Introduction

Are you driven by a desire to make a tangible difference in people's lives? Do you possess a unique blend of empathy, organization, and problem-solving skills? If you find yourself nodding along, a career as a Care Coordinator might be your calling. This role is more than just a job; it's the central nervous system of modern, patient-centric healthcare. Care Coordinators are the vital navigators who guide patients through the often-confusing labyrinth of medical appointments, insurance policies, and community resources, ensuring no one falls through the cracks. It's a profession built on advocacy, communication, and compassion, and it's one of the fastest-growing and most crucial roles in the healthcare landscape today.
But passion alone doesn't pay the bills. A critical question for anyone considering this path is: What is the real earning potential? The care coordinator salary is a key piece of the puzzle, and the good news is that it reflects the role's increasing importance. While salaries can vary widely based on numerous factors, the national median often falls between $50,000 and $65,000 per year. Entry-level positions may start in the $40,000s, but with experience, specialized credentials, and the right skills, senior Care Coordinators and those in management can earn upwards of $85,000 or more.
I once witnessed the profound impact of this role firsthand when a close family member was recovering from major surgery. The deluge of paperwork, conflicting appointment schedules, and confusing medication instructions was overwhelming for all of us. It was the hospital's Care Coordinator, a calm and incredibly organized professional named Maria, who became our lifeline. She was the human compass we desperately needed, translating medical jargon into plain English and orchestrating every detail of the post-discharge plan. It was in that moment I truly understood that Care Coordinators don't just manage cases; they restore order and hope during times of chaos.
This comprehensive guide is designed to be your definitive resource for understanding everything about the Care Coordinator salary and career path. We will delve deep into national averages, dissect the key factors that influence your pay, explore the promising job outlook, and provide a step-by-step roadmap to help you launch and advance your career.
### Table of Contents
- [What Does a Care Coordinator Do?](#what-is-a-care-coordinator)
- [Average Care Coordinator Salary: A Deep Dive](#average-salary)
- [Key Factors That Influence Your Salary](#key-factors)
- [Job Outlook and Career Growth](#job-outlook)
- [How to Get Started in This Career](#how-to-get-started)
- [Conclusion: Is a Career as a Care Coordinator Right for You?](#conclusion)
---
What Does a Care Coordinator Do?

At its core, a Care Coordinator acts as the central point of contact and chief advocate for a patient. They are the "quarterbacks" of a patient's care team, ensuring that all parties—including doctors, specialists, nurses, therapists, insurance providers, and community service agencies—are communicating and working together seamlessly toward a common goal: the patient's well-being. This role is particularly vital for patients with complex or chronic conditions, the elderly, or those facing significant social or economic barriers to health.
The primary mission of a Care Coordinator is to create, implement, and monitor a comprehensive care plan tailored to the individual needs of the patient. This involves breaking down silos between different healthcare providers and services to create a holistic, continuous, and efficient care experience.
Core Responsibilities and Daily Tasks:
The day-to-day work of a Care Coordinator is dynamic and multifaceted. Key responsibilities typically include:
- Patient Assessment: Conducting initial interviews and assessments with patients and their families to understand their medical history, current health status, social support systems, financial situation, and personal goals.
- Care Planning: Collaborating with physicians, nurses, and other healthcare professionals to develop a personalized, actionable care plan. This plan outlines specific health goals, necessary treatments, appointments, medications, and required support services.
- Coordination and Scheduling: Arranging appointments with specialists, scheduling diagnostic tests, and coordinating hospital admissions or discharges. They ensure that medical records and test results are transferred between facilities in a timely manner.
- Patient and Family Education: Explaining diagnoses, treatment options, and medication regimens in clear, understandable terms. They empower patients and their families to take an active role in their own healthcare management.
- Resource Navigation: Connecting patients with essential community resources, such as transportation services, meal delivery programs, financial assistance, support groups, and home health aides.
- Advocacy and Insurance Liaison: Acting as the patient's advocate, especially when dealing with insurance companies. They may help with prior authorizations, appeal claim denials, and help patients understand their coverage and out-of-pocket costs.
- Monitoring and Follow-Up: Regularly checking in with patients to monitor their progress, assess the effectiveness of the care plan, and make necessary adjustments. This follow-up is crucial for preventing hospital readmissions and managing chronic conditions.
- Documentation: Meticulously documenting all interactions, assessments, plans, and outcomes in the patient's Electronic Health Record (EHR) or case management system.
### A Day in the Life: "Elena," a Hospital-Based Care Coordinator
To make this role more tangible, let's follow a day in the life of Elena, a Care Coordinator working in a large urban hospital.
- 8:00 AM - Morning Huddle & Chart Review: Elena starts her day by attending a multidisciplinary team meeting on the cardiology floor. She discusses the status of her current patients with doctors, nurses, and physical therapists. They identify two patients who are potentially ready for discharge in the next 48 hours.
- 9:00 AM - Patient Assessment: Elena meets with Mr. Chen, a 72-year-old man recovering from a mild stroke. She assesses his home environment through conversation with his daughter, learning that he lives alone in a two-story house. She identifies potential needs: physical therapy, a home safety evaluation, and a medication dispenser to manage his new prescriptions.
- 10:30 AM - Coordination & Phone Calls: Elena spends the next two hours on the phone and her computer. She schedules a follow-up appointment for Mr. Chen with his primary care physician and a neurologist. She contacts his insurance provider to get pre-authorization for in-home physical therapy and submits the necessary clinical documentation.
- 12:30 PM - Lunch & Documentation: Elena catches a quick lunch while catching up on her documentation, carefully noting her conversations and the actions taken for each patient in the hospital's EHR system.
- 1:30 PM - Discharge Planning: She meets with Mrs. Davis, an 85-year-old patient being discharged after a hip replacement. Elena goes over the discharge instructions with Mrs. Davis and her son, explaining the medication schedule in simple terms. She confirms that a hospital bed and walker have been delivered to the home by a medical supply company and that a visiting nurse is scheduled for the next day.
- 3:00 PM - Crisis Intervention: A social worker alerts Elena to a patient whose insurance has unexpectedly denied coverage for a critical, expensive medication. Elena immediately gets on the phone with the insurance case manager, advocating fiercely for her patient. She gathers additional medical necessity documentation from the attending physician and files an expedited appeal.
- 4:30 PM - Final Follow-Ups: Before leaving, Elena makes a follow-up call to a patient who was discharged last week, checking to see if they are taking their medications correctly and have made it to their follow-up appointments. She documents the call and plans her priorities for the next day.
This snapshot reveals the essence of the job: a constant blend of structured planning, proactive problem-solving, and empathetic human connection.
---
Average Care Coordinator Salary: A Deep Dive

Understanding the financial landscape of a career is essential. While the drive to help others is a primary motivator for many Care Coordinators, competitive compensation ensures that it is a sustainable and rewarding long-term profession. The salary for a Care Coordinator is not a single, fixed number but rather a spectrum influenced by the factors we will explore in the next section. However, by examining data from authoritative sources, we can establish a clear and reliable picture of the typical earnings.
According to recent data from leading salary aggregators, the national median salary for a Care Coordinator in the United States generally falls within the $50,000 to $65,000 range.
- Salary.com reports a median salary for a Care Coordinator of $62,684 as of late 2023, with the typical range falling between $55,420 and $70,256.
- Payscale provides a slightly lower average base salary figure, around $51,150 per year, but shows that the total pay (including bonuses and other compensation) can extend up to $74,000 for the top 10% of earners.
- Glassdoor estimates a total pay average of approximately $58,743 per year, combining a base salary of around $51,000 with additional pay like cash bonuses and tips averaging over $7,000.
- The U.S. Bureau of Labor Statistics (BLS) does not have a distinct category for "Care Coordinator." However, the role often overlaps with two major categories: Social and Human Service Assistants and Medical and Health Services Managers.
- Social and Human Service Assistants, which represents many entry-level or non-clinical coordinator roles, had a median pay of $38,520 per year in May 2022. This often reflects roles in non-profit or community settings.
- Medical and Health Services Managers, a category that senior Care Coordinators or those with clinical licenses (like an RN) and managerial duties may fall into, shows a significantly higher median pay of $104,830 per year.
This disparity in BLS data highlights a crucial point: your specific background, credentials (e.g., being a Registered Nurse), and level of responsibility dramatically impact your place within the salary spectrum. A non-clinical coordinator at a community non-profit will earn closer to the Social and Human Service Assistant figure, while an RN Care Coordinator managing complex cases in a large hospital system will earn a salary that trends toward the Medical and Health Services Manager figure.
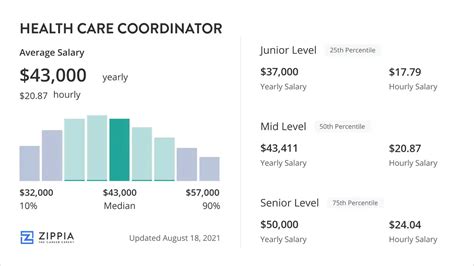
### Care Coordinator Salary by Experience Level
Experience is arguably the single most significant determinant of your salary. As you gain expertise, develop a track record of successful patient outcomes, and take on more complex cases, your value to an employer increases substantially.
Here is a typical salary progression you can expect throughout your career, based on aggregated data from Payscale and Salary.com:
| Experience Level | Years of Experience | Typical Annual Salary Range | Key Characteristics of the Role |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $40,000 - $52,000 | Learning core processes, managing less complex cases, heavy focus on scheduling and basic patient communication, working under close supervision. |
| Mid-Career | 3-7 Years | $52,000 - $68,000 | Handling a full caseload of moderately complex patients, working more autonomously, contributing to care plan development, starting to mentor new staff. |
| Senior/Experienced | 8-15 Years | $65,000 - $80,000+ | Managing highly complex cases (e.g., multi-system diseases), leading quality improvement initiatives, acting as a subject matter expert, training junior coordinators. |
| Lead/Managerial | 15+ Years | $75,000 - $95,000+ | Supervising a team of care coordinators, developing departmental policies and procedures, managing budgets, liaising with senior hospital administration. |
### Beyond the Base Salary: Understanding Total Compensation
Your annual salary is only one part of your overall earnings. A comprehensive compensation package for a Care Coordinator, especially one working for a hospital or large healthcare organization, often includes valuable additional components. When evaluating a job offer, it's critical to look at the "total compensation" picture.
- Bonuses: Some organizations offer annual performance-based bonuses. These might be tied to individual metrics (like reducing hospital readmission rates for your patient panel) or departmental/organizational performance. These can range from a few hundred to several thousand dollars.
- Profit Sharing: While less common in non-profit or government settings, some for-profit healthcare systems may offer profit-sharing plans, distributing a portion of the company's profits to employees.
- Health and Wellness Benefits: This is a significant part of compensation in the healthcare industry. Look for high-quality medical, dental, and vision insurance plans with low premiums and deductibles. Many employers also offer wellness programs, gym memberships, and mental health support.
- Retirement Savings Plans: A strong retirement plan, such as a 401(k) or 403(b) (for non-profits), is a crucial long-term benefit. Pay close attention to the employer match—a company that matches your contributions up to a certain percentage is essentially giving you free money.
- Paid Time Off (PTO): This includes vacation days, sick leave, and personal days. A generous PTO policy is a valuable component of work-life balance.
- Professional Development and Tuition Reimbursement: Many forward-thinking employers will invest in your growth by offering a stipend for continuing education, paying for certification exams (like the CCM), or providing tuition reimbursement for pursuing a higher degree (like a BSN or MSW). This is a benefit that pays dividends throughout your career.
- Life and Disability Insurance: Employer-sponsored short-term disability (STD), long-term disability (LTD), and life insurance policies provide a crucial financial safety net for you and your family.
When comparing job offers, calculate the approximate value of these benefits to understand the true worth of each compensation package. An offer with a slightly lower base salary but a phenomenal benefits package might be the better long-term choice.
---
Key Factors That Influence Your Salary
While the national averages provide a useful baseline, your individual salary as a Care Coordinator will be determined by a specific combination of factors. Understanding these variables is the key to maximizing your earning potential. This section breaks down the six most influential elements that shape your paycheck.
### 1. Level of Education and Clinical Licensure
Your educational background and professional credentials are the foundation of your career and a primary driver of salary.
- Associate's Degree: An Associate's degree in a field like human services or medical assisting can be a starting point for entry-level Care Coordinator or patient navigator roles, often in community health or social service settings. Salaries for these positions typically fall at the lower end of the spectrum, around $40,000 to $48,000.
- Bachelor's Degree: A Bachelor's degree is the most common educational requirement and significantly increases earning potential. Degrees in Social Work (BSW), Nursing (BSN), Public Health, Psychology, or a related healthcare field are highly valued. A Care Coordinator with a Bachelor's degree can expect to start in the $48,000 to $60,000 range, depending on other factors.
- Clinical Licensure (RN, LPN, LCSW): This is a major salary differentiator. A Registered Nurse (RN) who becomes a Care Coordinator commands a much higher salary due to their clinical assessment skills and deep medical knowledge. An RN Care Coordinator's salary often starts in the $65,000 to $75,000 range and can easily exceed $90,000 with experience. Similarly, a Licensed Clinical Social Worker (LCSW) brings advanced skills in psychosocial assessment and counseling, also commanding a premium salary.
- Master's Degree: Pursuing a Master's degree in Social Work (MSW), Nursing (MSN), Healthcare Administration (MHA), or Public Health (MPH) opens the door to senior, specialized, and leadership positions. Professionals with a Master's degree often work in program management, policy development, or department leadership, with salaries frequently ranging from $75,000 to over $100,000, aligning with the BLS data for Medical and Health Services Managers.
### 2. Years of Professional Experience
As detailed in the previous section, experience is paramount. However, it's not just the number of years but the *quality* of that experience that matters.
- 0-2 Years (Entry-Level): Focus is on learning systems, building foundational skills, and handling administrative tasks. Salary is at the base level as you are primarily in a learning and support role.
- 3-7 Years (Mid-Career): You have proven your ability to manage a caseload independently. Your salary increases as you demonstrate efficiency, positive patient outcomes, and a deep understanding of the healthcare ecosystem. You are a reliable and productive member of the team. At this stage, salaries typically see a 20-30% increase from entry-level.
- 8+ Years (Senior/Lead): You are now a subject matter expert. You handle the most complex and challenging cases, mentor new hires, and contribute to departmental strategy. Your expertise in navigating difficult insurance appeals or finding obscure community resources is highly valuable. Senior roles can command salaries 40-60% higher than entry-level positions. This is also the stage where you might transition into a formal leadership role, supervising a team of coordinators and taking on administrative responsibilities, which comes with another significant salary bump.
### 3. Geographic Location
Where you work has a massive impact on your salary. Compensation is often adjusted to reflect the local cost of living and the demand for healthcare professionals in a specific region. High-cost-of-living urban centers on the coasts typically offer the highest salaries, while rural areas and states with a lower cost of living offer less.
Top-Paying Metropolitan Areas for Related Professions (from BLS):
While specific data for "Care Coordinator" is sparse, looking at BLS data for "Medical and Health Services Managers" provides a strong indicator of high-paying regions:
1. San Jose-Sunnyvale-Santa Clara, CA
2. San Francisco-Oakland-Hayward, CA
3. Vallejo-Fairfield, CA
4. New York-Newark-Jersey City, NY-NJ-PA
5. Washington-Arlington-Alexandria, DC-VA-MD-WV
Salary Comparison by City (Illustrative Example):
| City | Cost of Living Index (US Avg = 100) | Typical Median Salary for a Care Coordinator |
| :--- | :--- | :--- |
| San Francisco, CA | 244 | ~$75,000 - $85,000+ |
| New York, NY | 180 | ~$70,000 - $80,000 |
| Boston, MA | 153 | ~$65,000 - $75,000 |
| Chicago, IL | 105 | ~$58,000 - $68,000 |
| Atlanta, GA | 100 | ~$55,000 - $65,000 |
| Dallas, TX | 101 | ~$54,000 - $64,000 |
| Kansas City, MO | 89 | ~$50,000 - $60,000 |
| Birmingham, AL | 76 | ~$48,000 - $58,000 |
*Source: Salary data is an aggregation of Payscale and Salary.com city-specific data. Cost of living index from Payscale.*
It's crucial to weigh the higher salary against the higher cost of living. A $75,000 salary in San Francisco may afford a similar or even lower quality of life than a $60,000 salary in Kansas City.
### 4. Work Setting: Company Type & Size
The type of organization you work for plays a significant role in compensation structure and overall benefits.
- Large Hospital Systems: These are often the highest-paying employers. They have larger budgets, more complex patient populations (requiring specialized coordinators), and structured salary bands. They also tend to offer the most robust benefits packages, including excellent health insurance and retirement plans.
- Private Clinics and Physician Groups: Salaries here can be competitive but may be slightly lower than in large hospitals. The work environment is often smaller and more intimate. Benefits packages can be more variable.
- Insurance Companies (Managed Care Organizations): Payers hire Care Coordinators (often called Case Managers) to manage the health of their members, especially those with high-cost chronic conditions. These roles are often remote or office-based rather than patient-facing. Salaries are very competitive, often rivaling or exceeding those in hospitals, as the work has a direct impact on the company's bottom line by preventing costly hospitalizations.
- Non-Profit and Community Health Organizations: These organizations are mission-driven and provide essential services to underserved populations. While incredibly rewarding, they typically operate on tighter budgets, which often translates to lower base salaries compared to for-profit entities. However, they may offer other benefits like strong work-life balance, a collaborative culture, and eligibility for programs like Public Service Loan Forgiveness (PSLF).
- Government Agencies (e.g., VA, Public Health Depts.): Government roles, such as those at the Department of Veterans Affairs (VA), offer competitive salaries with highly structured pay scales (like the GS scale). The main draw is exceptional job security and outstanding federal benefits, including a pension plan, which is rare in the private sector.
### 5. Area of Specialization
Just as doctors specialize, so too can Care Coordinators. Developing expertise in a specific, high-demand area can significantly boost your value and your salary.
- Oncology: Navigating cancer care is incredibly complex. Oncology Care Coordinators who understand chemotherapy cycles, radiation schedules, and supportive care needs are in high demand and can command higher salaries.
- Geriatrics: With the aging baby boomer population, expertise in geriatric care, including dementia, palliative care, and end-of-life planning, is extremely valuable.
- Pediatrics: Coordinating care for children with chronic or complex conditions requires a special skill set, including working closely with families, schools, and various pediatric specialists.
- Mental Health and Substance Abuse: These are high-need areas with a growing focus on integrated care. Coordinators who can navigate both the medical and behavioral health systems are critical and well-compensated.
- Transplant Coordination: This is a highly specialized, high-stakes field that involves managing every aspect of the organ transplant process for both donors and recipients. It's one of the highest-paying specializations due to the level of detail and responsibility required.
### 6. In-Demand Skills and Certifications
Beyond your degree and experience, specific, demonstrable skills can make you a more attractive candidate and give you leverage in salary negotiations.
High-Value Hard Skills:
- EHR/EMR Proficiency: Expertise in major Electronic Health Record systems like Epic, Cerner, or Allscripts is non-negotiable in most settings. Being a "super-user" is a major plus.
- Case Management Software: Familiarity with dedicated case management platforms (e.g., ZeOmega, Caspio).
- Data Analysis: The ability to track and analyze patient data to identify trends, measure outcomes (like readmission rates), and report on program effectiveness is increasingly important.
- Bilingualism: In diverse communities, fluency in a second language (especially Spanish) is a massive asset and can come with a salary differential or stipend.
- Medical Billing and Coding Knowledge: Understanding CPT, ICD-10, and insurance authorization processes gives you a significant advantage.
Impactful Certifications:
- Certified Case Manager (CCM): Offered by the Commission for Case Manager Certification (CCMC), the CCM is the gold standard credential for case managers and care coordinators. It demonstrates a high level of competence and adherence to professional standards. Earning your CCM often leads to a significant salary increase and is a requirement for many higher-level positions.
- Care Coordination and Transition Management (RN-BC): Offered by the American Nurses Credentialing Center (ANCC), this board certification is specifically for Registered Nurses working in care coordination. It validates an RN's expertise in this specialty.
- Accredited Case Manager (ACM): Offered by the American Case Management Association (ACMA), this is another highly respected credential, particularly for those working in hospital settings.
---
Job Outlook and Career Growth

For those investing their time, money, and energy into a career, long-term viability is a top