this translates into strong job security and ample opportunities for growth in the coming decade.
The U.S. Bureau of Labor Statistics (BLS) projects that employment for Exercise Physiologists is expected to grow by 9 percent from 2022 to 2032, which is much faster than the average for all occupations. The BLS anticipates
