Introduction

Imagine standing at the precipice of life, where every breath is a victory and every heartbeat a miracle. This is the world of the Neonatal Nurse Practitioner (NNP), a highly specialized role dedicated to the most vulnerable of patients: premature and critically ill newborns. If you are drawn to a career that combines profound purpose with advanced medical expertise and significant financial reward, you have arrived at the right place. The path to becoming a NICU NP is rigorous, but the destination offers a career that is not just a job, but a calling—one that also happens to be one of the most respected and well-compensated in the nursing profession.
The financial landscape for these specialists is compelling. While salaries fluctuate based on a variety of factors, the national median NICU NP salary hovers around an impressive $135,101 per year, with top earners exceeding $150,000 annually (Salary.com, 2024). This figure reflects the high level of education, critical responsibility, and specialized skill set required to thrive in the neonatal intensive care unit (NICU). I once spoke with a seasoned NICU NP who described her role not just as a medical provider, but as a "keeper of hope" for families on the most stressful days of their lives. That profound sense of purpose, she said, was the ultimate compensation, with the excellent salary being the vital foundation that allowed her to focus entirely on her life-saving work.
This comprehensive guide will serve as your definitive resource for understanding every facet of a NICU NP's career, with a special focus on salary potential. We will dissect the data, explore the influencing factors, and map out the exact steps you need to take to enter and excel in this extraordinary field.
### Table of Contents
- [What Does a NICU NP Do?](#what-is-a-nicu-np)
- [Average NICU NP Salary: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors)
- [Job Outlook and Career Growth](#job-outlook)
- [How to Become a NICU NP: Your Step-by-Step Guide](#how-to-become)
- [Conclusion: Is a NICU NP Career Right for You?](#conclusion)
What Does a NICU NP Do?

A Neonatal Nurse Practitioner is an Advanced Practice Registered Nurse (APRN) who has undergone extensive graduate-level education and clinical training to provide comprehensive, life-sustaining care to neonates. These patients range from extremely premature infants born months too soon to full-term babies with congenital anomalies, infections, or other life-threatening conditions. NNPs practice in a variety of settings, primarily within the tiered system of Neonatal Intensive Care Units (Level II, III, and IV).
They function as independent practitioners and as vital members of a collaborative healthcare team, working alongside neonatologists, pediatric surgeons, respiratory therapists, and a host of other specialists. Their scope of practice is vast and encompasses duties that were once exclusively the domain of physicians.
Core Roles and Responsibilities Include:
- Advanced Assessment and Diagnosis: Performing comprehensive physical examinations, interpreting complex lab results and imaging studies (X-rays, ultrasounds), and diagnosing acute and chronic neonatal illnesses.
- Developing and Managing Treatment Plans: Creating and implementing evidence-based plans of care, prescribing medications (including potent vasoactive drugs and antibiotics), and ordering and managing advanced therapies like mechanical ventilation and intravenous nutrition.
- Performing Advanced Procedures: NNPs are trained to perform highly technical, life-saving procedures. This can include endotracheal intubation, insertion of central and arterial lines (umbilical lines, PICC lines), lumbar punctures, chest tube placement, and needle aspiration.
- Attending High-Risk Deliveries: Being present in the delivery room for anticipated high-risk births to lead or assist in neonatal resuscitation, stabilizing the infant immediately after birth.
- Family-Centered Care and Education: Serving as the primary point of contact for parents and families. This involves explaining complex medical conditions in understandable terms, providing daily updates, offering emotional support, and educating parents on how to care for their baby, both in the NICU and in preparation for discharge.
- Collaboration and Leadership: Working seamlessly with neonatologists, fellows, residents, staff nurses, and other ancillary staff. NNPs often take a leadership role in rounds, care planning conferences, and quality improvement initiatives.
### A Day in the Life of a NICU NP
To truly understand the role, let's walk through a typical 12-hour shift for an NNP in a busy Level IV NICU.
- 7:00 AM - Handoff and Chart Review: The shift begins with a detailed sign-out from the night-shift NP or physician. You review the overnight events, lab results, and any changes for your assigned group of 4-6 critically ill infants. You meticulously check ventilator settings, fluid rates, medication orders, and nutrition plans.
- 8:30 AM - Morning Rounds: You lead or actively participate in multidisciplinary rounds. For each patient, you present a concise summary of their status, your physical exam findings, and your assessment and plan for the day. You collaborate with the neonatologist, bedside nurse, respiratory therapist, and pharmacist to finalize the day's orders.
- 10:00 AM - Procedures and Patient Care: One of your patients, a 25-week-gestation infant, needs a new peripherally inserted central catheter (PICC line) for long-term IV access. You prepare the sterile field, perform the procedure with ultrasound guidance, and order an X-ray to confirm placement.
- 12:00 PM - High-Risk Delivery: A stat page calls you to the delivery room for a 32-weeker with a known congenital heart defect. You lead the resuscitation team, intubating the infant at the bedside and placing an umbilical venous line for emergency medication access before transporting the stabilized baby to the NICU.
- 2:00 PM - Family Meeting: You meet with the parents of a long-term patient who is finally nearing discharge. You spend an hour teaching them CPR, how to use their baby's home oxygen equipment, and how to administer medications, patiently answering all their questions.
- 4:00 PM - Documentation and Follow-Up: The afternoon is dedicated to meticulously documenting all procedures, progress notes, and communication. You follow up on lab results from the morning, adjust medication dosages, and troubleshoot a feeding intolerance issue with another patient.
- 6:30 PM - Evening Sign-Out: You prepare a thorough, organized handoff for the incoming night-shift NP, highlighting key events, pending tasks, and any "watch-fors" on your patients.
- 7:30 PM - Departure: You leave the unit, mentally and emotionally tired, but with the profound knowledge that your expertise was the difference between life and death, and hope and despair, for multiple tiny patients and their families.
Average NICU NP Salary: A Deep Dive
The financial compensation for a NICU NP is a direct reflection of the advanced education, specialized skills, and immense responsibility the role entails. While the exact figure on your paycheck will depend on the factors we'll explore in the next section, we can establish a strong baseline by examining data from authoritative sources.
It's important to note that the U.S. Bureau of Labor Statistics (BLS) groups all Nurse Practitioners together in its reporting. The BLS data is an excellent starting point for understanding the profession's overall financial health. For 2023, the median annual wage for all Nurse Practitioners was $128,490. The profession shows a wide range, with the lowest 10 percent earning less than $94,960 and the highest 10 percent earning more than $174,930 (Source: [BLS Occupational Outlook Handbook, Nurse Practitioners](https://www.bls.gov/ooh/healthcare/nurse-anesthetists-nurse-midwives-and-nurse-practitioners.htm)).
However, to get a more precise picture of the NICU NP salary, we must turn to specialized salary aggregators that differentiate by subspecialty.
According to the latest 2024 data from Salary.com, the median annual salary specifically for a Neonatal Nurse Practitioner in the United States is $135,101. The typical salary range falls between $124,213 and $146,000. This demonstrates that NNPs, on average, earn a premium compared to the general NP median, acknowledging their critical care specialization.
### Salary Brackets by Experience Level
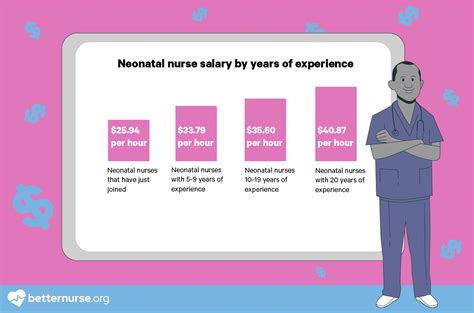
Like any profession, your earning potential as a NICU NP grows significantly with experience. As you transition from a new graduate to a seasoned clinical expert, your value to an organization—and your salary—increases accordingly.
Here is a breakdown of typical NICU NP salary expectations based on years of experience, compiled from data by sources like Payscale and Salary.com:
| Experience Level | Years of Experience | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level NNP | 0-2 Years | $110,000 - $125,000 | Recently graduated and certified. Focus is on consolidating core skills, developing clinical judgment, and working under close mentorship. |
| Mid-Career NNP | 3-9 Years | $125,000 - $140,000 | Proficient in a wide range of procedures and managing complex patients. Begins to take on informal leadership roles like precepting new NNPs. |
| Senior/Experienced NNP | 10-19 Years | $135,000 - $155,000 | Recognized as a clinical expert. Often leads quality improvement projects, participates in research, and may hold a formal role like Lead NNP or team coordinator. |
| Late-Career NNP | 20+ Years | $145,000 - $165,000+ | A veteran of the field. May have shifted into management, education, or administration. Highest earning potential, especially with a DNP and leadership responsibilities. |
*(Note: These are base salary ranges and do not include overtime, bonuses, or other compensation, which can add substantially to the total earnings.)*
### Beyond the Base Salary: Understanding Total Compensation
Your base salary is only one piece of the financial puzzle. A comprehensive compensation package for a NICU NP often includes several other valuable components that can increase total annual earnings by 10-20% or more.
- Sign-On Bonuses: In competitive markets, hospitals may offer substantial sign-on bonuses, often ranging from $5,000 to $20,000 or more, to attract top talent. These are usually tied to a commitment to stay with the employer for a specific period (e.g., 2-3 years).
- Shift Differentials: This is a significant factor. Working nights, weekends, and holidays comes with a premium pay rate. Night shift differentials can add 15-25% to your hourly base pay, while weekend differentials can add $2-$5 per hour. For an NNP working a rotating schedule, this can add thousands of dollars to their annual income.
- Overtime and On-Call Pay: Hospital-based NNPs often have opportunities for overtime, paid at 1.5 times the regular hourly rate. Many positions also involve on-call duties, where you are paid a small hourly stipend to be available and your full rate if you are called into work.
- Performance or Quality Bonuses: Some neonatology practices or hospital systems tie annual bonuses to meeting specific quality metrics, such as reducing infection rates or improving patient outcomes.
- Relocation Assistance: For NNPs moving to a new city for a job, employers frequently offer relocation packages worth several thousand dollars to cover moving expenses.
- Retirement Benefits: This is a cornerstone of long-term financial health. Employers typically offer a 401(k) or 403(b) plan with a matching contribution. A common match is 50-100% of your contribution up to 3-6% of your salary. This is essentially free money and a critical part of your total compensation.
- Continuing Education (CE) and Professional Development Funds: To maintain licensure and certification, NNPs need ongoing education. Most employers provide an annual stipend (e.g., $1,500 - $3,000) and paid time off to attend conferences or workshops.
- Tuition Reimbursement: Many hospital systems, particularly academic medical centers, offer tuition reimbursement for employees pursuing further education, such as a Doctor of Nursing Practice (DNP) degree.
- Health and Wellness Benefits: Comprehensive health, dental, and vision insurance, as well as life insurance and disability coverage, are standard components of a competitive benefits package.
When evaluating a job offer, it's crucial to look beyond the base salary and calculate the value of the entire compensation package to understand your true earning potential.
Key Factors That Influence NICU NP Salary
While we've established a national average, the actual salary you command as a NICU NP is a dynamic figure shaped by a confluence of critical factors. Understanding these variables is the key to strategically positioning yourself for maximum earning potential throughout your career. This section provides an exhaustive breakdown of what drives salary up—or holds it down.
###
1. Level of Education and Certification
The educational foundation of an NNP is the first and most fundamental determinant of salary. The journey is standardized but offers choices that can impact compensation.
- MSN vs. DNP: The minimum requirement to become a Neonatal NP is a Master of Science in Nursing (MSN). However, the Doctor of Nursing Practice (DNP) is increasingly becoming the preferred terminal degree for advanced practice. While the direct salary bump for a DNP over an MSN for a purely clinical role can be modest initially (perhaps a 3-7% increase), its true value lies in long-term career trajectory. A DNP prepares you for leadership, administration, policy-making, and academic roles, which come with significantly higher salaries. An NNP with a DNP who becomes a Director of Advanced Practice or a Clinical Associate Professor can easily earn $160,000 - $200,000+.
- The NNP-BC® Certification: This is the non-negotiable credential. All NNPs must pass the national certification examination offered by the National Certification Corporation (NCC) to earn the NNP-BC® (Neonatal Nurse Practitioner-Board Certified) credential. While holding the certification itself doesn't create salary tiers, *not* having it means you cannot practice as an NNP. Possessing additional certifications, while less common for direct salary increases, can make you a more attractive candidate. For example, a certification as a Clinical Nurse Specialist (CNS) or in a specific skill like lactation consultation (IBCLC) can add value and leverage in negotiations, particularly in specialized roles.
###
2. Years of Experience
As detailed in the previous section, experience is perhaps the single most powerful driver of salary growth in a clinical NNP role. The learning curve in a Level IV NICU is steep, and the clinical wisdom gained over years is invaluable.
- The New Graduate NNP (0-2 years): You are a significant investment for an institution. Your starting salary reflects your potential, but also the resources (mentorship, orientation, slower patient load) the hospital will invest in you. Your focus is on becoming safe and competent.
- The Competent NNP (3-9 years): This is where you see the most significant salary jumps. You are now a fully functional, autonomous provider who contributes immense value. You are proficient in procedures, can manage a full and complex patient load, and begin to mentor others. Your salary should reflect this transition from novice to expert. You can expect annual raises and will have significant leverage if you choose to change jobs.
- The Senior/Lead NNP (10+ years): At this stage, salary growth is often tied to taking on additional responsibilities. Simply being a bedside NNP for 20 years will see your salary plateau. However, by becoming a lead NNP, managing schedules, leading QI projects, participating in hospital committees, or pioneering new protocols, you justify a higher salary bracket. Experienced NNPs are crucial for maintaining unit stability and quality, and institutions will pay a premium to retain this expertise.
###
3. Geographic Location
Where you choose to practice has a monumental impact on your paycheck. Salaries for NNPs can vary by as much as $50,000 or more per year based on state and even metropolitan area. This variation is driven by cost of living, demand for specialized providers, state regulations on NP practice authority, and the prevalence of unionization.
Top-Paying States for Nurse Practitioners (including NNPs):
According to BLS data for all NPs, the following states consistently offer the highest average salaries. The high cost of living in these areas often corresponds with high wages.
1. California: Average NP Salary: $161,540
2. Washington: Average NP Salary: $145,710
3. New Jersey: Average NP Salary: $143,250
4. Oregon: Average NP Salary: $142,420
5. New York: Average NP Salary: $141,610
*(Source: BLS Occupational Employment and Wage Statistics, May 2023)*
An NNP in San Francisco or San Jose can command a salary well over $180,000, but this is offset by an extremely high cost of living.
Lower-Paying States for Nurse Practitioners:
Conversely, states with a lower cost of living and potentially lower demand tend to have lower average salaries.
- Tennessee: Average NP Salary: $105,430
- Alabama: Average NP Salary: $106,610
- South Carolina: Average NP Salary: $109,210
Cost of Living Adjustment is Key: A $140,000 salary in New York City may afford a lower quality of life than a $115,000 salary in a mid-sized Midwestern city. Aspiring NNPs should use a cost-of-living calculator to compare offers and understand their true purchasing power.
###
4. Facility Type and Work Setting
The type of institution you work for is another major salary determinant.
- Large Academic Medical Centers: These institutions (often university-affiliated) are typically the sites of Level IV NICUs. They often have strong nursing unions, leading to structured, transparent pay scales with regular step increases. While the base salary might sometimes be slightly lower than a top-tier private practice, the benefits are usually outstanding: excellent health insurance, generous retirement matching, and significant tuition benefits for yourself and your family. Total compensation can be very high.
- Large, Private Non-Profit Hospital Systems: These are also major employers of NNPs. Salaries are competitive and often market-driven. They may offer more flexibility in negotiation than a unionized public institution. Sign-on bonuses and performance bonuses can be more common here.
- Private Neonatology Groups: Many NNPs are employed not by a hospital, but by a private physician group that contracts its services to one or more hospitals. These positions can have the highest earning potential. Salary may be tied to productivity, RVUs (Relative Value Units), or practice profitability. This can be a high-risk, high-reward environment where a highly efficient and productive NNP can earn well above the national average. Benefits packages may be less robust than those at large academic centers.
- Community Hospitals (Level II/III NICUs): NNPs in smaller, regional hospitals may have a broader scope of responsibility as there are fewer fellows and residents. To attract an NNP away from a major metro center, these hospitals often have to offer a very competitive salary and may include attractive perks like student loan repayment assistance.
###
5. Area of Sub-Specialization and Unit Acuity
Within the world of neonatal care, there are further specializations and environments that can influence pay.
- NICU Acuity Level: The level of the NICU where you work is a significant factor.
- Level IV NICU: This is the highest level of care, for the most critically ill infants, including those requiring advanced surgical interventions like cardiac or ECMO (extracorporeal membrane oxygenation). Working in a Level IV unit requires the highest level of skill and often commands the highest salary due to the complexity and stress of the role.
- Level III NICU: Cares for very sick and premature infants but may transfer out those needing highly specialized surgery. Salaries are very competitive and in line with national averages.
- Level II Special Care Nursery: Cares for infants who are moderately ill or recovering from more critical illness. The pace is less intense, and the procedural demands are lower. Salaries for NNPs in Level II units may be slightly lower than in Level III/IV units.
- Specialized Teams: NNPs who join elite, specialized teams can often earn a premium.
- Neonatal Transport Team: These NNPs are responsible for stabilizing and transporting critically ill infants from outlying hospitals to a higher level of care, often by helicopter or ambulance. This role requires exceptional autonomy, procedural skill under pressure, and additional training (e.g., STABLE certification), and is often compensated with a higher base pay or stipends.
- ECMO/Cardiac NICU Teams: NNPs specializing in the care of infants with congenital heart disease or those requiring ECMO life support possess a rare and valuable skillset, which can translate to higher pay within a large medical center.
###
6. In-Demand Clinical and Professional Skills
Beyond your degree and years on the job, the specific, demonstrable skills you possess are your currency in salary negotiations. Cultivating these skills will make you an indispensable asset.
High-Value Clinical Skills:
- Advanced Procedural Competency: Being the "go-to" person for difficult intubations, challenging umbilical line placements, or PICC line insertions.
- Ventilator Management Expertise: Deep understanding of advanced ventilator modes, including high-frequency oscillation (HFO) and non-invasive ventilation.
- ECMO or CRRT Training: Certification and experience with these highly complex life-support technologies.
- Therapeutic Hypothermia (Cooling): Expertise in managing the cooling protocol for infants with hypoxic-ischemic encephalopathy (HIE).
- Point-of-Care Ultrasound (POCUS): Being trained to use ultrasound for procedural guidance (line placement) and basic diagnostic assessments (cardiac function, bladder scans).
High-Value Professional Skills:
- Leadership and Mentorship: Formally precepting new NNPs and RNs, acting as a team lead, or serving on unit leadership committees.
- Quality Improvement (QI) Project Leadership: Having a portfolio of successful QI projects you have led (e.g., reducing central line infections, improving feeding protocols) that demonstrate your ability to improve outcomes and save the hospital money.
- Research and Publication: Participating in or leading clinical research, and having your name on published papers or abstracts presented at national conferences.
- Bilingualism: In many parts of the country, being fluent in a second language (especially Spanish) is a highly valued skill that can sometimes come with a pay differential.
By strategically developing these facets of your professional profile, you can move from being a passive salary-taker to an active architect of your financial future.
Job Outlook and Career Growth

For those considering the significant investment of time and education required to become a NICU NP, the long-term career prospects are exceptionally bright. The demand for advanced practice providers, particularly in highly specialized fields like neonatology, is robust and projected to grow dramatically over the next decade.
### A Profession in High Demand
The U.S. Bureau of Labor Statistics (BLS) projects a staggering 45% growth for all nurse
