Introduction

There are few moments in life as profound and transformative as the birth of a child. It's a time of immense joy, overwhelming love, and profound vulnerability. For new parents, the first few hours and days are a whirlwind of learning, healing, and bonding. In the center of this delicate transition stands a uniquely skilled and compassionate professional: the mother-baby nurse. If you're drawn to a career that combines deep medical knowledge with the incredible privilege of guiding families through this life-altering event, you're exploring a path that is not only emotionally rewarding but also professionally and financially stable.
So, what can you expect to earn in this vital role? The salary for a mother-baby nurse is competitive, with national averages often landing between $80,000 and $95,000 per year. However, this figure is just a starting point. With the right experience, education, and location, top earners in this field can command salaries well over $130,000 annually.
I'll never forget the quiet confidence of the nurse who cared for my sister after her first baby was born. She didn't just check vitals; she taught my brother-in-law how to swaddle, she spent 45 minutes helping my sister with a difficult first latch, and she reassured them both that their anxieties were normal. She was a teacher, a coach, and a guardian, all rolled into one, and her impact on their confidence as new parents was immeasurable. That is the power and purpose of a mother-baby nurse.
This guide will provide a comprehensive, data-driven look at the mother-baby nurse salary and the career path that leads to it. We will explore every factor that influences your earning potential, from your degree to your zip code, and provide a clear roadmap for how to enter and thrive in this exceptional field.
### Table of Contents
- [What Does a Mother-Baby Nurse Do?](#what-does-a-mother-baby-nurse-do)
- [Average Mother-Baby Nurse Salary: A Deep Dive](#average-mother-baby-nurse-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Mother-Baby Nurse Do?

A mother-baby nurse, also known as a postpartum nurse, is a registered nurse (RN) who specializes in the care of new mothers and their infants in the period immediately following childbirth until they are discharged from the hospital. This specialty is unique because the nurse cares for two patients simultaneously—the mother and the baby—as a single unit, often referred to as a "couplet" or "dyad." Their role is a dynamic blend of clinical assessment, hands-on care, patient education, and emotional support.
The core mission of a mother-baby nurse is to ensure the health and well-being of both patients, foster family bonding, and empower new parents with the knowledge and skills they need to care for their newborn at home confidently. This requires a broad skill set that encompasses both obstetrics and pediatrics.
Core Responsibilities and Daily Tasks:
- Postpartum Assessment (The Mother): Nurses perform regular, comprehensive assessments of the mother to monitor her recovery from childbirth. This includes checking vital signs, assessing the uterine fundus (to ensure it is contracting properly to prevent hemorrhage), evaluating lochia (postpartum bleeding), inspecting perineal incisions or C-section wounds for signs of infection, and managing postpartum pain.
- Newborn Assessment (The Baby): They conduct head-to-toe assessments of the newborn, monitoring vital signs, weight, feeding patterns, and urine/stool output. They are vigilant for common newborn issues such as jaundice (hyperbilirubinemia), hypoglycemia, and signs of infection. They also administer standard newborn medications and vaccinations, such as the Vitamin K injection and Hepatitis B vaccine, and perform newborn screening tests.
- Lactation and Feeding Support: A significant portion of the role involves providing education and hands-on assistance with feeding, whether it's breastfeeding or formula feeding. For breastfeeding mothers, this includes teaching proper latching techniques, various feeding positions, and how to recognize infant hunger cues. They help troubleshoot common issues like sore nipples or low milk supply and may coordinate with a certified lactation consultant (IBCLC) for more complex cases.
- Patient Education: This is perhaps the most critical function. Mother-baby nurses are primary educators. They teach parents everything from basic infant care (diapering, swaddling, bathing, cord care) to safety protocols (safe sleep practices to prevent SIDS). They also educate the mother on her own physical and emotional recovery, including signs of postpartum complications like preeclampsia or postpartum depression.
- Emotional Support and Family Integration: The postpartum period can be an emotional rollercoaster. Nurses provide crucial emotional support, listening to parents' concerns, validating their feelings, and providing reassurance. They facilitate family bonding, encouraging skin-to-skin contact and helping siblings and other family members adjust to the new baby.
- Discharge Planning and Coordination: From the moment of admission to the postpartum unit, the nurse is preparing the family for a safe discharge. This involves ensuring all educational topics have been covered, follow-up appointments are scheduled, and the parents have the necessary prescriptions and resources.
### A Day in the Life of a Mother-Baby Nurse
7:00 AM - Shift Handoff: The day begins with a detailed report from the night shift nurse. You learn about your assigned patients: typically 3 to 4 couplets. Today you have a first-time mom who had a vaginal delivery and is struggling with breastfeeding, a seasoned mom on her third baby who had a scheduled C-section, and a teenage mother whose baby is being monitored for low blood sugar.
7:30 AM - First Rounds: You visit your first couplet. You greet the new parents, perform a full assessment on the mother (vitals, fundal check, pain level) and a head-to-toe assessment on the baby. You notice the baby seems a bit jaundiced and make a note to follow up on the latest lab results.
9:00 AM - Medication and Education: You administer pain medication to your C-section patient and help her get out of bed to walk for the first time post-surgery. Afterwards, you spend 30 minutes with your first-time mom, using a pillow to help her find a comfortable breastfeeding position. You see a successful latch and praise her efforts, boosting her confidence.
11:00 AM - Charting and Collaboration: You meticulously document all assessments, interventions, and patient education in the electronic health record (EHR). The pediatrician rounds on the jaundiced baby; you discuss the care plan, which includes starting phototherapy. You coordinate with the lab for a repeat bilirubin level test.
1:00 PM - Lunch Break (if you're lucky!): You take a quick break to refuel.
1:30 PM - A New Admission: You receive a new admission from Labor & Delivery: a mother who had a long labor and is utterly exhausted. You help her get settled, perform initial assessments, and bring her a meal while encouraging her to rest.
3:00 PM - Discharge Teaching: Your C-section patient is scheduled to go home tomorrow. You sit down with her and her partner to review discharge instructions, covering wound care, activity restrictions, medications, and the critical signs and symptoms of complications for both mom and baby.
5:00 PM - Crisis and Calm: You check on your teenage mom and find her crying, overwhelmed by the baby's glucose checks. You provide a listening ear, offer words of encouragement, and celebrate with her when the baby's next blood sugar level is finally stable.
6:30 PM - Final Rounds and Handoff Prep: You make final rounds on all your patients, ensuring they are comfortable and have everything they need. You complete your charting and prepare a detailed, organized report for the incoming night shift nurse.
7:00 PM - Shift End: You walk out of the hospital, tired but fulfilled, knowing you made a tangible difference in the first, most formative days of several new families' lives.
Average Mother-Baby Nurse Salary: A Deep Dive
Understanding your potential earnings is a critical part of career planning. While passion for patient care is the driving force for most nurses, financial compensation is a significant factor in job satisfaction and long-term viability. The salary for a mother-baby nurse is strong, reflecting the specialized skills and high-stakes nature of the role.
It's important to note that the U.S. Bureau of Labor Statistics (BLS) provides salary data for "Registered Nurses" as a broad category, not for specific specialties. Therefore, to get a precise picture, we must synthesize BLS data with information from major salary aggregators that collect real-world salary data for specific job titles.
According to the most recent BLS data (May 2023), the median annual wage for all Registered Nurses was $86,070. The lowest 10 percent earned less than $63,720, and the highest 10 percent earned more than $132,680. This provides a solid baseline for the nursing profession as a whole.
However, specialized roles like mother-baby nursing often have a slightly different salary profile. Let's look at the more specific data:
- Salary.com reports that the average Mother/Baby Nurse salary in the United States is $88,901 as of May 2024, with a typical salary range falling between $80,920 and $99,784.
- Payscale.com indicates a similar figure, with the average base salary for a Postpartum Nurse being around $76,800 per year, but notes that total pay can reach up to $110,000 when accounting for bonuses and overtime.
- Glassdoor places the average total pay for a Mother Baby RN at $96,558 per year, combining a base salary of around $85,000 with additional pay like cash bonuses and shift differentials.
Synthesizing this data, it's reasonable to conclude that a mother-baby nurse in the U.S. can expect to earn a base salary starting in the mid-$70,000s and averaging in the high $80,000s to low $90,000s. However, the total compensation package often pushes annual earnings significantly higher.
### Salary by Experience Level
Like any profession, experience is a primary driver of salary growth. As a mother-baby nurse gains clinical expertise, develops advanced skills, and takes on more responsibility, their value—and compensation—increases.
Here is a typical salary progression based on years of experience, compiled from industry data:
| Experience Level | Years of Experience | Typical Annual Salary Range (Base) | Key Characteristics & Responsibilities |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $65,000 - $80,000 | A new graduate or a nurse transitioning from another specialty. Focuses on mastering core competencies, time management, and patient assessment under supervision. |
| Mid-Career | 3-9 Years | $80,000 - $100,000 | An experienced, confident nurse who can handle complex patient assignments independently. Often acts as a preceptor for new nurses and may pursue specialty certification (RNC-MNN). |
| Senior/Experienced | 10-19 Years | $95,000 - $115,000 | A clinical expert and leader on the unit. May function as a Charge Nurse, team lead, or committee member. Capable of managing the most challenging patient cases. |
| Late-Career/Expert | 20+ Years | $105,000 - $130,000+ | A veteran nurse, often in a formal leadership role like Unit Educator, Clinical Nurse Specialist, or Nurse Manager. May also be a highly paid senior staff nurse in a high-cost-of-living, unionized environment. |
*Source: Data synthesized from Payscale.com, Salary.com, and Glassdoor salary reports for Postpartum and Mother-Baby Nurses.*
### Beyond the Base Salary: Understanding Your Total Compensation
Your annual salary is only one piece of the puzzle. The total compensation package for a mother-baby nurse, particularly one working in a hospital setting, is often robust and adds significant value. When evaluating a job offer, be sure to consider:
- Shift Differentials: This is a substantial component of nursing pay. Nurses working evening shifts, night shifts, or weekend shifts receive a pay differential, which is an extra dollar amount added to their hourly rate. This can increase total earnings by 10-20% or more.
- Overtime Pay: Hospital units are busy, and working overtime is common. Overtime is federally mandated to be paid at 1.5 times the regular hourly rate, which can significantly boost income.
- On-Call Pay: Some units require nurses to be "on-call," meaning they must be available to come into work on short notice. They receive a small hourly wage simply for being available, and their full overtime rate if they are called in.
- Bonuses:
- Sign-On Bonus: Hospitals facing nursing shortages often offer significant sign-on bonuses, ranging from $5,000 to $20,000 or more, to attract qualified nurses.
- Performance/Clinical Ladder Bonus: Many hospitals have a "clinical ladder" program that rewards nurses for professional development activities like earning a certification, precepting students, or joining a committee. Advancing up the ladder comes with a raise or an annual bonus.
- Certification Pay: Earning a specialty certification like the Registered Nurse, Certified - Maternal Newborn Nursing (RNC-MNN) often comes with a direct pay increase or an annual bonus.
- Retirement Savings: Most employers offer a retirement plan, such as a 401(k) or 403(b) for non-profits. The employer match is a key benefit—if your employer matches 100% of your contributions up to 5% of your salary, that's an immediate 5% boost to your compensation.
- Health and Wellness Benefits: Comprehensive health, dental, and vision insurance is a standard and valuable part of the package.
- Tuition Reimbursement: Many hospital systems offer generous tuition reimbursement programs, which can help you earn a BSN or an advanced degree like an MSN at a fraction of the cost, directly increasing your future earning potential.
When all these factors are combined, a mother-baby nurse with a base salary of $85,000 could easily see their total compensation package valued at well over $110,000 per year.
Key Factors That Influence Salary

While the national averages provide a useful benchmark, your individual salary as a mother-baby nurse will be determined by a combination of powerful factors. Understanding these variables is the key to maximizing your earning potential throughout your career. This is the most critical section for anyone looking to strategically build a high-income career in this specialty.
###
Level of Education
Your educational foundation is one of the first and most significant determinants of your starting salary and long-term career trajectory. In nursing, the debate between an Associate's Degree in Nursing (ADN) and a Bachelor of Science in Nursing (BSN) is central to this.
- Associate's Degree in Nursing (ADN): An ADN is a two-year degree that provides the fastest route to becoming a registered nurse. While it qualifies you to sit for the NCLEX-RN licensure exam, many hospitals, especially major medical centers and those seeking or holding Magnet status, now require or strongly prefer BSN-prepared nurses. An ADN-prepared nurse may find their job opportunities limited to smaller hospitals or long-term care facilities, and their starting salary may be 5-10% lower than their BSN-prepared counterparts.
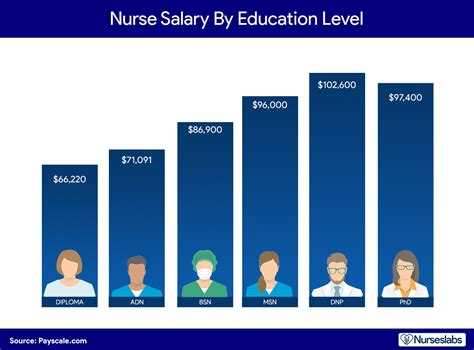
- Bachelor of Science in Nursing (BSN): A BSN is a four-year degree that includes all the clinical training of an ADN plus additional coursework in leadership, research, public health, and nursing theory. This broader education is highly valued by employers and is considered the gold standard for professional nursing. A BSN not only opens more doors—especially into competitive specialties like mother-baby—but also commands a higher salary. According to Payscale, nurses with a BSN earn an average of nearly $10,000 more per year than those with an ADN.
- Master of Science in Nursing (MSN): For those looking to move beyond the bedside, an MSN is the next step. This advanced degree can prepare you for leadership roles (Clinical Nurse Leader, Nurse Manager), education roles (Unit Educator), or advanced practice roles (Clinical Nurse Specialist - CNS). These positions come with a significant salary increase, often pushing earnings well into the $110,000 to $140,000+ range. A Perinatal CNS, for example, serves as an expert consultant for the entire service line, driving evidence-based practice and staff development.
The Bottom Line: While an ADN is a valid entry point, a BSN is the strategic choice for higher pay, better job prospects in premier hospitals, and the necessary foundation for future career and salary growth.
###
Years of Experience
As detailed in the salary table above, experience is king. Nursing is a practice-based profession where real-world clinical judgment is developed over time. Employers recognize and reward this accumulated wisdom.
- 0-2 Years (Novice to Advanced Beginner): In this stage, you are building confidence and competence. Your focus is on mastering skills and time management. Your salary reflects your entry-level status, but you can expect annual merit increases of 2-4%.
- 3-9 Years (Competent to Proficient): This is where significant salary growth occurs. You are now a reliable, independent practitioner. You can handle complex patient loads, serve as a resource for newer nurses (precepting), and begin to specialize. Earning a certification like the RNC-MNN during this phase is a key strategy to accelerate your pay. Nurses with 5-9 years of experience often see salaries 15-25% higher than new graduates.
- 10+ Years (Expert): As a senior nurse, you are a leader on the unit, whether in a formal or informal capacity. Your deep clinical knowledge makes you invaluable for managing high-risk situations. Many nurses at this stage take on roles like Charge Nurse, which comes with a pay differential. In unionized hospitals, pay scales are strictly seniority-based, meaning a 20-year veteran nurse can earn 50-70% more than a new graduate in the same role, simply based on their years of service.
###
Geographic Location
Where you choose to work is arguably the single most powerful factor influencing your salary. The demand for nurses and the cost of living vary dramatically across the United States, leading to vast pay disparities.
States with high costs of living, strong nursing unions, and competitive healthcare markets tend to offer the highest salaries. Conversely, states with lower costs of living and less union representation typically have lower pay scales.
Top 5 Highest-Paying States for Registered Nurses (BLS, May 2023):
1. California: Annual Mean Wage: $137,690
2. Hawaii: Annual Mean Wage: $119,710
3. Oregon: Annual Mean Wage: $109,620
4. Washington: Annual Mean Wage: $107,720
5. Alaska: Annual Mean Wage: $107,310
Top 5 Highest-Paying Metropolitan Areas for Registered Nurses (BLS, May 2023):
1. San Jose-Sunnyvale-Santa Clara, CA: Annual Mean Wage: $180,010
2. San Francisco-Oakland-Hayward, CA: Annual Mean Wage: $169,320
3. Vallejo-Fairfield, CA: Annual Mean Wage: $160,540
4. Sacramento-Roseville-Arden-Arcade, CA: Annual Mean Wage: $150,740
5. Salinas, CA: Annual Mean Wage: $145,030
A mother-baby nurse working in the San Francisco Bay Area could easily earn over $160,000 per year, while a nurse in a lower-paying state like Alabama (Annual Mean Wage: $71,640) or South Dakota (Annual Mean Wage: $68,170) might earn less than half that for the same job. It is crucial to research the salary norms in your target region and weigh them against the local cost of living.
###
Work Setting & Employer Type
The type of facility you work for has a direct impact on your compensation and benefits.
- Large Academic Medical Centers & Magnet Hospitals: These are typically the top payers. They are often unionized, have structured clinical ladder programs for advancement, and offer robust benefits packages and tuition reimbursement. They are also research and teaching hubs, providing an enriching professional environment. Competition for jobs here is fierce.
- Private, For-Profit Hospital Systems: These hospitals are run like businesses and can offer competitive salaries and sign-on bonuses to attract talent, especially in high-demand markets. Pay structures can vary widely from one system to another.
- Community and Non-Profit Hospitals: Pay may be slightly lower than at large academic centers, but these hospitals often offer a strong sense of community, a better work-life balance, and excellent benefits.
- Government Facilities (e.g., VA Hospitals, Military Hospitals): Government nursing jobs offer exceptional job security and outstanding federal benefits, including a generous pension plan (FERS). The pay scale (General Schedule or GS) is transparent and seniority-based, though it may not reach the highest peaks of private sector pay in some ares of California.
- Outpatient Birthing Centers: While less common for the initial postpartum stay, some facilities offer postpartum care. These roles may offer more predictable hours (no night shifts) but typically come with a lower salary compared to the 24/7, high-acuity environment of a hospital.
###
Area of Specialization & Certifications
Within the mother-baby specialty, you can further develop niche expertise that makes you more valuable.
- Specialty Certification (RNC-MNN): This is the most important credential for a mother-baby nurse. The Registered Nurse, Certified - Maternal Newborn Nursing certification is offered by the National Certification Corporation (NCC). Earning it demonstrates a high level of knowledge and commitment to the specialty. Most hospitals reward certified nurses with an annual bonus, a permanent hourly pay increase, and preference for advanced roles.
- Lactation Consulting (IBCLC): Many mother-baby nurses become dually certified as an International Board Certified Lactation Consultant (IBCLC). This makes them an invaluable resource on the unit, able to handle the most complex breastfeeding challenges. A nurse with an IBCLC can often command a higher salary or work in a hybrid role that combines bedside nursing with formal lactation consults.
- Charge Nurse/Team Lead: Taking on leadership responsibilities as a Charge Nurse for the unit comes with a pay differential (typically an extra $2-5 per hour) and is a stepping stone to management.
- Perinatal Educator: Some nurses specialize in patient education, teaching prenatal or postpartum classes on childbirth, newborn care, or
