Introduction

Choosing a career in medicine is a monumental decision, often driven by a deep-seated desire to heal and make a difference. Yet, within the vast landscape of medical specialties, few are as profoundly impactful and deeply human as palliative care. If you are drawn to a path that prioritizes quality of life, compassionate communication, and holistic patient care in the face of serious illness, you may be considering becoming a palliative care physician. But alongside the immense personal and professional fulfillment this role offers, practical questions about financial viability and career trajectory are not just important—they are essential for long-term success and sustainability.
This guide is designed to be your comprehensive resource, exploring every facet of a palliative care physician salary and the career that commands it. We will move beyond a single number to dissect the complex factors that shape your earning potential, from your years of experience and geographic location to your practice setting and specialized skills. The national average salary for a palliative care physician is substantial, typically ranging from $200,000 to over $300,000 annually, reflecting the advanced training and critical expertise required.
I once sat with a family struggling with a devastating diagnosis. The air was thick with fear and unspoken questions. The palliative care physician who entered the room didn't just discuss treatment options; she listened, translated complex medical jargon into human terms, and helped the family define what a "good day" looked like for their loved one. In that moment, I saw firsthand that this specialty is not about giving up—it's about empowering patients and families to live as fully as possible, for as long as possible.
This article will provide the data, insights, and actionable steps you need to determine if this rewarding and challenging career is the right fit for you.
### Table of Contents
- [What Does a Palliative Care Physician Do?](#what-does-a-palliative-care-physician-do)
- [Average Palliative Care Physician Salary: A Deep Dive](#average-palliative-care-physician-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Palliative Care Physician Do?

A common misconception is that palliative care is synonymous with hospice or end-of-life care. While it includes hospice, its scope is far broader. Palliative care is specialized medical care for people living with serious illnesses, such as cancer, heart failure, COPD, kidney disease, Alzheimer's, or ALS. The primary goal is to provide relief from the symptoms and stress of the illness, with the overarching aim of improving quality of life for both the patient and their family. Crucially, it can be provided at any age and at any stage of an illness, often alongside curative treatment.
The palliative care physician acts as a master communicator, an expert symptom manager, and the leader of an interdisciplinary team. They are the bridge between the patient's goals and the medical team's treatment plan. Their responsibilities are a unique blend of art and science, requiring both deep medical knowledge and profound emotional intelligence.
Core Responsibilities Include:
- Symptom Management: Expertly treating pain, nausea, shortness of breath, fatigue, depression, anxiety, and other distressing symptoms associated with serious illness. This often involves complex pharmacology and a nuanced understanding of how treatments interact.
- Communication and Goal Setting: Facilitating difficult but essential conversations with patients and families. This includes clarifying the patient's understanding of their prognosis, exploring their values and care preferences, and establishing clear goals of care. They answer the question, "Given your medical situation, what is most important to you?"
- Interdisciplinary Team Leadership: Collaborating closely with and often leading a team that may include palliative care nurses, social workers, chaplains, pharmacists, and physical therapists. This team-based approach ensures that the patient's physical, emotional, social, and spiritual needs are all addressed.
- Care Coordination: Working with the patient's other doctors (like oncologists or cardiologists) to ensure that care plans are aligned, streamlined, and centered on the patient's goals. They help navigate the complexities of the healthcare system.
- Family and Caregiver Support: Recognizing that a serious illness affects the entire family unit. Palliative care physicians provide support, guidance, and resources for caregivers, helping to alleviate their burden and stress.
### A Day in the Life of a Hospital-Based Palliative Care Physician
To make this tangible, let's walk through a typical day:
- 8:00 AM - 9:00 AM: Team Huddle. The day begins with the interdisciplinary team. The physician, nurse practitioner, social worker, and chaplain review new consult requests and follow-up on existing patients. They discuss complex cases, share insights, and create a coordinated plan for the day. A patient's pain is still uncontrolled despite standard medication; the team decides the physician will assess for a nerve block. Another patient's family is conflicted about treatment; the social worker and physician will co-facilitate a family meeting.
- 9:00 AM - 12:30 PM: Patient Rounds. The physician sees patients throughout the hospital. One visit might involve adjusting a complex pain medication regimen for a cancer patient. The next could be a new consult for a patient in the ICU with heart failure, where the physician helps the family understand the trajectory of the illness and explore what "quality of life" means to them. Another visit might be a simple check-in to manage nausea for a patient undergoing chemotherapy.
- 12:30 PM - 1:30 PM: Documentation and Lunch. Charting is a critical part of the day. The physician meticulously documents conversations, symptom assessments, and changes to the care plan. This documentation is vital for communicating with the primary teams.
- 1:30 PM - 3:30 PM: Family Meetings and Consults. This time is often reserved for longer, more intensive conversations. The physician might lead a family meeting to establish goals of care, helping a family decide whether to pursue another round of aggressive treatment or shift focus to comfort. They may also see new patients referred from the emergency department.
- 3:30 PM - 5:00 PM: Follow-ups and Team Wrap-up. The physician follows up on any urgent issues from the morning, calls consulting specialists, and connects with the primary teams to provide recommendations. The day ends with a brief team check-in to ensure all tasks are completed and to plan for any overnight concerns.
This "day in the life" highlights the dynamic nature of the role—it is a demanding, intellectually stimulating, and emotionally resonant specialty that sits at the very heart of patient-centered care.
Average Palliative Care Physician Salary: A Deep Dive
Understanding the financial landscape of a palliative care career is a critical step in your professional journey. While the non-monetary rewards are immense, a competitive salary is essential for recognizing the extensive training required and for maintaining personal financial well-being. Palliative medicine physician salaries are robust and competitive with many other non-procedural internal medicine subspecialties.
It is important to note that palliative care is a subspecialty, meaning physicians first complete a residency in a field like Internal Medicine, Family Medicine, or Pediatrics before pursuing a fellowship. Therefore, their compensation is often benchmarked against these primary specialties, with an additional premium for their specialized expertise.
### National Average and Salary Range
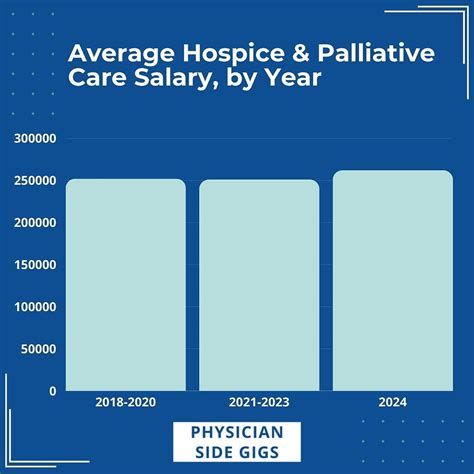
Salary data for palliative care physicians can vary slightly between reporting sources due to different methodologies, sample sizes, and demographics of the physicians surveyed. However, by triangulating data from several authoritative sources, we can establish a reliable picture.
- Salary.com reports the median salary for a Palliative Care Physician in the United States as $248,309 as of late 2023, with a typical range falling between $209,209 and $307,809. This represents the middle 50% of earners, meaning 25% earn less and 25% earn more.
- Medscape's 2023 Physician Compensation Report, while not having a separate category for Palliative Medicine, lists the average salary for Internists at $273,000 and Family Medicine physicians at $255,000. Palliative care physicians, with their additional fellowship training, typically earn within or slightly above these ranges, particularly when in high-demand settings.
- The 2023 Doximity Physician Compensation Report indicates that the average compensation for Internal Medicine is $293,000. Again, palliative care physicians fall within this specialty's umbrella and their salaries are comparable.
- Data from Merritt Hawkins, a leading physician recruiting firm, often shows palliative care salaries in the $230,000 to $280,000 range for staff physicians, with medical director roles commanding significantly more.
Taking a composite view, a realistic national average base salary for a palliative care physician in 2024 is approximately $250,000, with a broad range of $200,000 to $320,000+ depending on the factors we will explore below.
### Salary by Experience Level
Like any profession, compensation for palliative care physicians grows significantly with experience, expertise, and leadership responsibilities. The salary trajectory reflects a physician's increasing ability to handle complex cases, mentor junior colleagues, and take on administrative or program-building roles.
Here is a typical breakdown of how salary progresses throughout a career, based on aggregated data from industry reports and salary platforms:
| Career Stage | Years of Experience | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 Years | $200,000 - $240,000 | Recently completed fellowship. Focus is on clinical practice, building confidence in managing complex cases and navigating family dynamics. Often in a staff physician role within a hospital or academic setting. |
| Mid-Career | 4-10 Years | $240,000 - $280,000 | Established clinical expert. May take on roles like leading quality improvement projects, mentoring fellows, or serving as the lead physician for a specific unit (e.g., oncology palliative care). |
| Senior/Experienced | 11-20 Years | $270,000 - $310,000 | Recognized leader in the field. Often holds leadership positions, such as Associate Medical Director or Fellowship Program Director. May have a mix of clinical and administrative duties. |
| Late-Career/Leadership | 20+ Years | $300,000 - $350,000+ | Typically in senior leadership roles like Section Chief, Division Chief, or Medical Director of Palliative Care/Hospice for an entire health system. Focus is on strategic program growth, budgeting, and system-wide integration. |
### Breakdown of Compensation Components
The figure on your paycheck is more than just a base salary. A comprehensive compensation package for a palliative care physician often includes several other valuable components. When evaluating a job offer, it's crucial to look at the total rewards, not just the base number.
- Base Salary: This is the guaranteed annual income and forms the largest part of your compensation.
- Bonuses: These are common and can be structured in several ways:
- Productivity Bonus: Often tied to Relative Value Units (RVUs), which are a measure of physician work. While palliative care is less RVU-driven than procedural specialties, some systems use it to incentivize seeing a certain volume of patients.
- Quality Bonus: Increasingly common, these bonuses are tied to meeting specific quality metrics, such as patient satisfaction scores, documentation completion rates, or improvements in symptom control across a patient population.
- Performance Bonus: A discretionary bonus awarded by the employer based on overall performance, contributions to the team, and citizenship within the organization.
- Signing Bonus: A one-time, lump-sum payment offered to new physicians as an incentive to join an organization. These can range from $10,000 to $30,000 or more, especially in underserved areas.
- Retirement Benefits: This is a critical component of long-term financial health. Look for employer contributions to a 401(k) or 403(b) plan. A generous employer match (e.g., matching 50% or 100% of your contributions up to a certain percentage of your salary) can add tens of thousands of dollars to your nest egg each year.
- Health and Insurance Benefits: Comprehensive health, dental, and vision insurance are standard. Employers also typically provide life insurance and disability insurance (both short-term and long-term), which are essential protections for a physician's high income.
- Paid Time Off (PTO): This includes vacation days, sick leave, and holidays. A typical package for a physician is 4-6 weeks of PTO per year.
- CME Allowance: Continuing Medical Education (CME) is required for maintaining medical licensure. Employers provide an annual allowance, typically between $3,000 and $5,000, to cover the costs of conferences, courses, and medical journal subscriptions.
- Relocation Assistance: For physicians moving to a new city for a job, employers often offer a relocation package to cover moving expenses, which can be a significant financial benefit.
- Malpractice Insurance: The employer will provide comprehensive medical malpractice insurance coverage, a non-negotiable and essential benefit.
When all these elements are combined, the total compensation package for a palliative care physician can be significantly higher than the base salary alone suggests.
Key Factors That Influence Salary

While the national averages provide a useful benchmark, a palliative care physician's actual salary is determined by a complex interplay of several key variables. Understanding these factors will empower you to negotiate effectively, make strategic career choices, and maximize your earning potential over the long term. This is the most critical section for understanding the "why" behind the salary numbers.
###
1. Geographic Location
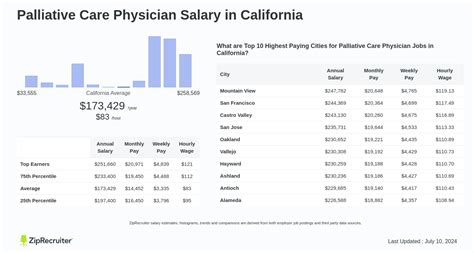
Where you practice medicine is arguably one of the most significant determinants of your salary. This variation is driven by supply and demand, cost of living, and the local healthcare market dynamics. High-paying regions often have a higher demand for specialists and a higher cost of living, while lower-paying areas may offer a more relaxed lifestyle but less competitive compensation.
According to data from physician compensation reports and salary aggregators, here is a general breakdown:
High-Paying States/Regions:
These areas often combine high demand with a high cost of living, leading to more competitive salaries to attract talent.
- The Midwest and Southeast: Surprisingly, some of the most competitive salaries for internists and related specialists are found in states like Alabama, Kentucky, Tennessee, and Oklahoma. Doximity's 2023 report consistently places these states in the top tier for physician compensation, driven by a high demand to serve large, aging populations in both rural and urban settings.
- The West (excluding coastal California): States like Arizona, Utah, and Nevada offer competitive salaries due to growing populations and a need for more specialists.
- Examples of High-Paying Metropolitan Areas: Cities like Charlotte, NC; St. Louis, MO; and Phoenix, AZ, often offer compensation packages that are higher than the national average when adjusted for cost of living.
Average-Paying States/Regions:
These regions typically offer salaries close to the national average.
- Texas, Florida, and parts of the Midwest (Ohio, Indiana): These states have large, robust healthcare systems and a steady demand for palliative care physicians, resulting in solid, predictable compensation.
- The Pacific Northwest (Oregon, Washington): Salaries here are strong but are often balanced by a very high cost of living, particularly in cities like Seattle and Portland.
Lower-Paying States/Regions:
These areas tend to have lower costs of living but also a higher concentration of physicians due to desirable locations or numerous academic training programs, which can suppress salaries.
- The Northeast (Maryland, Massachusetts, New York): These states, particularly in major metropolitan areas like Boston and New York City, have a high density of academic medical centers and physicians. While the nominal salaries may seem high, they often do not keep pace with the extremely high cost of living, making the effective take-home pay lower than in other regions. According to the Doximity report, Maryland, Massachusetts, and Washington D.C. are consistently among the lowest-paying areas for physicians.
- Coastal California: Similar to the Northeast, cities like Los Angeles and San Francisco have a high supply of physicians and an exceptionally high cost of living, which can temper salary growth.
Why does this variation exist?
- Supply and Demand: Rural areas and less "popular" states often have to pay more to attract highly specialized physicians.
- Payer Mix: The proportion of patients with private insurance versus Medicare/Medicaid in a given region affects hospital and practice revenue, which in turn influences physician salaries.
- Cost of Living: Employers in high-cost areas must offer higher nominal salaries, but these may not always translate to greater purchasing power.
###
2. Practice Setting (Employer Type)
The type of organization you work for has a profound impact on your salary, work environment, and day-to-day responsibilities.
- Large Hospital Systems (Private or Non-Profit): This is one of the most common employment models. These systems often offer competitive salaries, excellent benefits, and significant infrastructure support. Palliative care teams in large hospitals are typically well-integrated, handling inpatient consults, and may have an outpatient clinic. Compensation is often a combination of a base salary plus quality or productivity bonuses. These roles generally fall within the $230,000 - $290,000 range.
- Academic Medical Centers: Working for a university-affiliated hospital involves a tripartite mission: clinical care, teaching, and research. While the clinical work is similar to a community hospital, there is an added expectation to teach medical students, residents, and fellows, and potentially to conduct research. Base salaries in academia are traditionally slightly lower than in private practice or large community hospital systems, often in the $210,000 - $260,000 range. However, this is often offset by outstanding benefits, intellectual stimulation, and opportunities for career advancement through academic promotion.
- Private Practice (Physician-Owned Groups): While less common for palliative care than for other specialties, some physicians work in or own private palliative medicine groups. This model offers the highest potential for income, as you are a business owner. However, it also comes with the greatest risk and administrative burden, including managing staff, billing, and overhead. Income can vary widely, but successful private practice owners can potentially earn $350,000+.
- Hospice Organizations: Many palliative care physicians split their time between inpatient palliative consults and serving as a hospice medical director. Roles within large, well-funded non-profit or for-profit hospice agencies can be very competitive, often with salaries in the $240,000 - $300,000 range, especially for leadership positions.
- Veterans Affairs (VA) Hospitals: The VA is a major employer of palliative care physicians. VA salaries are determined by a national pay scale and are generally competitive, with excellent federal benefits, including a generous pension plan. The pace can be less hectic than in the private sector, and there is a strong sense of mission. Salaries are often in the $220,000 - $270,000 range.
###
3. Leadership and Administrative Roles
One of the most direct ways to increase your salary is to move beyond a purely clinical role and take on leadership responsibilities. These positions command higher pay due to their increased scope of responsibility, which includes strategic planning, program development, budgeting, and staff management.
- Staff Physician: The baseline role with purely clinical duties.
- Lead Physician: An experienced physician who provides clinical leadership for a specific team or service line without formal administrative title. This may come with a small stipend.
- Medical Director of Palliative Care: This is a common leadership role responsible for the clinical and operational oversight of a palliative care program within a hospital or clinic. This role typically carries a salary premium of $20,000 to $50,000 over a staff physician role.
- Hospice Medical Director: Responsible for the medical component of a hospice agency, including certifying patient eligibility and overseeing care plans. This is a significant leadership position with commensurate pay.
- Division Chief or Section Head of Palliative Medicine: In a large academic center or health system, this senior leader oversees the entire palliative care division, including clinical services, education (like the fellowship program), and research. These roles are among the highest-paid, often reaching $300,000 to $350,000 or more.
###
4. Sub-Specialization and Niche Expertise
While Hospice and Palliative Medicine (HPM) is already a subspecialty, developing a niche *within* it can increase your value and earning potential.
- Pediatric Palliative Care: This is a highly specialized and underserved field. Physicians trained in both pediatrics and HPM are rare and in high demand, which can lead to more competitive salary negotiations, particularly at major children's hospitals.
- Outpatient Palliative Care: As palliative care moves "upstream," there is a massive growth in outpatient clinics, particularly those embedded within cancer centers or heart failure clinics. Physicians with experience in building and running successful outpatient programs are highly sought after.
- Expertise in Interventional Pain Management: Palliative care physicians who have additional training or expertise in specific interventional pain procedures (though this often requires a separate pain fellowship) can command higher salaries.
###
5. Level of Education and Board Certification
For any physician, the educational path is long and standardized: an undergraduate degree, a medical degree (MD or DO), residency, and fellowship. The key differentiator for palliative care physicians is the fellowship and subsequent board certification.
- Board Certification in HPM: Being board-certified in Hospice and Palliative Medicine is the gold standard and a non-negotiable requirement for most high-quality jobs. It signifies that you have met rigorous standards of training and knowledge. Lack of board certification would significantly limit your job prospects and salary potential.
- Dual Boarding: Being board-certified in your primary specialty (e.g., Internal Medicine) *and* in HPM is the standard expectation and is priced into the salary ranges discussed.
###
6. In-Demand Skills (Beyond the Clinical)
In today's value-based healthcare environment, skills that go beyond clinical acumen are increasingly valued and can impact compensation, particularly through quality bonuses or promotion opportunities.
- Exceptional Communication Skills: The ability to navigate highly emotional conversations with empathy and clarity is the cornerstone of the specialty. While a "soft skill," it is a core competency that differentiates an average physician from a great one.
- Program Development and Quality Improvement: Physicians who can demonstrate a history of building programs (e.g., launching a new outpatient clinic) or leading successful quality improvement projects (e.g., reducing hospital length-of-stay for palliative patients) are seen as more valuable assets.
- Business Acumen: Understanding billing, coding, and the financial aspects of a palliative care service line is a huge advantage, especially for those aspiring to leadership roles.
- Telehealth Proficiency: The ability to effectively deliver palliative care consultations via video is a growing and valuable skill, allowing programs to expand their reach to rural or homebound patients.
By strategically developing these skills and considering the geographic and practice setting that aligns with your personal and financial goals, you can actively shape a successful and lucrative career in this vital field.
Job Outlook and Career Growth

The demand for palliative care physicians is not just strong; it is projected to grow dramatically in the coming years. This robust job outlook is fueled by powerful demographic and healthcare trends, making it one of the most secure and opportunity-rich fields in medicine for the foreseeable future.
### Overwhelming Demand, Limited Supply
The core driver of the exceptional job outlook is a simple economic principle: a widening gap between demand and supply.
Demand-Side Drivers:
1. The Aging Population: The U.S. Census Bureau projects that by 2030, all baby boomers will be older than 65, and older adults will outnumber children for the first time in U.S. history. This "silver tsunami" means a massive increase in the number of people living with multiple, complex, and chronic serious illnesses—the exact patient population that benefits most from palliative care.
2. Increased Awareness and Acceptance: Palliative care has successfully shed much of its former stigma of being only for the dying. Referring physicians, patients, and families now better understand its role in improving quality of life alongside curative treatments. This has led to an explosion in consultation requests.
3. Proven Value to Health Systems: Numerous studies have demonstrated that palliative care is not just good for patients; it's good for hospitals. Well-integrated palliative care programs have been shown to reduce hospital costs, decrease length of stay, lower readmission rates, and improve patient satisfaction scores. As health systems shift toward value-based care models, palliative care is no longer seen as a luxury but as a financial and clinical necessity.
Supply-Side Constraints:
1. Limited Training Slots: While growing, the number of HPM fellowship positions in the United States is insufficient to meet the projected demand. According to the American Academy of Hospice and Palliative Medicine (AAHPM), there is a significant workforce shortage.
2. An Aging Workforce: A substantial portion of the current palliative care physician workforce is itself nearing retirement age, which will further exacerbate the shortage.
3. The "Leaky Pipeline": The path to becoming a palliative care physician is long (4 years of medical school, 3+ years of residency, 1 year of fellowship), and burnout is a real concern in this emotionally demanding field, leading to some physicians leaving the specialty.
The U.S. Bureau of Labor Statistics (BLS) does not track palliative care physicians separately, but it groups them under "Physicians and Surgeons, All Other." The outlook for this general group is a growth of 3% between 2022 and 2032, which is about average. However, this broad statistic masks the acute reality within the specialty. Industry experts and professional organizations like the Center to Advance Palliative Care (CAPC) consistently report that the demand for palliative specialists far outstrips the BLS average for physicians as a whole, with many hospitals having multiple, difficult-to-fill openings.
### Emerging Trends and Future Opportunities
The field of palliative care is not static. Several emerging trends are shaping the future of the profession and creating new avenues for career growth.
- Upstream Integration: The biggest trend is the shift of palliative care "upstream"—introducing it earlier in the course of a serious illness, often at the time of diagnosis in an outpatient setting. This creates a huge demand for physicians to staff and lead ambulatory palliative care clinics, especially those embedded in oncology, cardiology, pulmonology, and neurology practices.
- Telepalliative Care: The COVID-19 pandemic accelerated the adoption of telehealth, and it has proven to be a highly effective model for many aspects of palliative care. It allows specialists to reach patients in rural areas, consult with nursing homes, and provide follow-up care for homebound patients, dramatically expanding the reach and efficiency of palliative services.
- Specialization in Non-Cancer Illnesses: While palliative care has deep roots in oncology, there is a growing need for expertise in managing non-cancer illnesses like advanced heart failure, COPD, dementia, and end-stage renal disease. Physicians who develop this expertise will be in high demand.
- Community-Based Palliative Care: The future of healthcare is moving out of the hospital and into the community. There are burgeoning opportunities in developing and leading community-based palliative care programs that provide services in patients' homes, long-term care facilities, and other settings. This is a frontier for innovation in the field.
### How to Stay Relevant and Advance Your Career
In such a dynamic and growing field, continuous learning and strategic career planning are key.
1. Embrace Lifelong Learning: Stay current not only on clinical advances in symptom management but also on healthcare policy, new care delivery models, and quality improvement methodologies.
2. Develop Leadership Skills: Seek out opportunities to lead, even on a small scale. Volunteer to chair a committee, lead a quality improvement project, or mentor a trainee. These experiences build the foundation for future leadership roles.
3. Cultivate a Niche: Become the go-to expert in a specific area, whether it's outpatient clinic development, pediatric palliative care, or managing the palliative needs of dementia patients.
4. Network and Engage: Actively participate in professional organizations like the A