Introduction

For those drawn to medicine not just to extend life, but to profoundly improve its quality, the field of pain management represents a pinnacle of purpose and practice. Imagine a career where you are the specialist who gives a patient their life back—the ability to walk without a grimace, to play with their grandchildren, to sleep through the night. This is the daily reality for a pain management doctor. Beyond this immense personal fulfillment, the profession offers significant financial rewards, with the average pain management doctor salary often ranking among the highest in the medical field, typically ranging from $350,000 to over $600,000 annually.
I once spoke with a retired construction worker who had lived with debilitating back pain for over a decade, isolating him from his family and hobbies. After a successful spinal cord stimulator trial performed by his pain specialist, he described his first pain-free walk in the park as "being reborn." This single conversation cemented my understanding of this specialty's power: it is a unique intersection of advanced procedural skill, deep empathy, and life-altering impact.
This guide is designed to be your definitive resource, whether you are a medical student weighing specialties or a practicing physician considering a fellowship. We will delve into every facet of a pain management doctor's career, from the intricate details of their daily work to a comprehensive breakdown of salary data, the factors that drive compensation, and a step-by-step roadmap to entering this challenging and rewarding field.
### Table of Contents
- [What Does a Pain Management Doctor Do?](#what-does-a-pain-management-doctor-do)
- [Average Pain Management Doctor Salary: A Deep Dive](#average-pain-management-doctor-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Pain Management Doctor Do?

A pain management specialist, or algologist, is a physician who has undergone advanced fellowship training to evaluate, diagnose, and treat a wide spectrum of pain-related disorders. Their expertise is not limited to one area of the body but encompasses the complex physiological and psychological dimensions of pain itself. They are the detectives of the medical world, piecing together patient histories, physical exams, and advanced diagnostic imaging to uncover the root cause of suffering.
The core of their role is to create comprehensive, multimodal treatment plans that are highly individualized to the patient. This goes far beyond simply prescribing medication. A modern pain management practice is built on a foundation of interventional procedures, physical therapy, psychological support, and lifestyle modification.
Core Responsibilities and Daily Tasks:
- Patient Diagnosis and Consultation: Conducting thorough patient evaluations, including detailed medical histories, physical examinations, and reviewing MRIs, CT scans, and X-rays to identify the source of acute or chronic pain.
- Developing Treatment Plans: Creating tailored, long-term strategies that may include a combination of interventional procedures, non-opioid medications, referrals to physical or occupational therapy, and psychological counseling.
- Performing Interventional Procedures: This is a cornerstone of the specialty. Pain physicians perform a variety of minimally invasive, often image-guided (using fluoroscopy or ultrasound), procedures. Common examples include:
- Epidural steroid injections
- Nerve blocks and radiofrequency ablation
- Joint injections (hip, knee, shoulder)
- Spinal cord stimulator (SCS) trials and implants
- Kyphoplasty or vertebroplasty for spinal fractures
- Implantable pain pumps
- Medication Management: Prescribing and managing complex medication regimens, with a strong emphasis on non-opioid analgesics and responsible, guideline-driven use of opioids only when necessary.
- Patient Education: Empowering patients with knowledge about their condition, treatment options, and strategies for self-management to improve function and quality of life.
- Collaboration and Coordination of Care: Working as part of a multidisciplinary team with surgeons (orthopedic, neurosurgery), neurologists, physiatrists, primary care physicians, physical therapists, and psychologists to provide holistic care.
---
> ### A Day in the Life: Dr. Evelyn Reed, Interventional Pain Specialist
>
> 7:30 AM - 8:30 AM: Morning Huddle and Chart Review
> Dr. Reed arrives at her private practice, grabs a coffee, and meets with her nurse practitioner and medical assistant. They review the day's schedule, highlighting complex cases and ensuring all necessary pre-authorizations for procedures are in place. She reviews imaging and patient notes for the first few appointments.
>
> 8:30 AM - 12:00 PM: Procedure Block
> The morning is dedicated to interventional procedures in the in-office fluoroscopy suite.
> * 8:30 AM: A 68-year-old patient with lumbar spinal stenosis receives a fluoroscopy-guided epidural steroid injection.
> * 9:15 AM: A 45-year-old with chronic neck pain from facet joint arthritis undergoes a cervical radiofrequency ablation.
> * 10:30 AM: A 55-year-old with Complex Regional Pain Syndrome (CRPS) begins a spinal cord stimulator trial. Dr. Reed carefully places the temporary leads and ensures the patient feels the desired paresthesia covering their painful areas.
>
> 12:00 PM - 1:00 PM: Lunch and Administrative Tasks
> Dr. Reed dictates her procedure notes, returns urgent phone calls to referring physicians, and reviews lab results.
>
> 1:00 PM - 4:30 PM: Clinic Hours (Patient Consultations)
> The afternoon is for patient consultations.
> * 1:00 PM: A new patient consultation for a 38-year-old with severe sciatica. Dr. Reed performs a detailed exam and orders an MRI.
> * 1:45 PM: A follow-up with a patient two weeks post-procedure to assess their progress and adjust their physical therapy plan.
> * 3:00 PM: A long-term patient on a stable medication regimen comes in for their quarterly check-up and prescription renewal.
>
> 4:30 PM - 5:30 PM: Charting and Wrap-Up
> Dr. Reed completes all her electronic health records (EHR) for the day, signs off on her team's notes, and develops treatment plans for the new patients she saw. She leaves the office around 5:30 PM, fulfilled by the tangible difference she made in her patients' ability to function and live more comfortably.
---
Average Pain Management Doctor Salary: A Deep Dive
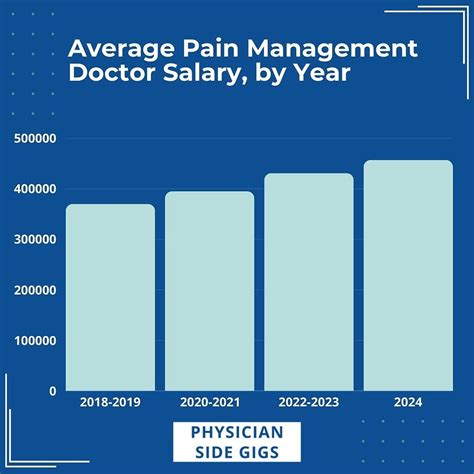
The salary for a pain management doctor is among the most competitive in the medical profession, reflecting the extensive training required and the high value of the procedural services they provide. Compensation is not a single number but a wide spectrum influenced by numerous factors, which we will explore in the next section.
It is crucial to consult multiple, high-authority sources for a balanced view, as methodologies can differ. Medical salary reports from organizations like Doximity, Medscape, and Merritt Hawkins are considered industry standards, supplemented by data from aggregators like Salary.com.
### National Average Salary and Range
According to the 2023 Doximity Physician Compensation Report, a premier source for physician salary data, the average annual compensation for the closely related field of Anesthesiology (from which many pain specialists originate) is $472,906. The report further notes that specialists who are more procedure-oriented tend to earn more. Pain management, with its heavy focus on interventions, often exceeds this average.
The Medscape Physician Compensation Report 2023 provides corroborating evidence. It lists Anesthesiology with an average salary of $448,000. However, industry experts and anecdotal data consistently place interventional pain management specialists in a higher bracket.
Based on an analysis of these reports and data from Salary.com, a realistic national average salary for a dedicated Pain Management Physician falls between $400,000 and $500,000.
- Salary.com (as of late 2023) reports a tighter median salary for a "Pain Management Physician" at $403,912, but shows a typical range extending from $340,361 to $529,144. The top 10% of earners in this field can easily surpass $600,000.
This wide range highlights the significant earning potential. The lower end typically represents physicians in academic settings or those with a less procedure-heavy practice, while the higher end reflects experienced physicians in private practice with high procedural volume.
### Salary by Experience Level
Like all professions, compensation in pain medicine grows substantially with experience, reputation, and efficiency. Here is a typical trajectory:
| Career Stage | Years of Experience (Post-Fellowship) | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Early Career | 1-5 Years | $300,000 - $425,000 | Recently completed fellowship. Often in a salaried hospital or group practice position, sometimes with a productivity bonus. Focus is on building a patient base and honing procedural skills and speed. |
| Mid-Career | 6-15 Years | $425,000 - $550,000 | Peak earning years. Established reputation leading to strong referral streams. High efficiency in performing procedures. May have achieved partnership in a private practice, leading to a share of profits. |
| Senior/Late Career| 16+ Years | $450,000 - $650,000+ | Highly respected expert in the field. May continue a high-volume practice or transition to a mix of clinical work, administrative leadership (e.g., medical director), or ancillary ventures (e.g., owning a surgery center). |
*Source: Analysis based on data from Doximity, Medscape, and Salary.com, synthesized with industry knowledge.*
### Deconstructing the Compensation Package
A pain management doctor's total earnings are rarely just a flat salary. The compensation package is a composite of several elements, especially in private practice.
- Base Salary: A guaranteed annual salary. This is the most common model for physicians employed by hospitals or large academic centers.
- Productivity Bonuses (RVU-Based): This is a critical component of many compensation models. Physicians earn Work Relative Value Units (wRVUs) for each service and procedure they perform. The wRVU value is set by Medicare and reflects the time, skill, and intensity required for a service. The physician is then paid a certain dollar amount per wRVU generated above a set threshold. This model directly rewards procedural volume and efficiency.
- *Example:* A physician might have a base salary of $300,000 and be paid $60 for every wRVU generated over 5,000 in a year. If they generate 8,000 wRVUs, they would earn an additional (3,000 wRVUs * $60/wRVU) = $180,000 bonus, for a total compensation of $480,000.
- Profit Sharing / Partnership Income: For physicians who are partners in a private practice, a significant portion of their income comes from a share of the practice's net profits. This offers the highest earning potential but also carries the risks and responsibilities of business ownership.
- Call Pay: Compensation for being on-call for hospital consults or emergencies after hours or on weekends. This is more common in hospital-employed positions.
- Ancillary Service Revenue: Practice owners can significantly increase their income through ancillary services, such as owning their own in-office procedure suite, ambulatory surgery center (ASC), physical therapy wing, or toxicology lab.
- Standard Benefits: In addition to direct compensation, packages almost always include:
- Malpractice Insurance: A crucial and expensive benefit.
- Health, Dental, and Vision Insurance.
- Retirement Plans: Such as a 401(k) or 403(b), often with a generous employer match.
- Continuing Medical Education (CME) Allowance: An annual stipend to cover the costs of conferences and courses needed to maintain medical licenses.
- Paid Time Off (PTO) and Sick Leave.
- Signing Bonuses and Relocation Assistance: Often offered to attract physicians to a new position, especially in less-populated areas.
Key Factors That Influence Salary

While the national averages provide a useful benchmark, a pain management doctor's actual salary is a dynamic figure shaped by a confluence of critical factors. Understanding these variables is key to maximizing earning potential throughout one's career. This is the most detailed part of our analysis, breaking down exactly what drives compensation up or down.
###
1. Level of Education and Board Certification
In medicine, the educational path is long and standardized, but key credentials significantly impact earning power and employability.
- The Fellowship is Non-Negotiable: To practice as a pain management specialist, a one-year, ACGME-accredited fellowship in Pain Medicine is mandatory. This occurs *after* completing a full residency.
- Primary Residency Matters: The most common residency pathways into a pain fellowship are Anesthesiology, Physical Medicine & Rehabilitation (PM&R), Neurology, and Psychiatry. While all can lead to a successful career, physicians from an Anesthesiology background often have a slight advantage in the job market, particularly for roles that are heavily procedural and hospital-based, due to their extensive training in advanced airway management, sedation, and perioperative care.
- Dual Board Certification is the Gold Standard: The single most important educational credential for maximizing salary is achieving board certification in both your primary specialty (e.g., Anesthesiology) and the subspecialty of Pain Medicine. Certification is granted by the American Board of Medical Specialties (ABMS) or the American Osteopathic Association (AOA). It signals the highest level of expertise to employers, insurance companies, and patients. Lacking this certification can severely limit job opportunities and result in lower reimbursement rates from insurers, directly impacting the revenue you can generate and thus your salary.
###
2. Years of Experience and Reputation
As detailed in the previous section, experience is a primary driver of salary growth. This isn't just about time served; it's about what that time develops.
- Early Career (1-5 Years): Focus is on efficiency. A new-in-practice physician might take 30 minutes for a procedure that a 10-year veteran can complete safely and effectively in 15 minutes. This increase in speed directly translates to higher patient volume and wRVU generation. Initial salaries might be lower, often with a partnership track offer after 2-3 years.
- Mid-Career (6-15 Years): This is the stage of peak productivity and reputation. A mid-career physician has a well-established network of referring doctors (primary care, surgeons, chiropractors) who trust their outcomes. They are efficient, experienced in handling complex cases, and if in private practice, are now likely a full partner, reaping the financial rewards of ownership. This is when salaries often peak.
- Late Career (16+ Years): While some physicians maintain a high clinical volume, many leverage their expertise in other ways. They may take on lucrative leadership roles like Department Chair or Medical Director of a hospital or surgery center. Others engage in consulting for medical device companies or start their own ancillary businesses, creating multiple streams of income that keep their total compensation very high, even if their clinical wRVUs decrease slightly.
###
3. Geographic Location
Location is arguably one of the most significant factors influencing physician salaries across all specialties, and pain management is no exception. Compensation varies dramatically by state and even between urban and rural areas within the same state.
- State-by-State Variation: According to the Doximity report, compensation is often highest in the Midwest and Southeast and lower in the Northeast and some areas of the West Coast. This is due to a combination of supply and demand, cost of living, and the local insurance reimbursement landscape.
- High-Paying States: States like Wisconsin, Indiana, Georgia, and parts of Texas and Florida often report higher-than-average physician salaries to attract and retain talent.
- Lower-Paying States: States like Maryland, Massachusetts, and Colorado, often with a high density of physicians and academic centers, may have salaries closer to or slightly below the national average.
- Metropolitan vs. Rural/Underserved Areas: This presents a classic trade-off.
- Major Metropolitan Areas (e.g., New York City, Los Angeles, Chicago): These areas have a high concentration of specialists, leading to more competition. While the cost of living is very high, physician salaries are not always proportionally higher and can sometimes be lower than in other regions.
- Rural and Medically Underserved Areas: To attract a highly trained specialist, hospitals and practices in these areas often offer significantly higher salaries, generous signing bonuses, and student loan repayment assistance. A physician might earn $50,000 to $100,000 more per year by choosing to practice in a smaller community over a major city.
###
4. Practice Type and Size
The setting in which a pain doctor works has a profound impact on their compensation structure and overall earning potential.
- Private Practice (Partner/Owner): This setting offers the highest income ceiling. Partners in a successful multi-physician pain practice, especially one that owns its own ambulatory surgery center (ASC), can earn well into the $750,000 to $1,000,000+ range. Their income is a direct result of the practice's profitability. However, this comes with the immense responsibilities of running a business: managing staff, marketing, billing and coding, and regulatory compliance.
- Hospital or Health System-Employed: This offers stability and security. The physician is a salaried employee with a predictable income, excellent benefits, and no administrative burden of running a practice. Malpractice insurance is covered, and there is a built-in referral base. The salary is typically very competitive, often in the $350,000 to $500,000 range, frequently with a productivity bonus structure. This is an attractive option for those who want to focus solely on clinical medicine.
- Academic Medical Center: This path prioritizes teaching, research, and treating complex cases over pure income maximization. Salaries at universities are almost always lower than in private or hospital-employed settings, often ranging from $275,000 to $400,000. The trade-off is the prestige, the opportunity to educate the next generation of doctors, protected time for research, and often a better quality of life with more reasonable hours and call schedules.
- Locum Tenens: This involves working as a temporary, independent contractor to fill in for other physicians. Pay rates are extremely high on a per-diem or weekly basis, but this does not include benefits like health insurance, retirement, or paid time off, which the physician must cover themselves.
###
5. Area of Specialization (Procedural Focus)
Within the field of pain management, the single biggest differentiator for income is the degree to which the practice is "interventional."
- High-Interventional Focus: Physicians who dedicate a significant portion of their practice to performing advanced, high-reimbursement procedures earn the most. These procedures generate high wRVUs. The most lucrative procedures include:
- Spinal Cord Stimulator (SCS) Implants: These are complex procedures used for neuropathic pain conditions and command the highest reimbursement.
- Vertebral Augmentation (Kyphoplasty/Vertebroplasty): Procedures to treat painful vertebral compression fractures.
- Intrathecal Pain Pump Implants: For cancer pain or severe spasticity.
- Advanced Radiofrequency Ablation Techniques: Such as cooled or genicular nerve RFA.
- A practice that is 70-80% interventional will generate far more revenue than one that is not.
- Medication Management and Consultative Focus: A practice that primarily involves consultations, medication management, and performing only basic injections (e.g., trigger point injections, basic joint injections) will have a significantly lower earning potential. While essential, these services are reimbursed at a much lower rate than advanced interventional procedures.
###
6. In-Demand Skills
Beyond the core competencies, certain skills can make a physician a more valuable asset to a practice or hospital, leading to higher compensation.
- Procedural Versatility and Expertise: Mastery of the full spectrum of pain procedures, from basic injections to the most advanced implantables. Expertise in using both fluoroscopy and ultrasound for guidance is highly desirable.
- Business Acumen: For those in or aspiring to private practice, understanding the business of medicine is paramount. Skills in financial management, contract negotiation with insurance companies, marketing, and operational efficiency can directly translate a well-run practice into higher personal income.
- Leadership and Administrative Skills: The ability to lead a department, manage a team of advanced practice providers (NPs/PAs), and ensure quality and safety compliance can lead to director-level positions with additional stipends and a higher base salary.
- Expertise in Regenerative Medicine: While many regenerative treatments (like PRP and stem cell injections) are still considered investigational and are often cash-based, having expertise in this growing area can attract a new patient demographic and create an additional revenue stream for a practice.
Job Outlook and Career Growth

For those investing the decade-plus of training required to become a pain management specialist, the long-term career outlook is exceptionally positive. The demand for skilled pain physicians is robust and projected to grow steadily over the next decade, driven by powerful demographic and healthcare trends.
### Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) groups pain management physicians under the broader category of "Physicians and Surgeons." According to the BLS's Occupational Outlook Handbook, employment for this group is projected to grow 3 percent from 2022 to 2032, which is about as fast as the average for all occupations. While this number may seem modest, it represents approximately 23,800 openings for physicians and surgeons projected each year, on average, over the decade.
However, the outlook for pain management specifically is likely much stronger than this general figure suggests due to several key factors:
1. An Aging Population: The baby boomer generation is entering its senior years, leading to a significant increase in the prevalence of age-related chronic pain conditions, such as degenerative disc disease, spinal stenosis, and osteoarthritis. This demographic shift is the single largest driver of demand for pain management services.
2. The Opioid Crisis and Shift in Treatment Philosophy: The national opioid crisis has fundamentally changed how pain is treated. There is immense pressure on the healthcare system to move away from long-term opioid prescribing and toward safer, more effective alternatives. Interventional pain specialists are at the forefront of this movement, offering minimally invasive procedures that can reduce or eliminate the need for opioids. This has made their expertise more critical—and in-demand—than ever before.
3. Technological Advancements: The continuous innovation in medical devices and procedures creates new and better ways to treat pain. Advancements in spinal cord stimulation (e.g., high-frequency and DTM stimulation), radiofrequency ablation technology, and minimally invasive spinal procedures mean that physicians can treat more conditions more effectively, expanding the patient population that can benefit from their care.
### Emerging Trends and Future Challenges
The field is not static. To thrive, physicians must stay ahead of emerging trends and navigate potential challenges.
**
