Introduction

Choosing to become a doctor is more than a career decision; it's a profound commitment to a life of service, continuous learning, and immense responsibility. For those drawn to the vibrant, demanding, and endlessly rewarding landscape of New York, the path is even more unique. You're not just considering a profession; you're contemplating joining an elite echelon of medical professionals at the epicenter of global innovation, culture, and finance. But alongside the noble aspirations and intellectual challenges lies a practical, crucial question: What is the financial reality of this path? What can you realistically expect for a doctor salary in NY?
The answer is complex and encouraging. While the journey is long and expensive, the financial rewards for physicians in New York are substantial, reflecting the high cost of living and the immense value they provide. The average salary for a physician in New York hovers around $280,000 to $350,000 per year, but this figure is merely a starting point. Depending on your specialty, location within the state, and years of experience, this number can climb well over $500,000 or even $700,000 annually.
I once had a conversation with a third-year surgical resident after she had just completed a grueling 28-hour shift at a major trauma center in the Bronx. Despite her visible exhaustion, her eyes lit up when she spoke about a complex procedure that saved a patient's life. "The salary will be a relief," she admitted, "but this feeling—knowing you were the last line of defense for someone—that's the real compensation." That conversation perfectly encapsulates the duality of a medical career in New York: it demands everything from you, but the returns, both tangible and intangible, are extraordinary.
This guide is designed to be your definitive resource, providing a transparent, data-driven, and comprehensive look into every facet of a physician's salary and career in the Empire State. We will dissect the numbers, explore the influencing factors, map out the career trajectory, and provide you with an actionable roadmap to get started.
### Table of Contents
- [What Does a Doctor in New York Do?](#what-does-a-doctor-in-new-york-do)
- [Average Doctor Salary in NY: A Deep Dive](#average-doctor-salary-in-ny-a-deep-dive)
- [Key Factors That Influence a Doctor's Salary in NY](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Doctors in NY](#job-outlook-and-career-growth)
- [How to Become a Doctor in New York: A Step-by-Step Guide](#how-to-get-started-in-this-career)
- [Conclusion: Is a Medical Career in New York Right for You?](#conclusion)
---
What Does a Doctor in New York Do?
At its core, the role of a doctor, formally known as a physician, is to diagnose and treat human diseases, injuries, and other physical and mental impairments. They are stewards of health, guiding patients from prevention and diagnosis through treatment and recovery. However, being a doctor in New York adds unique layers of complexity, pace, and diversity to this fundamental mission. The state's vast and varied population—from the dense, multicultural boroughs of New York City to the rural communities upstate—means a physician's work is incredibly dynamic.
The foundational responsibilities remain consistent across all specialties and locations:
- Patient Examination and History: Conducting thorough physical examinations and taking detailed medical histories to understand a patient's health concerns.
- Diagnosis: Ordering, performing, and interpreting diagnostic tests (e.g., blood work, X-rays, MRIs) to identify the nature of a disease or injury.
- Treatment Planning: Developing and prescribing treatment plans, which can include medication, surgery, therapy, or lifestyle changes.
- Counseling: Educating patients and their families about their conditions, treatment options, and preventative health measures.
- Collaboration: Working as part of a multidisciplinary team, consulting with other physicians, surgeons, nurses, and healthcare professionals to ensure comprehensive patient care.
- Record-Keeping: Meticulously documenting patient encounters, diagnoses, treatments, and outcomes in Electronic Health Records (EHRs).
- Continuous Learning: Staying abreast of the latest medical research, treatments, and technologies through continuing medical education (CME).
Beyond these core duties, the "New York factor" introduces specific demands. A doctor in a bustling NYC hospital might face a higher volume of trauma cases, rare infectious diseases from a global travel hub, and the challenges of communicating with a diverse, multilingual patient base. Conversely, a primary care physician in a smaller upstate town might be the sole healthcare provider for a wide geographic area, requiring a broader knowledge base and a deep understanding of community health issues.
### A Day in the Life: An NYC Emergency Medicine Physician
To make this tangible, let's walk through a hypothetical day for an attending Emergency Medicine (EM) physician at a large hospital in Manhattan.
- 6:30 AM - Arrival and Sign-Out: The day begins by taking "sign-out" from the overnight physician. This is a critical handover of all current patients in the Emergency Department (ED). They discuss critical cases, pending lab results, and potential admissions.
- 7:00 AM - 11:00 AM - The First Rush: The morning rush begins. The physician moves between patient rooms, assessing a wide array of cases: a tourist with chest pain, a construction worker with a fractured limb, a child with a high fever, and an elderly patient with signs of a stroke. They are simultaneously ordering tests, interpreting EKGs, consulting specialists (Cardiology, Neurology), and directing the nursing and resident teams.
- 11:00 AM - 1:00 PM - Trauma and Critical Care: A "Level 1 Trauma" alert blares. A multi-vehicle accident on the FDR Drive brings in several severely injured patients. The EM physician leads the trauma team, performing a rapid assessment (the "primary survey"), ordering immediate imaging, and making split-second decisions to stabilize the most critical patient for the operating room.
- 1:00 PM - 2:00 PM - Documentation and Follow-Up: A brief lull allows the physician to catch up on charting in the EHR system—a crucial but time-consuming task. They also follow up on lab results for patients seen earlier and coordinate hospital admissions with internists.
- 2:00 PM - 5:30 PM - Managing Flow: The afternoon brings a new wave of patients. The physician focuses on managing the overall flow of the ED, deciding who can be safely discharged, who needs to be admitted, and who requires further observation. They might perform procedures like suturing a complex laceration or reducing a dislocated shoulder.
- 5:30 PM - 6:30 PM - Winding Down and Sign-Out: The physician prepares a detailed sign-out for the incoming evening shift physician, ensuring a safe and seamless transition of care for all patients remaining in the department. Before leaving, they do one last round on their most critical patients.
This day illustrates the high-stakes, fast-paced, and intellectually stimulating environment that defines much of the medical profession in New York. It's a role that requires not just medical expertise, but also exceptional resilience, communication skills, and the ability to lead under pressure.
---
Average Doctor Salary in NY: A Deep Dive
Analyzing physician compensation is complex, as "average salary" can be misleading. Averages are heavily skewed by specialty, location, and practice type. However, by examining data from multiple authoritative sources, we can construct a detailed and reliable picture of what doctors earn in New York.
It's crucial to first distinguish between resident salaries and attending physician salaries. Residents are physicians in training who have graduated from medical school but are not yet board-certified in a specialty. Their salaries are modest and often standardized within a hospital system. Attending physicians have completed all training and are fully licensed and credentialed. Their salaries are significantly higher and more variable. This section will focus on attending physicians.
### New York vs. National Averages
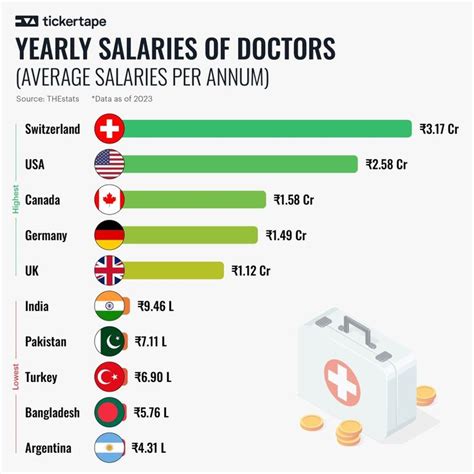
Nationally, physician compensation is robust. The Medscape Physician Compensation Report 2023, a widely respected industry benchmark, found the average overall physician salary in the United States to be $352,000. This includes both primary care physicians (PCPs) at $265,000 and specialists at $382,000.
How does New York stack up? Data consistently shows that New York physician salaries are competitive, often slightly above the national average, especially when accounting for the state's high cost of living.
- The U.S. Bureau of Labor Statistics (BLS) Occupational Employment and Wage Statistics (OEWS) program provides some of the most reliable government data. As of May 2023, the mean annual wage for "Physicians and Surgeons, All Other" in New York State was $280,020. However, the BLS often has a wage ceiling in its public data, reporting top-end salaries as "$239,200+". This means the actual average is likely much higher, as confirmed by other sources.
- Doximity's 2023 Physician Compensation Report, which surveys over 190,000 U.S. physicians, provides more granular insight. While it doesn't always break out state-level averages, its regional data places the Northeast in a competitive bracket. For example, it ranks the New York City metropolitan area as #13 in the country for highest average physician compensation.
- Commercial salary aggregators paint a more current and often higher picture. According to Salary.com (data retrieved in 2024), the average physician salary in New York City is $259,578, but this is for a general "Physician - Generalist," and the typical range falls between $225,274 and $299,634. For a specialist like a Cardiologist in NYC, the average jumps to $485,307.
Key Takeaway: A conservative baseline for an average attending physician salary in New York is around $280,000, but this figure is heavily weighted by primary care roles. For specialists in high-demand fields, the average is closer to $400,000 - $500,000.
### Salary by Experience Level
A physician's earning potential grows significantly with experience. The journey from a newly minted attending to a senior partner or department head is marked by substantial salary increases.
| Experience Level | Typical Years Post-Residency | Estimated Annual Salary Range (NY) | Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level Attending | 0-3 Years | $200,000 - $300,000 | Initial salary after completing residency/fellowship. Often lower in academic settings, higher in private practice. |
| Mid-Career Physician | 4-10 Years | $280,000 - $450,000 | Established patient panel, increased procedural efficiency, and potential for partnership track in private groups. |
| Senior/Experienced Physician | 10+ Years | $350,000 - $600,000+ | Peak earning years. May include income from partnership, medical directorships, or other administrative roles. |
| Late Career/Pre-Retirement | 25+ Years | $300,000 - $550,000+ | May see a slight dip if physicians reduce hours, but highly experienced surgeons/specialists can maintain peak earnings. |
*Data compiled and estimated from Salary.com, Medscape reports, and Doximity data.*
### Beyond the Base Salary: Understanding Total Compensation
A doctor's salary is only one piece of their total compensation package, which is often very generous. When evaluating a job offer, it's critical to look at the entire picture.
- Bonuses: This is a significant component of physician pay. Bonuses are typically tied to productivity, measured by Relative Value Units (RVUs), patient volume, or quality metrics. An annual bonus can range from $20,000 to over $100,000. The Medscape report found that the average incentive bonus for physicians was around $41,000.
- Profit-Sharing and Partnership: In private practice, physicians may have the opportunity to become a partner after a few years. This means they buy into the practice and receive a share of the profits, which can dramatically increase total income.
- Retirement Plans: Employers typically offer robust retirement plans, such as a 401(k) or 403(b), often with a generous employer match (e.g., 5-10% of salary).
- Health Insurance: Comprehensive health, dental, and vision insurance for the physician and their family is standard.
- Malpractice Insurance: This is a crucial and expensive benefit. Employers typically cover the full cost of malpractice ("claims-made" or "occurrence-based") insurance, which can be worth tens of thousands of dollars per year, especially for high-risk specialties in New York.
- Continuing Medical Education (CME) Stipend: A yearly allowance (e.g., $3,000 - $7,000) to cover the costs of attending conferences, subscribing to journals, and fulfilling CME requirements for licensure.
- Paid Time Off (PTO): Usually includes 4-6 weeks of vacation time, plus additional time for sick leave and CME.
- Relocation Assistance: A sign-on bonus or relocation package (often $10,000 - $25,000) is common, especially for hospitals trying to recruit talent from out of state.
- Loan Repayment Programs: Some non-profit hospitals and clinics in underserved areas (including parts of NYC and rural upstate) may offer student loan repayment assistance as a powerful recruitment incentive.
When all these elements are combined, the total compensation package for a New York physician is often 20-30% higher than their base salary alone.
---
Key Factors That Influence a Doctor's Salary in NY
The "average" salary figures we've discussed are a starting point. In reality, a physician's income is determined by a confluence of powerful factors. Understanding these variables is key to maximizing your earning potential and making informed career choices. This is the most critical section for understanding the nuances of the doctor salary in NY.
### 1. Area of Specialization
This is, by far, the single most significant factor determining a physician's salary. The gap between primary care and procedural specialties is vast. This disparity is largely driven by the fee-for-service reimbursement model, where procedures (surgeries, imaging interpretations, invasive tests) are compensated at a much higher rate than cognitive work (patient consultations, chronic disease management).
Here is a breakdown of estimated average annual salaries for various specialties in the New York metropolitan area, demonstrating the wide range.
Top-Tier Earning Specialties (Procedural/Surgical):
| Specialty | Estimated Average NY Metro Salary | Notes |
| :--- | :--- | :--- |
| Neurosurgery | $750,000 - $1,000,000+ | Consistently one of the highest-paid specialties due to the complexity and risk of procedures. |
| Orthopedic Surgery | $600,000 - $850,000+ | High volume of lucrative procedures like joint replacements. Sub-specialties like spine surgery can earn even more. |
| Cardiology (Invasive/Interventional) | $550,000 - $800,000+ | Performing procedures like stenting and catheterizations drives high compensation. Non-invasive cardiologists earn less. |
| Plastic Surgery | $500,000 - $750,000+ | High earning potential, especially for those with a strong cosmetic/private pay practice. |
| Gastroenterology | $500,000 - $700,000 | High volume of procedures like colonoscopies and endoscopies leads to high productivity and income. |
| Urology | $480,000 - $650,000 | A blend of surgical procedures and clinical practice. |
High-Earning Specialties (Diagnostic/Hospital-Based):
| Specialty | Estimated Average NY Metro Salary | Notes |
| :--- | :--- | :--- |
| Radiology | $450,000 - $600,000 | High demand for interpreting complex imaging (MRI, CT). Teleradiology offers flexible work models. |
| Anesthesiology | $440,000 - $580,000 | Critical role in all surgeries. Compensation is stable and high. |
| Dermatology | $430,000 - $550,000 | Favorable lifestyle and a mix of medical, surgical, and cosmetic procedures. |
| Emergency Medicine | $350,000 - $450,000 | High-stress, shift-based work. Pay is strong but burnout can be a factor. |
Primary Care and Cognitive Specialties:
| Specialty | Estimated Average NY Metro Salary | Notes |
| :--- | :--- | :--- |
| Internal Medicine (Outpatient) | $260,000 - $320,000 | The foundation of adult healthcare. Compensation is rising due to demand but lags behind procedural fields. |
| Family Medicine | $250,000 - $310,000 | Broad-spectrum care for all ages. Faces similar compensation challenges as Internal Medicine. |
| Pediatrics | $240,000 - $290,000 | Generally the lowest-paid major specialty, driven by lower reimbursement rates for pediatric care. |
| Neurology | $280,000 - $350,000 | Cognitive-focused specialty, but demand is growing rapidly due to the aging population. |
| Psychiatry | $280,000 - $360,000 | Soaring demand and a shortage of providers have significantly increased compensation in recent years. |
*Sources: Data synthesized and estimated from Doximity 2023 Report, Medscape 2023 Report, and Salary.com specialty data for NYC.*
### 2. Geographic Location Within New York State
New York is not a monolith. The economic landscape of Manhattan is worlds apart from that of Buffalo or the Adirondacks. Physician salaries reflect these regional differences in cost of living, demand, and market competition.
- New York City (Manhattan, Brooklyn, Queens, Bronx, Staten Island): NYC and its immediate suburbs (Long Island, Westchester) generally offer the highest absolute salaries. The Doximity report consistently ranks the NYC metro area high for compensation. However, this is offset by an exceptionally high cost of living and intense market competition. A $400,000 salary in Manhattan might have less purchasing power than a $350,000 salary in a smaller city.
- Upstate Metropolitan Areas (Albany, Buffalo, Rochester, Syracuse): These cities offer a compelling value proposition. Salaries are often only slightly lower than in the NYC metro area, but the cost of living is dramatically less. For example, a specialist earning $450,000 in Buffalo likely has a much higher quality of life from a financial perspective than a colleague earning $500,000 in NYC. Health systems in these cities are actively recruiting and often offer competitive packages.
- Rural and Underserved Areas: To attract physicians to more remote parts of the state (e.g., the North Country, parts of the Southern Tier), hospitals and clinics must offer significant financial incentives. These can include higher base salaries, substantial sign-on bonuses, and generous student loan repayment programs. While the amenities may be fewer, the financial rewards and sense of community can be significant.
Salary Comparison: Family Medicine Physician
| Location | Estimated Average Salary | Key Considerations |
| :--- | :--- | :--- |
| Manhattan, NYC | $275,000 | Extremely high cost of living, high competition, diverse patient base. |
| Albany, NY | $255,000 | Lower cost of living, stable government/tech economy, good quality of life. |
| Buffalo, NY | $250,000 | Very low cost of living, resurgent economy, major academic medical centers. |
| Rural North Country| $285,000+ | Potentially higher salary, plus loan repayment. Slower pace of life, fewer amenities. |
This illustrates that the highest salary isn't always in the biggest city, especially for primary care where recruitment to rural areas is a priority.
### 3. Practice Setting (Employer Type & Size)
Where a doctor works has a profound impact on their compensation structure and total earnings.
- Physician-Owned Private Practice: This setting traditionally offers the highest income potential. After a partnership track (typically 2-3 years), physicians become owners and share in the practice's profits. This model rewards efficiency and business acumen. However, it also comes with the responsibilities of running a business: administrative burdens, overhead costs, and managing staff.
- Large Hospital System Employment (e.g., Northwell Health, NYU Langone, Mount Sinai, NewYork-Presbyterian): This is now the most common employment model. It offers stability, predictable hours (for many specialties), excellent benefits, and no administrative overhead. The base salary might be slightly lower than top-end private practice, but the total package, including strong bonuses and retirement plans, is very competitive. There is often less autonomy than in private practice.
- Academic Medical Centers: Working for a university-affiliated hospital involves a tripartite mission: clinical care, teaching (medical students and residents), and research. This path often offers immense intellectual satisfaction and prestige but comes with a "pay cut." Academic salaries are consistently lower than in private practice or even general hospital employment, as a portion of one's time is dedicated to non-revenue-generating academic pursuits.
- Government/VA Hospitals: Physicians working for the Department of Veterans Affairs (VA) or other government entities are federal employees. Their salaries are often lower than in the private sector, but they come with exceptional benefits, including a federal pension, generous leave policies, and robust job security. The pace is often slower, and the bureaucratic hurdles can be significant.
- Locum Tenens: This means working as a temporary, independent contractor to fill in for other physicians. Locum tenens work offers very high daily or hourly rates and extreme flexibility, but it provides no benefits, stability, or paid time off. It's an attractive option for physicians between jobs or seeking to maximize earnings in the short term.
### 4. Years of Experience and Career Progression
As detailed in the salary table earlier, experience is a primary driver of income growth. A resident's salary in NYC is typically between $70,000 and $85,000, a fixed stipend that barely covers the high cost of living. Upon finishing residency, their salary immediately jumps by 300-500% to an entry-level attending salary.
From there, the growth trajectory continues for 10-15 years. This is due to several factors:
- Increased Efficiency: Experienced physicians are faster and more confident in their clinical and procedural work, allowing them to see more patients or perform more procedures (increasing RVU-based bonuses).
- Reputation and Referrals: A strong reputation builds a steady stream of patient referrals, which is crucial for specialists in private practice.
- Seniority and Leadership: With experience comes the opportunity for leadership roles—Medical Director, Department Chair, Chief of Staff—which carry additional administrative stipends and salary increases.
### 5. Level of Education (Degree and Sub-specialization)
While the baseline requirement is a medical degree (MD or DO), further specialization via a fellowship is a major salary determinant. A general internist who completes a three-year residency will earn significantly less than a colleague who, after the same residency, completes an additional three-year fellowship in cardiology. Those extra years of training directly translate to higher earning potential due to the specialized, often procedural, nature of the work. The choice to sub-specialize is one of the most critical financial decisions a young doctor makes.
### 6. In-Demand Skills and Other Factors
- Procedural Skills: The ability to perform in-demand, well-reimbursed procedures is a direct path to higher income.
- Bilingualism: In a place as diverse as New York City, being fluent in a second language (especially Spanish, Mandarin, Russian, or Bengali) is a highly valuable asset that can make a candidate more attractive to employers and lead to a larger patient panel.
- Telehealth Proficiency: The COVID-19 pandemic accelerated the adoption of telemedicine. Physicians who are comfortable and efficient with virtual care platforms can increase their patient volume and work more flexibly, potentially boosting income.
- Willingness to Work Undesirable Hours: In hospital-based specialties like Emergency Medicine or Hospitalist Medicine, physicians who are willing to work primarily nights, weekends, or holidays often receive a "shift differential," which is a higher hourly rate of pay.
---
Job Outlook and Career Growth for Doctors in NY

For those investing the immense time, effort, and capital to become a physician, the long-term career stability and growth prospects are a critical consideration. Fortunately, the outlook for physicians, both nationally and in New York, is exceptionally strong.
### National Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) projects that overall employment for physicians and surgeons will grow by 3% from 2022 to 2032. While this may seem slower than the average for all occupations, it's a bit misleading. The BLS notes that this figure represents a mix of specialties, some with faster growth than others. More importantly, this 3% growth still translates to about 23,800 projected job openings each year, on average, over the decade.
The primary drivers of this sustained demand are clear:
1. An Aging Population: The large baby-boomer generation is aging and living longer with multiple chronic conditions, which will continue to increase the demand for all types of physician services, from primary care to cardiology and oncology.
2. Physician Retirements: A significant portion of the current physician workforce is also approaching retirement age, creating openings that will need to be filled by new doctors.
3. Advances in Medicine: New treatments and technologies allow for the management of conditions that were once untreatable, expanding the scope and necessity of physician care.
### The New York-Specific Outlook
In New York, these national trends are amplified. The state has a large, aging population and is a major hub for "medical tourism," with patients traveling from around the world to seek care at its renowned medical centers. This creates a robust and dynamic job market.
However, the market is not without its challenges. There is an ongoing and well-documented shortage of primary care physicians, particularly in rural areas and underserved urban neighborhoods. This creates immense opportunity for family medicine physicians, internists, and pediatricians willing to work in these communities, often with the added incentive of state or
