Table of Contents

- [What Does an OB/GYN Physician Assistant Do?](#what-does-an-obgyn-physician-assistant-do)
- [The OB/GYN PA Salary: A Comprehensive Breakdown](#the-obgyn-pa-salary-a-comprehensive-breakdown)
- [Key Factors That Influence Your OB/GYN PA Salary](#key-factors-that-influence-your-obgyn-pa-salary)
- [Job Outlook and Career Growth for OB/GYN PAs](#job-outlook-and-career-growth-for-obgyn-pas)
- [How to Become an OB/GYN Physician Assistant](#how-to-become-an-obgyn-physician-assistant)
- [Is a Career as an OB/GYN PA Right for You?](#is-a-career-as-an-obgyn-pa-right-for-you)
The decision to enter the medical field is rarely driven by a single motive. It's a complex blend of intellectual curiosity, a profound desire to help others, and, practically speaking, the need for a stable and rewarding career. For those drawn to the intricate and deeply personal field of women's health, the role of an Obstetrics and Gynecology Physician Assistant (OB/GYN PA) presents a uniquely compelling path. It's a career that places you at the very heart of a patient's life journey, from routine check-ups and family planning to the miracle of childbirth and the challenges of menopause.
But what does that translate to in terms of professional and financial reward? The query "OB/GYN PA salary" is more than just a search for a number; it's a search for validation that this demanding and vital career can provide a foundation for a secure future. The answer is a resounding yes. While salaries can vary significantly, the national median salary for experienced PAs in this specialty often ranges from $115,000 to over $140,000 annually, with top earners and those in high-demand areas commanding even more.
I once spoke with a friend who, during a high-risk pregnancy, found her greatest source of comfort not in the brilliant but brief visits from her obstetrician, but in the consistent, patient presence of the practice's PA. It was the PA who had the time to answer every anxious question, explain every test result in detail, and provide the steady reassurance that made all the difference. That is the irreplaceable value you bring to the table—a value that is increasingly recognized and compensated in today's healthcare landscape.
This guide is designed to be your definitive resource, moving beyond simple salary figures to explore the full spectrum of a career as an OB/GYN PA. We will delve into the nuances of compensation, dissect the factors that drive salary growth, map out the career trajectory, and provide an actionable roadmap to get you started. Whether you are a student exploring your options, a PA considering a specialty change, or simply curious about this dynamic profession, this article will provide the expert insights you need to make an informed decision.
What Does an OB/GYN Physician Assistant Do?

A Physician Assistant (PA) is a nationally certified and state-licensed medical professional who practices medicine on healthcare teams with physicians and other providers. An OB/GYN PA, therefore, is a specialist who works under the supervision of an obstetrician-gynecologist, providing a vast range of healthcare services to women throughout their lives. They are not merely "assistants" but are integral clinical providers, often serving as the primary point of contact for patients and ensuring continuity of care.
Their scope of practice is extensive and can be divided into two primary domains: obstetrics (care related to pregnancy and childbirth) and gynecology (care related to the female reproductive system). The specific duties are governed by the supervising physician's scope, state laws, and the PA's own experience and training, but a typical workload involves a dynamic mix of clinical, procedural, and educational responsibilities.
Core Responsibilities in an OB/GYN Setting:
- Patient History and Physical Exams: Performing comprehensive annual exams (including Pap tests and breast exams), taking detailed medical histories, and assessing new patient complaints.
- Prenatal and Postpartum Care: Managing routine prenatal visits, ordering and interpreting lab tests and ultrasounds, monitoring fetal development, educating expectant mothers on nutrition and lifestyle, and conducting postpartum check-ups.
- Gynecological Problem Visits: Diagnosing and treating common conditions such as vaginal infections, menstrual irregularities, pelvic pain, and symptoms of menopause.
- Family Planning and Contraception: Counseling patients on various contraceptive options, prescribing birth control, and performing procedures like IUD and contraceptive implant insertions and removals.
- In-Office Procedures: Performing procedures such as colposcopies (for abnormal Pap results), endometrial biopsies, and vulvar biopsies.
- Patient Education: Serving as a primary educator on topics like sexually transmitted infections (STIs), breast cancer screening, HPV vaccination, and general wellness.
- Surgical Assistance: In many settings, OB/GYN PAs act as the first-assist in the operating room for surgeries like Cesarean sections, hysterectomies, and laparoscopies.
- Prescribing Medication: Prescribing medications for a wide range of gynecological issues, prenatal needs, and hormonal therapies.
- Managing Patient Flow: In a busy practice, the PA is crucial for maintaining patient flow, handling urgent add-on appointments, and triaging patient phone calls.
### A Day in the Life of an OB/GYN PA
To make this role more tangible, let's walk through a hypothetical day for "PA Sarah," who works in a private practice affiliated with a local hospital.
- 7:30 AM - Hospital Rounds: Sarah arrives at the hospital to round on postpartum patients who delivered the previous day. She checks on their recovery, manages any pain or complications, answers questions about breastfeeding, and ensures they are prepared for discharge. She also quickly checks in on a patient who had a hysterectomy two days prior, for which she first-assisted in the OR.
- 8:30 AM - Morning Huddle: Sarah heads to the clinic and meets with her supervising physician, the other PAs, and the nursing staff. They review the day's patient schedule, flag any complex cases, and discuss the hospital patients.
- 9:00 AM - 12:30 PM - Morning Clinic: Sarah's morning is a mix of appointments. She sees three routine prenatal patients, one new OB patient for a full workup, two annual GYN exams, and one patient for an IUD insertion. In between, she reviews lab results that have come in and sends prescription refills to the pharmacy.
- 12:30 PM - 1:15 PM - Lunch & Charting: A quick lunch while catching up on charting from the morning. She dictates her notes, signs off on lab orders, and returns a patient call regarding abnormal bleeding.
- 1:15 PM - 4:30 PM - Afternoon Clinic: The afternoon brings more variety. She performs a colposcopy for a patient with an abnormal Pap smear, counsels a teenager on contraceptive options, and manages a patient struggling with severe menopausal symptoms. A patient calls with concerns about decreased fetal movement, and Sarah has her come in immediately for a non-stress test, which she performs and interprets.
- 4:30 PM - 5:30 PM - Wrap-up: Sarah finishes her patient charts, responds to messages in the electronic health record (EHR), and consults with her supervising physician about the colposcopy results and a plan for a patient with complex pelvic pain. She confirms the OR schedule for the next day, where she is scheduled to assist with a C-section.
This example illustrates the immense variety and autonomy in the role. An OB/GYN PA is a problem-solver, an educator, a proceduralist, and a compassionate caregiver, all in one day.
The OB/GYN PA Salary: A Comprehensive Breakdown
Understanding the earning potential is a critical component of career planning. The salary for a Physician Assistant is robust, reflecting the high level of education, responsibility, and skill required. While the OB/GYN specialty is demanding, it is also compensated competitively within the PA profession.
To provide the most accurate picture, we will analyze data from several authoritative sources, including the U.S. Bureau of Labor Statistics (BLS), the American Academy of PAs (AAPA), and leading salary aggregators.
### The National Benchmark: PA Salary Across All Specialties
First, let's establish a baseline. The U.S. Bureau of Labor Statistics (BLS) provides a comprehensive overview of PA compensation across the entire United States, regardless of specialty.
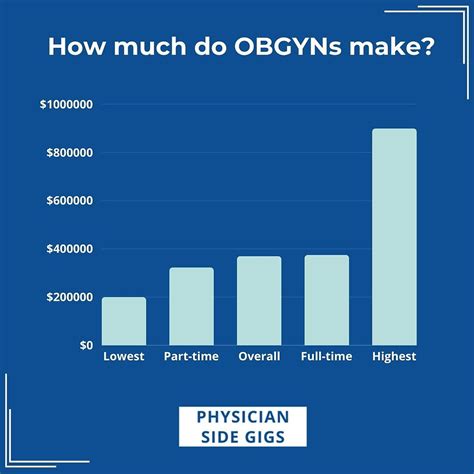
According to the BLS Occupational Outlook Handbook (data from May 2022), the median annual wage for all Physician Assistants was $126,010. This means that half of all PAs earned more than this amount, and half earned less. The salary distribution shows a wide range:
- Lowest 10%: Earned less than $80,070
- Median (50%): $126,010
- Highest 10%: Earned more than $164,620
This data is an excellent starting point, but specialty plays a significant role in determining actual income.
### Specialty Spotlight: The OB/GYN PA Salary
To get a more precise figure for the OB/GYN field, we turn to the industry's most definitive resource: the AAPA Salary Report. This report surveys thousands of PAs across the country, providing granular data on compensation by specialty, experience, location, and more.
According to the 2023 AAPA Salary Report (reflecting 2022 data), the median total compensation for PAs specializing in Obstetrics and Gynecology was highly competitive. While specific numbers can fluctuate slightly year to year, PAs in OB/GYN have consistently earned salaries around or slightly above the national median for all PAs.
The report found that the median base salary for a full-time PA in OB/GYN was $115,000. However, base salary is only part of the story. When considering median total compensation (which includes bonuses and other pay), this figure rises. For instance, data from previous years and other sources suggests a median total income closer to $120,000 - $125,000.
Salary aggregators provide further real-time insights:
- Salary.com (as of late 2023) reports the median salary for a "Physician Assistant - OB/GYN" in the United States to be approximately $128,400, with a typical range falling between $118,300 and $138,500.
- Payscale.com indicates a similar average base salary, often noting additional compensation in the form of bonuses that can add several thousand dollars to the annual total.
Summary of OB/GYN PA Salary Data:
- Median Base Salary: ~$115,000 - $120,000
- Median Total Compensation: ~$120,000 - $130,000+
- Typical Range (Experienced): ~$118,000 - $140,000+
### Salary Growth by Experience Level
Your earning potential as an OB/GYN PA is not static; it grows significantly with experience. As you build clinical confidence, master procedural skills, and become a more efficient and autonomous provider, your value to a practice increases exponentially.
Here is a typical salary progression based on data from the AAPA and other industry sources:
| Experience Level | Years in Practice | Typical Median Base Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level / New Graduate | 0-1 years | $95,000 - $110,000 | Focus on learning practice flow, building a patient panel, and mastering core competencies under closer supervision. |
| Early Career | 2-5 years | $110,000 - $125,000 | Increased autonomy, faster patient throughput, and proficiency in common in-office procedures. May begin taking on more call. |
| Mid-Career | 6-10 years | $125,000 - $140,000 | Considered a senior clinician. Often involved in training new staff, leading quality improvement projects, or developing a sub-specialty focus. |
| Senior / Experienced | 10+ years | $135,000 - $155,000+ | Expert level of practice. May hold a leadership role (e.g., Lead PA). Highest earning potential, especially if compensated on productivity. |
*Note: These are national estimates. Actual figures can be higher or lower based on the influential factors discussed in the next section.*
### Beyond the Base Salary: Understanding Total Compensation
A savvy professional looks beyond the base salary to evaluate the entire compensation package. In the world of OB/GYN PAs, this is particularly important, as bonuses and benefits can add significant value.
Common Components of an OB/GYN PA's Compensation Package:
1. Base Salary: The guaranteed annual or hourly wage. This forms the foundation of your income.
2. Productivity Bonus: This is extremely common. Many practices incentivize PAs based on the volume of patients they see or the revenue they generate. This is often calculated using Relative Value Units (RVUs), a standardized measure of the value of a medical service. A PA who is efficient and performs many procedures can earn a substantial annual bonus, sometimes adding 10-20% to their base salary.
3. On-Call Pay: PAs who share in the "call" schedule (being available after hours and on weekends for patient emergencies or hospital deliveries) are typically compensated for this time. This can be a flat per-diem rate, an hourly rate for time spent working, or a combination.
4. Surgical Assist Fees: In some private practice models, a PA may receive a portion of the fee billed for first-assisting in surgery, though it's more common for this work to be covered by the base salary in a hospital-employed model.
5. Sign-On Bonus: To attract talent in competitive markets, employers may offer a one-time bonus of $5,000 to $20,000+ upon signing an employment contract.
6. Relocation Assistance: Financial help for moving expenses if the job is in a different city or state.
7. Continuing Medical Education (CME): A crucial benefit. Employers typically provide an annual allowance (e.g., $2,000 - $4,000) and paid time off (e.g., 5 days) to attend conferences and maintain certification.
8. Professional Dues and Licensing: Coverage for state license renewals, DEA registration fees, and membership in professional organizations like the AAPA and the Association of PAs in OB/GYN (APAOG).
9. Retirement Plans: Access to a 401(k) or 403(b) plan, often with a generous employer match.
10. Health Insurance and Malpractice Insurance: Comprehensive health, dental, and vision insurance is standard. Crucially, the employer must provide full malpractice ("liability") insurance coverage.
When evaluating a job offer, it's essential to calculate the total value of the package, not just the number on the paycheck. A lower base salary with an excellent productivity bonus structure and robust benefits can often be more lucrative than a higher-paying job with minimal extras.
Key Factors That Influence Your OB/GYN PA Salary
While we've established a solid baseline for an OB/GYN PA's salary, the actual figure on your employment contract will be influenced by a powerful combination of personal and environmental factors. Understanding these variables is the key to negotiating effectively and maximizing your long-term earning potential. Think of your salary not as a single number, but as an equation with multiple inputs. Mastering these inputs gives you control over the outcome.
### 1. Geographic Location: The Power of Place
Where you choose to practice is arguably the single most significant factor impacting your salary. The demand for healthcare providers, the cost of living, and state-level regulations create a widely varied compensation landscape across the United States.
High-Paying States and Regions:
Generally, states in the Pacific West (California, Washington, Oregon, Alaska, Hawaii) and the Northeast (New York, Connecticut, New Jersey, Massachusetts) tend to offer the highest PA salaries. This is often driven by a higher cost of living and strong demand. For example, according to BLS data, the top-paying states for PAs across all specialties include:
1. Washington
2. California
3. Alaska
4. Hawaii
5. Oregon
A PA working in a major metropolitan area like San Francisco, New York City, or Los Angeles can expect a salary significantly higher than the national median—often in the $140,000 to $160,000+ range. However, this comes with a proportionally higher cost of living.
Hidden Gems: High Salary, Lower Cost of Living:
The most strategic locations often lie in a sweet spot: states with competitive salaries but a more moderate cost of living. States in the Southwest (Arizona, New Mexico) and certain areas of the Midwest and Southeast can offer excellent financial opportunities. Furthermore, states with more favorable practice laws for PAs (granting more autonomy) may also offer higher compensation to attract and retain talent.
Rural vs. Urban:
The dynamic between rural and urban salaries is complex. While major cities typically offer the highest absolute salaries, rural and medically underserved areas often provide powerful financial incentives to attract providers. A PA position in a rural community might come with:
- A competitive or even higher base salary than in a saturated suburban market.
- Significant sign-on bonuses.
- Student loan repayment programs, such as the National Health Service Corps (NHSC) Loan Repayment Program, which can be worth tens of thousands of dollars.
When considering location, it's crucial to analyze the salary-to-cost-of-living ratio. A $130,000 salary in Houston, Texas, may afford a much higher quality of life than a $150,000 salary in San Jose, California.
### 2. Practice Setting: The Impact of Your Work Environment
The type of facility you work in has a direct correlation with your compensation structure and overall earnings.
Private OB/GYN Practice:
- Small to Mid-Sized Groups: This is a very common setting. Compensation is often a mix of a base salary and a strong productivity bonus. The potential for high earnings exists if the practice is busy and you are an efficient provider. The culture can be more tight-knit, but benefits might be less robust than in a large hospital system.
- Large, Multi-Specialty Groups: These larger organizations may offer more structured salary tiers and comprehensive benefits packages. There might be more corporate oversight but also greater stability and internal opportunities for advancement.
Hospital Systems & Academic Medical Centers:
- Structure: These are typically salaried positions. Compensation is often predictable and transparent, based on established pay grades tied to years of experience.
- Pros: Salaries are generally competitive, and the benefits packages are almost always excellent, with strong retirement contributions, generous paid time off, and access to top-tier health insurance. There are often opportunities for teaching, research, and working with residents.
- Cons: Productivity bonuses may be smaller or non-existent compared to private practice. The pace can be intense, and the work may be more siloed. Salary ceilings might be more rigid.
Community Health Centers / Federally Qualified Health Centers (FQHCs):
- Mission and Compensation: These centers serve medically underserved populations. While their base salaries have historically been slightly lower than in the private sector, this gap has been closing rapidly due to provider shortages.
- The X-Factor: Loan Repayment: The primary financial advantage of working in an FQHC is eligibility for federal and state loan repayment programs. The NHSC program can provide up to $50,000 in tax-free loan repayment in exchange for a two-year service commitment. For a new graduate with significant student debt, this is a massive compensation benefit that can outweigh a higher base salary elsewhere.
Fertility Clinics (Reproductive Endocrinology and Infertility - REI):
- A Lucrative Sub-specialty: This is a highly specialized, often cash-based area of medicine. PAs in REI perform specialized procedures, coordinate complex treatment cycles, and work with a very motivated patient population. Due to the specialized nature of the work, salaries for experienced PAs in REI are often among the highest in the OB/GYN field, frequently exceeding $150,000.
### 3. Sub-specialization & Advanced Procedural Skills
Within the broad field of OB/GYN, developing a niche skillset is a direct path to a higher salary. A generalist is valuable, but an expert is indispensable.
Surgical First-Assisting:
A PA who is a skilled and reliable first-assistant in the operating room is a tremendous asset to an OB/GYN surgeon. Proficiency in assisting with major procedures like C-sections, hysterectomies (abdominal, vaginal, and laparoscopic/robotic), and myomectomies makes you more valuable. In some private practice models, this can lead to direct additional compensation. In a hospital setting, it makes you a candidate for higher-paying, surgery-heavy positions.
Advanced In-Office Procedures:
While most OB/GYN PAs perform IUD insertions and basic biopsies, mastering more advanced techniques can boost your earning potential, particularly in a productivity-based model. These skills include:
- Colposcopy and LEEP (Loop Electrosurgical Excision Procedure): For managing abnormal cervical cells.
- Hysteroscopy: Visualizing the inside of the uterus.
- Urodynamic Testing: For evaluating urinary incontinence.
- Obstetrical Ultrasound: Performing and interpreting basic ultrasounds in-house adds significant value and revenue to a practice.
Sub-specialty Focus:
Dedicating your practice to a specific area of OB/GYN can lead to specialized, higher-paying roles:
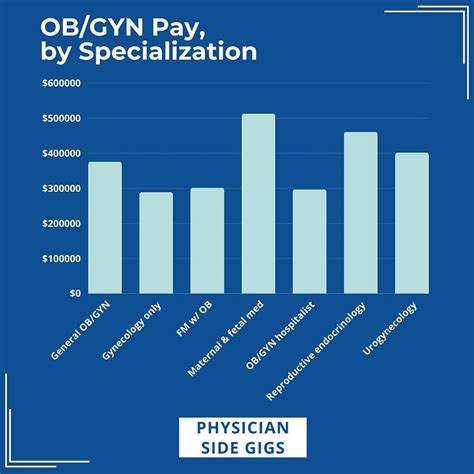
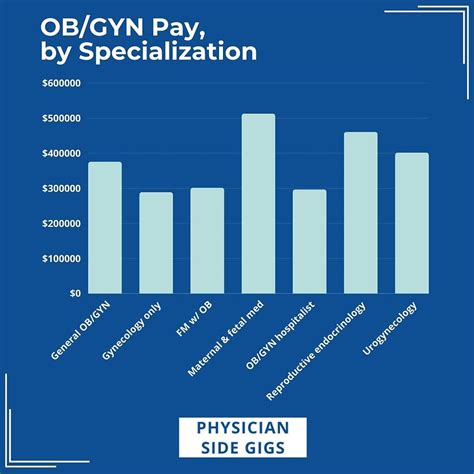
- Reproductive Endocrinology and Infertility (REI): As mentioned, this is a top-tier earning path.
- Urogynecology: Focusing on female pelvic floor disorders like incontinence and prolapse.
- Gynecologic Oncology: Working with physicians who treat cancers of the reproductive organs. This demanding field often commands higher compensation.
- High-Risk Obstetrics (Maternal-Fetal Medicine): Assisting in the management of complex pregnancies.
### 4. Compensation Model: Base Salary vs. Productivity
Understanding how you are paid is just as important as how much you are paid.
- Straight Salary: You receive a fixed, predictable annual salary. This is common in academic centers and some hospital systems. It provides stability but may not reward high performers.
- Base Salary + Productivity Bonus: This is the most common model in private practice. You receive a guaranteed base salary, plus a bonus calculated on your productivity. Productivity is typically measured in Relative Value Units (RVUs), which are assigned to every patient visit and procedure. The more patients you see and the more procedures you perform, the more RVUs you generate, and the higher your bonus. This model offers high earning potential for efficient and skilled PAs.
- Pure Productivity: Less common for new PAs, this model offers no guaranteed salary. Your entire income is based on a percentage of the revenue or RVUs you generate. This carries the highest risk but also the highest potential reward for established, busy providers.
When negotiating, clarify the bonus structure. Ask: What is the RVU threshold to start earning a bonus? How much are you paid per RVU above that threshold? Can you see a report of what current PAs are generating?
### 5. Advanced Education and Certifications
While a Master's degree is the standard for entry into PA practice, further education can enhance your credentials and earning potential.
- Doctor of Medical Science (DMSc): This advanced degree is becoming more popular. A DMSc can have a concentration in leadership, education, or a specific clinical area. While it may not provide an immediate salary bump in a clinical role, it can make you a much stronger candidate for leadership positions (Lead PA, Director of APPs), academic roles, and administrative jobs, which do come with higher salaries.
- Postgraduate PA Residencies/Fellowships: These are intensive, 12-month training programs in a specialty area like OB/GYN, surgery, or emergency medicine. Completing an OB/GYN residency provides an unparalleled level of focused training. While you earn a reduced stipend during the residency year, you graduate with the skills and confidence of a PA with 3-5 years of on-the-job training. This allows you to command a higher starting salary and immediately qualify