Introduction

Imagine standing under the brilliant, focused lights of an operating room. The rhythmic beep of the heart monitor is the room's steady pulse, and you are an indispensable part of a team holding a human life in your hands. You’re not just an assistant; you are a highly skilled clinician, a trusted practitioner making critical decisions, suturing complex vessels, and often, literally holding a patient's heart. This is the world of the Cardiothoracic (CT) Surgery Physician Assistant—a career at the absolute apex of medical intensity, skill, and reward. For those with the nerve, intellect, and compassion to pursue it, the financial compensation is as significant as the professional satisfaction. A cardiothoracic surgery physician assistant salary often starts in the low six figures and can soar to well over $200,000, reflecting the immense responsibility and expertise required.
This isn't a career for the faint of heart. The hours are long, the stress is palpable, and the learning curve is one of the steepest in the medical field. I once had the privilege of speaking with a veteran CT PA who had just finished a grueling 14-hour day that included a complex triple-vessel bypass surgery. Exhausted but visibly fulfilled, she told me, "There's a sacred moment when the cross-clamp comes off, the heart is reperfused, and it starts beating on its own again. In that second, every ounce of exhaustion, every missed family dinner, it all just melts away. You've given someone a future." It is this profound sense of purpose, coupled with a compensation package that provides financial security and acknowledges the immense value of the role, that makes this one of the most sought-after and respected PA specialties.
This comprehensive guide is designed to be your definitive resource, whether you're a pre-health student dreaming of the operating room, a PA student planning your specialty, or a practicing PA considering a transition into the dynamic world of cardiac surgery. We will dissect every component of a cardiothoracic surgery physician assistant salary, explore the factors that drive your earning potential, and provide a clear, actionable roadmap to launching and advancing in this exceptional career.
### Table of Contents
- [What Does a Cardiothoracic Surgery Physician Assistant Do?](#what-does-a-cardiothoracic-surgery-physician-assistant-do)
- [Average Cardiothoracic Surgery Physician Assistant Salary: A Deep Dive](#average-cardiothoracic-surgery-physician-assistant-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
---
What Does a Cardiothoracic Surgery Physician Assistant Do?

A Cardiothoracic Surgery Physician Assistant (CT PA) is a highly specialized medical professional who works under the supervision of a cardiothoracic surgeon. However, the term "supervision" can be misleading. In reality, experienced CT PAs practice with a remarkable degree of autonomy, serving as a true extension of the surgeon. They are integral to the seamless delivery of patient care across the entire surgical continuum: before, during, and after a procedure. Their role is a demanding blend of clinical knowledge, technical surgical skill, and critical thinking under pressure.
The responsibilities of a CT PA are vast and can be broadly categorized into three domains:
1. Pre-Operative Patient Management: This involves preparing the patient for surgery. The PA is often the primary point of contact for the patient and their family, building rapport and trust during a vulnerable time.
- Conducting Comprehensive Work-Ups: Performing detailed patient histories and physical examinations.
- Ordering and Interpreting Diagnostics: Ordering tests such as ECGs, stress tests, echocardiograms, chest X-rays, and lab work, and interpreting the results to formulate a patient assessment.
- Patient Education: Thoroughly explaining the planned surgical procedure, risks, benefits, and alternatives to the patient and their family, and obtaining informed consent.
- Pre-operative Orders: Writing orders for medications, diet, and other pre-surgical preparations.
2. Intra-Operative First Assisting: This is the core surgical component of the role and where the CT PA's technical skills shine. They stand directly across from the surgeon at the operating table.
- Endoscopic Vein Harvesting (EVH): This is arguably the most critical and defining skill of a CT PA. The PA makes a small incision in the leg or arm and uses an endoscope to carefully dissect and remove a length of the saphenous vein or radial artery. This vessel is then used by the surgeon to create bypasses around blocked coronary arteries. An efficient and skilled PA can perform an EVH concurrently while the surgeon begins the sternotomy, saving precious time while the patient is on cardiopulmonary bypass.
- Surgical Assistance: Providing exposure by holding retractors, suctioning the surgical field, managing sutures, and anticipating the surgeon's every move.
- Surgical Tasks: Depending on their experience and the surgeon's confidence in them, PAs may cannulate for cardiopulmonary bypass, place chest tubes, insert pacing wires, and perform the initial stages of surgical closure.
- Robotic Surgery: In centers with robotic systems like the da Vinci Surgical System, PAs may assist at the bedside, changing instruments and ensuring the smooth operation of the robotic arms, or even train to operate a console.
3. Post-Operative Critical Care Management: The surgery itself is only half the battle. The PA plays a vital role in managing the patient's recovery, often from the moment they leave the OR through to their hospital discharge.
- ICU/Step-Down Care: Managing ventilators, titrating vasoactive drips (medications that control blood pressure), managing fluid and electrolyte balance, and monitoring for post-operative complications like bleeding or arrhythmias.
- Procedural Tasks: Removing chest tubes, epicardial pacing wires, and sutures/staples.
- Wound Care: Managing complex sternal and harvest-site incisions.
- Discharge Planning: Writing prescriptions, coordinating follow-up care, and educating the patient on their recovery process, medications, and activity limitations.
### A Day in the Life of a CT PA
To make this tangible, consider a typical (if there is such a thing) day:
- 5:30 AM: Arrive at the hospital. Begin "pre-rounding" on all post-operative patients in the Cardiovascular ICU and the step-down unit. Review overnight events, vital signs, lab results, and imaging for 5-15 patients.
- 7:00 AM: Round with the entire surgical team, including surgeons, residents, and nurses. Present each patient, discuss their progress, and formulate the plan of care for the day. Write daily progress notes and put in new orders.
- 8:00 AM: Head to the operating room for the first case: a Coronary Artery Bypass Graft (CABG). Greet the patient in the pre-op holding area, answer any last-minute questions, and confirm consent.
- 8:30 AM - 1:00 PM: In the OR. While the surgeon performs the median sternotomy, you are at the patient's leg, performing an endoscopic vein harvest. Once the vein is out and prepared, you scrub in and first-assist for the remainder of the complex surgery.
- 1:00 PM - 2:00 PM: The case finishes. You help close the chest, transport the patient to the ICU, and give a detailed sign-out to the ICU nurse. You might grab a quick lunch while writing the post-operative orders and the operative note.
- 2:00 PM - 5:00 PM: The afternoon is spent on the floor. You might remove a chest tube from a patient who is three days post-op, assess a patient with a new-onset arrhythmia, and perform a discharge consultation with a patient going home tomorrow. You also see new consults on the hospital floors.
- 5:00 PM - 6:30 PM: "Table round" with the team again to sign out the day's events to the PA or resident on call for the night. Finish any remaining patient notes and documentation.
- 6:30 PM (or later): Head home... unless you are the one on call for the night, in which case you might be called back in for an emergency aortic dissection.
This demanding schedule underscores why the cardiothoracic surgery physician assistant salary is among the highest in the profession. It requires a unique combination of stamina, intelligence, and fine motor skill, placing PAs at the center of life-saving medicine.
---
Average Cardiothoracic Surgery Physician Assistant Salary: A Deep Dive
The compensation for a Cardiothoracic Surgery PA is a direct reflection of the specialization's high stakes, extensive training, and demanding lifestyle. While a general PA salary is already competitive, specializing in a surgical subspecialty like cardiothoracic surgery provides a significant and well-deserved financial premium.
Let's break down the numbers based on the most reliable industry data. The primary source for PA salary information is the annual Salary Report published by the American Academy of Physician Associates (AAPA). This report surveys tens of thousands of PAs across all specialties and provides the most granular and authoritative data available.
### National Averages and Typical Ranges
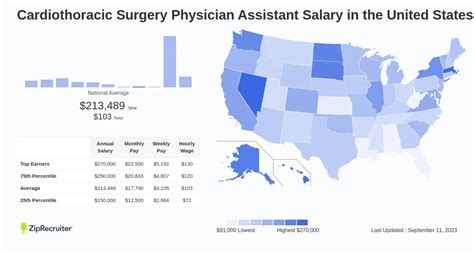
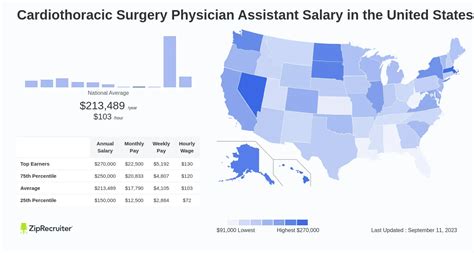
According to the 2023 AAPA Salary Report, the median total compensation for a Physician Assistant specializing in cardiothoracic and vascular surgery was $145,000. Total compensation is a critical figure because it includes not just the base salary but also any bonuses received throughout the year. The median base salary for this specialty was $136,000.
However, medians only tell part of the story. The salary range is vast, influenced by the many factors we will explore in the next section. A more realistic picture of the cardiothoracic surgery physician assistant salary spectrum looks like this:
- Entry-Level (0-2 years, often in a fellowship): $110,000 - $130,000
- Mid-Career (3-9 years, fully proficient): $135,000 - $175,000
- Senior/Experienced (10+ years, expert level): $175,000 - $220,000+
It's not uncommon for highly experienced PAs in high-demand locations, particularly those who take on significant call burdens or have productivity-based bonuses, to exceed these upper limits. Data from other reputable salary aggregators supports this. As of late 2023, Salary.com reports the average Cardiothoracic Surgery PA salary in the United States as $148,871, with a typical range falling between $132,159 and $164,198. These platforms often allow you to input your location and experience level for a more personalized estimate.
### Salary Progression by Experience Level
The salary growth trajectory for a CT PA is steep, especially in the first five years as they move from a novice assistant to a proficient and autonomous clinician.
| Experience Level | Typical Base Salary Range | Key Responsibilities & Skills |
| :--- | :--- | :--- |
| Entry-Level (0-2 Years) | $110,000 - $130,000 | Focus on learning fundamental skills. Heavy supervision. Mastering EVH, basic suturing, and post-op floor management. High learning curve. May include a post-graduate residency year at a lower salary ($80k-$90k). |
| Mid-Career (3-9 Years) | $135,000 - $175,000 | Fully autonomous in most roles. Highly proficient and efficient at EVH. Manages complex ICU patients independently. First-assists on a wide variety of cases (valves, dissections). Begins to train new PAs or students. |
| Senior-Level (10+ Years)| $175,000 - $220,000+ | Expert clinician and proceduralist. Often serves as Lead PA or Chief PA. Involved in program development (e.g., TAVR program). May have administrative duties. The "go-to" person for the most complex cases and patient issues. Negotiates a premium salary. |
### Beyond the Base: Deconstructing Total Compensation
A savvy professional never looks at base salary alone. In a field like CT surgery, the components of your total compensation package can add tens of thousands of dollars to your annual earnings.
- Base Salary: This is your guaranteed annual pay. It forms the foundation of your compensation but is often only 75-90% of your total take-home pay.
- Bonuses:
- Sign-On Bonus: To attract talent, especially for positions that are hard to fill, hospitals often offer a sign-on bonus ranging from $5,000 to $25,000+. This is often tied to a commitment to stay with the employer for a certain period (e.g., two years).
- Performance/Productivity Bonus: Some private groups or hospital systems may offer bonuses tied to the number of cases (RVUs - Relative Value Units) you participate in or overall department profitability. This can be a significant addition to your income.
- Annual Bonus: A discretionary bonus based on individual and hospital performance.
- Call Pay & Overtime: This is a huge factor. Surgical specialties require 24/7 coverage. Call is typically structured on a rotating basis (e.g., one night a week and one weekend a month). Compensation models vary widely:
- Hourly Pay for Call-Back: You receive your regular hourly rate (or time-and-a-half) for every hour you are physically in the hospital when called in.
- Call Stipend: A flat fee paid for each shift you are on call (e.g., $250 for a 24-hour weekend shift), plus hourly pay if you get called in.
- Inclusive Higher Salary: Some employers offer a higher base salary with the expectation that call is part of the job description, with no additional pay. It's crucial to clarify this during negotiations.
- Comprehensive Benefits Package: The value of a good benefits package cannot be overstated.
- Health Insurance: Medical, dental, and vision insurance for you and your family. Look for low-deductible, low-premium plans.
- Retirement Savings: A 401(k) or 403(b) plan. The employer match is free money. A common match is 50% of your contribution up to 6% of your salary. Over a career, this can amount to hundreds of thousands of dollars.
- Malpractice Insurance: The employer must provide this. The crucial detail is "tail coverage." This policy covers you for any claims made *after* you leave the job that relate to incidents that occurred *during* your employment. Without it, you would have to purchase an expensive policy yourself when you change jobs.
- Continuing Medical Education (CME) Allowance: PAs must complete 100 hours of CME every two years. Employers typically provide an allowance of $1,500 - $5,000 per year to cover the costs of conferences, textbooks, and subscriptions.
- Paid Time Off (PTO): This includes vacation, sick days, and holidays. Given the demanding nature of the job, a generous PTO package (e.g., 4-6 weeks) is essential for preventing burnout.
- Licensing and Dues: Many employers will pay for your state license renewal, DEA license, and membership dues for professional organizations like the AAPA or the Association of Physician Assistants in Cardiothoracic and Vascular Surgery (APACVS).
When evaluating a job offer, you must calculate the value of this entire package. An offer with a $140,000 base salary and an excellent benefits package with robust call pay could be far more lucrative than a $150,000 offer with poor benefits and unpaid call.
---
Key Factors That Influence Salary

The substantial range in a cardiothoracic surgery physician assistant salary isn't arbitrary. It's determined by a complex interplay of experience, skills, geography, and employer type. Understanding these levers is the key to maximizing your earning potential throughout your career. As an expert career analyst, I've seen professionals strategically leverage these factors to increase their income by tens of thousands of dollars.
### `
`Geographic Location: Where You Work Matters—A Lot
Geography is one of the most powerful drivers of salary. The demand for specialized PAs, combined with the local cost of living and the competitiveness of the healthcare market, creates significant salary disparities across the country.
- High-Paying States and Metropolitan Areas: Generally, areas with high population density, multiple competing hospital systems, and a high cost of living tend to offer the highest salaries. According to BLS and AAPA data, states like California, New York, Alaska, Washington, and Connecticut consistently rank among the top-paying states for PAs in general. Within these states, major metropolitan areas often pay a premium. A CT PA position in New York City, Los Angeles, or the San Francisco Bay Area can command a salary 15-30% higher than the national median. For example, a role that pays $150,000 in the Midwest might command $185,000 in Southern California.
- Cost of Living Adjustment: It's crucial to analyze salary in the context of cost of living. A $170,000 salary in Manhattan may provide a lower quality of life than a $140,000 salary in a city like Charlotte, NC, where the cost of housing, taxes, and daily expenses are significantly lower. Use online cost-of-living calculators to compare offers realistically.
- Rural vs. Urban and Regional Markets: Don't discount non-metropolitan areas. While major cities offer the highest nominal salaries, some rural or underserved areas, desperate for specialized talent, may offer surprisingly competitive packages. These can include not only a strong salary but also significant student loan repayment assistance (through state or federal programs like the National Health Service Corps), large sign-on bonuses, and relocation packages. The Southeast and Midwest, for instance, have a growing number of advanced cardiac centers and may offer a fantastic balance of high salary and low cost of living. A CT PA might earn $160,000 in a mid-sized Ohio city and live exceptionally well.
- Market Saturation: In areas with a high concentration of PA training programs, the supply of new graduates can sometimes depress entry-level wages. Conversely, a region with a growing elderly population and fewer specialized providers creates a high-demand, high-salary environment.
### `
`Years of Experience and Skill Mastery: The Provenance Premium
In a field as complex as cardiothoracic surgery, experience isn't just about time served; it's about the accumulation of skills, confidence, and efficiency. This is why the salary curve is so steep in the first decade of practice.
- The Novice to Expert Trajectory (Years 0-5): A new graduate is an investment for a surgical practice. The first 1-2 years are an intensive training period. The PA is learning to perform EVH efficiently, manage ICU patients, and function smoothly in the OR. Their salary reflects this trainee status. By years 3-5, the PA has become a reliable, autonomous, and productive member of the team. They can handle routine cases and post-operative care with minimal oversight. This leap in value and contribution is directly reflected in a significant salary jump.
- The Senior Clinician (Years 10+): After a decade, a CT PA is an expert. Their value is immense.
- Efficiency: A 10-year veteran can harvest a vein in a fraction of the time it takes a new grad, saving valuable OR time (which translates to money for the hospital).
- Problem Solving: They can manage the most complex and critically ill post-op patients, preventing costly complications and readmissions.
- Advanced Cases: They are trusted to first-assist on the most challenging procedures, such as aortic dissections, re-do sternotomies, or complex valve replacements.
- Mentorship: They are often responsible for training new PAs, residents, and students, adding value beyond their own clinical work.
This level of expertise allows them to negotiate top-tier salaries, often pushing well past the $200,000 mark, especially when combined with leadership responsibilities.
### `
`Type of Employer: The Impact of Practice Setting
The type of institution you work for has a profound impact on your salary structure, benefits, and overall work environment.
- Large Academic Medical Centers: These are university-affiliated hospitals.
- Salary: Base salaries may be slightly lower than in the private sector. They often have more rigid, tiered pay scales based on years of experience.
- Pros: Excellent benefits packages (pension plans, tuition remission for family members), a strong focus on education and research, and the prestige of working at a leading institution. You are exposed to cutting-edge technology and "zebras" (rare cases).
- Cons: Can be bureaucratic, with less flexibility in salary negotiation.
- Large Private Hospital Systems (Non-Academic): These are the large, often for-profit or non-profit, community-based health systems that dominate many regional markets.
- Salary: Often the highest payers in terms of base salary. They are run like businesses and are willing to pay top dollar to attract and retain the talent needed to drive their high-revenue service lines, like cardiac surgery.
- Pros: Highly competitive salaries, often with performance bonus potential.
- Cons: Can have a more corporate feel, with a strong focus on productivity metrics and patient throughput.
- Private Surgeon-Owned Groups: These are smaller groups of surgeons who employ their own PAs.
- Salary: The earning potential here can be extremely high. Compensation might be structured with a moderate base salary plus a significant productivity bonus tied directly to the group's profits.
- Pros: More autonomy, a close-knit team environment, and the potential for very high income if the practice is successful.
- Cons: Benefits packages may be less robust than at a large hospital. Job security is tied to the success of the practice. There is often less of a buffer—if a surgeon leaves, the group's dynamics and workload can change dramatically.
- Locum Tenens: Latin for "to hold the place of." Locum tenens PAs are temporary, independent contractors who fill in for staffing shortages, maternity leaves, or vacations.
- Salary: The pay is extremely high, often paid as a daily or hourly rate that can equate to an annualized salary of $200,000 - $250,000 or more. The agency also typically covers travel, housing, and malpractice insurance.
- Pros: Top-tier pay, flexibility to choose assignments, and the opportunity to experience different practice settings across the country.
- Cons: No benefits (no health insurance, no retirement plan, no PTO). You are responsible for your own taxes as a 1099 contractor. There is a lack of stability and a constant need to adapt to new teams, surgeons, and hospital systems.
### `
`Advanced Certifications and Training: Formalizing Your Expertise
While experience is paramount, formal credentials can validate your skills and enhance your negotiating power.
- CAQ in Cardiovascular and Thoracic Surgery: The most significant credential a CT PA can earn is the Certificate of Added Qualifications (CAQ) from the National Commission on Certification of Physician Assistants (NCCPA). To be eligible, a PA needs a PANCE certification, significant experience in the specialty (at least 4,000 hours), a physician attestation of their skills, and must pass a rigorous specialty exam.
- Impact on Salary: Holding a CAQ demonstrates a tested, high level of expertise. While it may not trigger an automatic raise, it makes you a far more competitive candidate for high-paying jobs and strengthens your position during salary negotiations. Some institutions, particularly academic centers, may offer a specific stipend or higher salary grade for CAQ holders. It signals to an employer that you are a career specialist, not just a transient in the field.
### `
`In-Demand Procedural and Clinical Skills: Your Value Proposition
In surgery, what you can *do* is what defines your value. Certain high-level skills will make you an indispensable asset and directly increase your earning potential.
- Endoscopic Vessel Harvesting (EVH & ERAH): As mentioned before,