Introduction

Imagine being the calm, steady presence in a room electric with anticipation. You are the expert a family turns to during one of life’s most profound and vulnerable moments: the birth of a child. This is the world of an obstetrics (OB) nurse. It's a career that demands immense skill, deep compassion, and unwavering resilience, but it offers a reward few other professions can match—the privilege of helping to bring new life into the world. If you're drawn to this powerful blend of science and soul, you're likely also wondering about the practicalities: What does an obstetrics nurse earn? Is it a stable career path with room for growth?
The answer is a resounding yes. The field of obstetrics nursing is not only emotionally fulfilling but also financially rewarding and professionally secure. On average, a registered nurse specializing in obstetrics can expect to earn a national average salary of approximately $89,010 per year, with a typical range falling between $75,000 and over $130,000 annually, depending on a confluence of factors we will explore in detail. I once spoke with a veteran L&D nurse who told me, "You'll have days that break your heart and days that make it soar higher than you thought possible, sometimes in the same shift. The salary supports my family, but the work sustains my spirit."
This comprehensive guide is designed to be your definitive resource on the obstetrics nurse salary and career path. We will dissect every component of compensation, from entry-level earnings to the peak potential for seasoned experts. We'll explore the critical factors that influence your pay, analyze the robust job outlook for the coming decade, and provide a clear, step-by-step roadmap for launching your own career in this extraordinary field.
### Table of Contents
- [What Does an Obstetrics Nurse Do?](#what-does-an-obstetrics-nurse-do)
- [Average Obstetrics Nurse Salary: A Deep Dive](#average-obstetrics-nurse-salary-a-deep-dive)
- [Key Factors That Influence an Obstetrics Nurse Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Become an Obstetrics Nurse: A Step-by-Step Guide](#how-to-become-an-obstetrics-nurse-a-step-by-step-guide)
- [Conclusion: Is a Career in Obstetrics Nursing Right for You?](#conclusion)
What Does an Obstetrics Nurse Do?
An obstetrics nurse, often called a labor and delivery (L&D) nurse or a perinatal nurse, is a registered nurse (RN) who specializes in caring for women throughout the entire childbirth process. Their scope of practice is remarkably broad, covering pregnancy (antepartum), labor and birth (intrapartum), and the immediate period after delivery (postpartum). They are the frontline caregivers, a unique blend of medical expert, patient advocate, educator, and emotional support system.
Their responsibilities are dynamic and shift dramatically based on the patient's stage and needs. These duties can be broken down into several key phases:
- Antepartum Care: For patients experiencing high-risk pregnancies, OB nurses in antepartum units provide continuous monitoring and care. This can involve managing conditions like preeclampsia, gestational diabetes, or preterm labor, administering medications, and educating patients on their condition.
- Intrapartum (Labor and Delivery) Care: This is the most widely recognized aspect of the role. During labor, an L&D nurse is responsible for:
- Monitoring the mother's vital signs (blood pressure, heart rate, temperature).
- Tracking the progression of labor, including cervical dilation and effacement.
- Continuously monitoring the fetal heart rate using electronic fetal monitoring (EFM) to ensure the baby's well-being.
- Administering medications as ordered, such as Pitocin to augment labor or epidurals for pain management.
- Acting as a "coach," providing breathing techniques, positioning advice, and constant encouragement.
- Assisting the physician or certified nurse-midwife during the delivery.
- Being prepared for emergencies, such as a sudden drop in fetal heart rate, and initiating immediate interventions.
- In many hospitals, OB nurses also act as circulating nurses in the operating room during Cesarean sections (C-sections).
- Postpartum Care: After delivery, the focus shifts to the recovery of the mother and the health of the newborn. The OB nurse, often called a "mother-baby nurse" in this setting, will:
- Assess the mother for signs of hemorrhage or other complications.
- Manage postpartum pain.
- Educate new parents on newborn care, including feeding (breastfeeding support is a major component), bathing, and recognizing signs of illness.
- Perform newborn assessments and administer necessary medications or vaccinations.
- Patient and Family Education: Throughout every stage, education is paramount. OB nurses empower parents with the knowledge they need to navigate pregnancy, birth, and early parenthood with confidence.
### A Day in the Life of an L&D Nurse
To truly understand the role, let's walk through a hypothetical 12-hour shift:
- 7:00 AM: Arrive at the unit, get your patient assignments, and receive a detailed handoff report from the night shift nurse. Your primary patient is a first-time mom, 6 cm dilated, with an epidural in place.
- 7:30 AM: You enter the patient's room, introduce yourself, and build rapport. You perform a full assessment: check the mother's vitals, assess her pain level, and analyze the fetal monitoring strip. Everything looks stable.
- 9:00 AM: The patient is progressing well. You help her change positions to facilitate labor and ensure the baby is in an optimal position. You answer her partner's questions about what to expect next.
- 11:00 AM: The physician comes to check on the patient. You provide a concise, professional update (SBAR report) on her progress. A new patient arrives in triage with contractions, and you perform the initial assessment to see if she is in active labor.
- 1:00 PM: Your primary patient is now fully dilated and feeling the urge to push. The room's atmosphere shifts. You become the coach, guiding her breathing, providing encouragement, and monitoring the baby's response to pushing.
- 2:15 PM: After an hour of pushing, a healthy baby girl is born! You assist the physician, note the time of birth, and place the baby skin-to-skin on the mother's chest.
- 2:30 PM - 4:30 PM: This is the "golden hour." You closely monitor both mom and baby, assessing for any potential complications like postpartum hemorrhage. You assist with the first latch if the mother is breastfeeding and perform the initial newborn assessment.
- 5:00 PM: You transfer the stable mother-baby couplet to the postpartum unit, giving a thorough report to the receiving nurse. You then admit a new patient who is scheduled for an induction.
- 6:45 PM: You complete your charting for all patients, ensuring every intervention, assessment, and communication is meticulously documented. You prepare your handoff report for the incoming night shift nurse.
- 7:15 PM: After giving a report, you finally leave the unit, emotionally and physically tired but with the deep satisfaction of having been part of a family's most important day.
Average Obstetrics Nurse Salary: A Deep Dive
When evaluating a career, compensation is a critical factor. For obstetrics nurses, the financial outlook is strong and competitive within the nursing profession. It's important to understand that salary data can be presented in a few ways. The U.S. Bureau of Labor Statistics (BLS) provides the most authoritative data for "Registered Nurses" as a broad category, while specialized salary aggregators offer more targeted insights for OB nurses specifically.
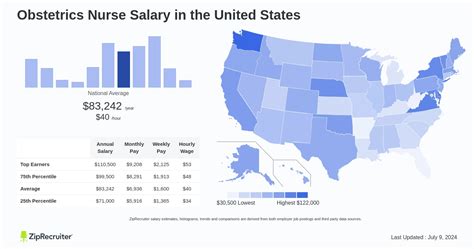
### National Averages and Salary Ranges
According to the most recent data from the U.S. Bureau of Labor Statistics (BLS) Occupational Outlook Handbook, the median annual wage for all registered nurses was $86,070 in May 2023. This figure serves as an excellent baseline.
However, specialized fields like obstetrics often command slightly different pay scales due to the unique skills, high-stakes environment, and potential for overtime and differential pay. More specific data from reputable salary aggregators paints a clearer picture for OB nurses:
- Salary.com reports that the average Obstetrics and Gynaecology (OB/GYN) Nurse salary in the United States is $89,849 as of May 2024, with a typical salary range falling between $81,770 and $101,235.
- Payscale.com provides a similar range, indicating an average base salary of around $75,000 per year, with the total pay (including bonuses and overtime) reaching up to $105,000 for experienced professionals.
- Glassdoor estimates the total pay for a Labor and Delivery Nurse to be around $104,821 per year in the United States, which includes an average base salary of $90,123 and additional pay (bonuses, profit sharing, etc.) of approximately $14,698.
Key Takeaway: A conservative national average for an OB nurse falls between $85,000 and $95,000 per year. Entry-level nurses may start closer to $70,000, while highly experienced nurses in high-paying states can easily surpass $130,000 or more.
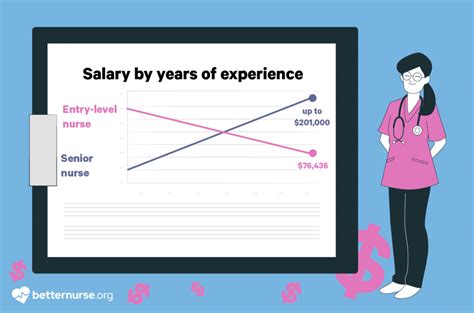
### Salary by Experience Level
Like most professions, compensation for OB nurses grows significantly with experience. As a nurse develops clinical judgment, hones specialized skills, and takes on more responsibility, their value—and salary—increases accordingly.
Here is a typical salary progression based on years of experience, compiled from industry data:
| Experience Level | Typical Years in Field | Typical Annual Salary Range | Key Responsibilities & Skills |
| :--- | :--- | :--- | :--- |
| Entry-Level (Nurse I) | 0-2 years | $70,000 - $85,000 | Mastering foundational skills, learning unit protocols, developing clinical judgment, managing 1-2 low-risk patients. |
| Mid-Career (Nurse II) | 2-5 years | $85,000 - $100,000 | Proficient in all aspects of OB care, can manage higher-risk patients, starts to precept new nurses, competent in emergencies. |
| Experienced (Nurse III) | 5-10 years | $95,000 - $115,000 | Expert clinical skills, often acts as a resource or "charge nurse" for the unit, mentors other staff, may lead quality improvement projects. |
| Senior/Expert (Nurse IV/Clinical Lead) | 10+ years | $110,000 - $130,000+ | Serves as a clinical leader, may have advanced certifications, potential to move into management or education roles. Deep expertise in complex cases. |
*Note: These ranges are national averages and can be significantly higher in certain geographic locations.*
### A Closer Look at the Compensation Package
The annual salary is only one piece of the puzzle. A comprehensive compensation package for an OB nurse often includes several other valuable components:
- Base Salary: The fixed hourly wage or annual salary you earn.
- Shift Differentials: This is a crucial component for hospital-based nurses. Expect a significant pay increase (often 10-25% of your base rate) for working evening shifts, night shifts, weekends, and holidays. Because babies are born 24/7, many OB nurses work these less traditional hours, substantially boosting their take-home pay.
- On-Call Pay: Some roles, particularly in smaller hospitals, may require nurses to be "on-call." This involves receiving a small hourly stipend to be available and then being paid a premium rate (often time-and-a-half) if called into work.
- Overtime Pay: Nursing shortages and unpredictable patient volume mean overtime is common. All non-exempt hourly nurses are entitled to overtime pay, typically 1.5 times their regular hourly rate, for any hours worked over 40 in a week.
- Bonuses: Sign-on bonuses are increasingly common, especially in high-demand areas, and can range from $5,000 to $20,000 or more. Retention bonuses may also be offered to experienced nurses.
- Benefits: This is an invaluable part of compensation. A strong benefits package includes:
- Health Insurance: Comprehensive medical, dental, and vision plans.
- Retirement Savings: Access to a 401(k) or 403(b) plan, often with a generous employer match.
- Paid Time Off (PTO): Includes vacation days, sick leave, and personal days.
- Tuition Reimbursement: Many hospital systems offer financial assistance for nurses pursuing higher education (e.g., a BSN or MSN), a major perk for career advancement.
- Life and Disability Insurance: Provides a financial safety net for you and your family.
When considering a job offer, it's essential to evaluate the entire compensation package, not just the base salary. A lower base salary with excellent shift differentials and a strong retirement match might be more valuable in the long run than a slightly higher base salary with poor benefits.
Key Factors That Influence an Obstetrics Nurse Salary
While national averages provide a useful benchmark, your actual earnings as an obstetrics nurse will be determined by a specific set of variables. Understanding these factors is key to maximizing your earning potential throughout your career. This is the most critical section for anyone looking to strategically build a high-earning career in OB nursing.
### 1. Level of Education and Certification
Your educational foundation is one of the most significant determinants of your starting salary and long-term career trajectory.
- Associate Degree in Nursing (ADN): An ADN is the minimum requirement to become a registered nurse. While it's the fastest path (typically 2 years), nurses with an ADN may face lower starting salaries and find that many major hospitals, particularly those with Magnet designation, exclusively hire or strongly prefer BSN-prepared nurses.
- Bachelor of Science in Nursing (BSN): A BSN (4-year degree) is increasingly becoming the industry standard. According to a 2023 survey by the American Association of Colleges of Nursing (AACN), BSN-prepared nurses earn higher salaries than their ADN-prepared counterparts. The BSN curriculum includes more in-depth training in leadership, research, and community health, making these graduates more desirable to employers and positioning them for leadership roles and higher pay grades.
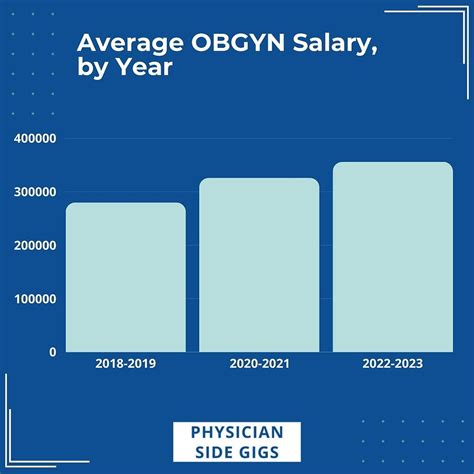
- Master of Science in Nursing (MSN) / Doctor of Nursing Practice (DNP): Pursuing an advanced degree opens the door to the highest-paid roles in and adjacent to obstetrics.
- Certified Nurse-Midwife (CNM): An advanced practice registered nurse (APRN) who provides comprehensive care to women, including delivering babies. According to the BLS, the median salary for nurse midwives was $129,650 in May 2023.
- Women's Health Nurse Practitioner (WHNP): An APRN specializing in the comprehensive care of women throughout their lives, focusing more on gynecology and primary care than deliveries. Their salaries are comparable to CNMs.
- Clinical Nurse Specialist (CNS): An MSN or DNP-prepared nurse who works as an expert clinician in a specialized area like perinatal care. They often serve as educators, consultants, and leaders within a hospital system, commanding salaries well over $115,000.
Professional Certifications: Beyond degrees, specialty certifications are a powerful way to validate your expertise and boost your income. The most recognized certification in obstetrics is the Inpatient Obstetric Nursing (RNC-OB®) from the National Certification Corporation (NCC). Earning this credential demonstrates a high level of knowledge and can lead to a direct salary increase or an annual bonus. Other valuable certifications include:
- Electronic Fetal Monitoring (C-EFM®): Essential for all L&D nurses.
- Neonatal Resuscitation Program (NRP): A required certification for working with newborns.
- Advanced Cardiovascular Life Support (ACLS): Often required for dealing with maternal emergencies.
### 2. Years of Experience
As detailed in the previous section, experience is a primary driver of salary growth. Hospitals use clinical ladders or career progression models to reward nurses for their developing expertise.
- New Graduate (0-1 year): Focus is on building core competencies. Salary is at the lower end of the pay scale.
- Competent Nurse (2-4 years): You are confident in your skills and can handle more complex patient assignments. This is typically when you see your first significant salary jumps.
- Proficient/Charge Nurse (5-10 years): You are a resource for the entire unit. You take on charge nurse duties (managing staffing and patient flow for a shift), precept new nurses, and participate in unit-based committees. Each of these responsibilities comes with a pay differential or leads to a promotion to a higher pay grade.
- Expert/Clinical Leader (10+ years): At this stage, you are a clinical authority. Your deep knowledge is highly valued, and your salary reflects this. Many nurses at this level transition into formal leadership (Nurse Manager), education (Clinical Educator), or advanced practice roles (CNM, CNS).
### 3. Geographic Location
Where you work is arguably the single biggest factor influencing your salary. Pay scales vary dramatically by state and even by metropolitan area, largely due to differences in cost of living, the strength of nursing unions, and regional demand.
Highest-Paying States for Registered Nurses: According to the BLS (May 2023 data), the top-paying states for RNs are consistently on the West Coast, with others in the Northeast and Alaska. OB nurses in these states can expect similarly high earnings.
| State | Annual Mean Wage (for all RNs) |
| :--- | :--- |
| California | $137,690 |
| Hawaii | $120,400 |
| Oregon | $113,440 |
| Washington | $111,030 |
| Alaska | $109,770 |
Highest-Paying Metropolitan Areas: Pay is often even higher in major cities within these states.
| Metropolitan Area | Annual Mean Wage (for all RNs) |
| :--- | :--- |
| San Jose-Sunnyvale-Santa Clara, CA | $180,010 |
| San Francisco-Oakland-Hayward, CA | $172,410 |
| Vallejo-Fairfield, CA | $166,460 |
| Napa, CA | $158,540 |
| Sacramento-Roseville-Arden-Arcade, CA | $154,160 |
In contrast, states in the Southeast and parts of the Midwest tend to have lower average salaries for nurses. However, the lower cost of living in these areas can sometimes offset the pay difference. An OB nurse earning $80,000 in Alabama may have a similar or even better quality of life than one earning $115,000 in California.
### 4. Work Setting & Employer Type
The type of facility you work in has a direct impact on your compensation and work environment.
- Large Academic Medical Centers & Unionized Hospitals: These facilities, often found in major cities, typically offer the highest pay scales, best benefits, and most opportunities for advancement. They often have strong nursing unions that negotiate for competitive wages, guaranteed raises, and strict nurse-to-patient ratios.
- Community Hospitals: Smaller, non-profit or for-profit community hospitals may have slightly lower base salaries but can offer a different work culture. They may offer attractive sign-on bonuses to compete for talent.
- Birthing Centers: Freestanding birthing centers provide a less medicalized, more holistic environment. Nurses here often work more closely with midwives. Salaries may be slightly lower than in a hospital setting, but the work-life balance can be a major draw for some.
- Private OB/GYN Practices: Nurses in physicians' offices assist with prenatal check-ups, patient education, and non-stress tests. The work is typically 9-to-5 with no weekends or holidays, but the pay is generally lower than in an inpatient hospital setting due to the lack of shift differentials and acuity.
- Government and Military: Working for the Department of Veterans Affairs (VA) or as a nurse in the U.S. military offers competitive, standardized pay scales and exceptional government benefits, including pensions and robust educational funding.
### 5. Area of Specialization within Obstetrics
While "OB Nurse" is a specialty, there are sub-specialties within the field that can affect pay and job duties.
- Labor & Delivery (L&D): This is the highest-acuity area. The fast pace, high stress, and need for critical thinking skills mean L&D nurses often have a slightly higher base pay or earn more through overtime and on-call work.
- Postpartum (Mother-Baby): This role focuses on recovery, education, and couplet care. The pace can be less frantic than L&D, though still very busy. Pay is generally comparable to other hospital floor nursing roles.
- Antepartum: This high-risk unit requires specialized knowledge of maternal-fetal complications. These are often highly skilled, experienced nurses whose pay reflects their expertise.
- Perinatal Float Pool: Some nurses choose to work in a float pool, covering L&D, postpartum, and the nursery. This requires a broad skill set and flexibility, which is often rewarded with a higher hourly "float differential."
### 6. In-Demand Skills and Competencies
Beyond formal education and certifications, developing specific, high-value skills can make you a more attractive candidate and command a higher salary.
- Charge Nurse/Leadership Experience: Demonstrating the ability to lead a team, manage patient flow, and handle staffing issues is a clear path to promotion and higher pay.
- Surgical First-Assist: In some states, experienced OB nurses can be trained to act as a surgical first-assistant during C-sections. This highly specialized skill comes with a significant pay increase.
- Advanced Fetal Monitoring Expertise: Being the unit's "go-to" expert for interpreting complex or concerning fetal monitoring strips is a highly valuable, though informal, skill.
- Bilingualism: In diverse communities, being fluent in a second language (especially Spanish) is a massive asset and may come with a pay differential.
- Technology Proficiency: Expertise with the specific Electronic Health Record (EHR) system used by the hospital (e.g., Epic, Cerner) and other medical technology makes you a more efficient and valuable team member.
Job Outlook and Career Growth

For anyone considering a long-term career as an obstetrics nurse, the job outlook is exceptionally positive. The demand for skilled registered nurses is projected to grow robustly over the next decade, driven by several demographic and healthcare trends.
### Strong Projected Job Growth
The U.S. Bureau of Labor Statistics (BLS) projects that overall employment for registered nurses will grow by 6 percent from 2022 to 2032, which is faster than the average for all occupations.
This translates to approximately 177,400 openings for registered nurses each year, on average, over the decade. Many of these openings are expected to result from the need to replace nurses who retire or transfer to different occupations.
Several factors specifically support the strong demand for OB nurses:
1. Consistent Birth Rates: While birth rates fluctuate, there is always a fundamental need for skilled professionals to care for birthing parents and newborns.
2. Increasing Complexity of Pregnancies: Trends such as rising maternal age and higher rates of chronic conditions like hypertension and diabetes mean that more pregnancies are considered high-risk, requiring specialized nursing care.
3. The Nursing Shortage and Retirements: A significant portion of the experienced nursing workforce is approaching retirement age. This "silver tsunami" will create a major vacuum of experienced OB nurses, increasing demand and creating opportunities for new and mid-career nurses to advance.
4. Focus on Reducing Maternal Mortality: With a growing national focus on improving maternal health outcomes and reducing mortality rates in the U.S., there is greater emphasis on and funding for high-quality, evidence-based obstetric care, which hinges on skilled nursing.
### Emerging Trends and Future Challenges
The field of obstetrics is not static. Aspiring and current nurses should be aware of the trends and challenges shaping the future of the profession:
Trends:
- Telehealth Integration: Telehealth is increasingly being used for routine prenatal check-ins, postpartum follow-ups, and patient education, creating new roles for nurses in virtual care.
- **