For those driven by a profound desire to heal and a fascination with the intricate workings of the human body, a career in medicine is a natural calling. But for a select few, this calling narrows to a highly specialized and deeply impactful field: pediatric gastroenterology. It’s a career that combines the intellectual rigor of internal medicine, the technical skill of a surgeon, and the compassionate patience required to care for the youngest and most vulnerable patients. If you're considering this demanding yet incredibly rewarding path, one of your primary questions is likely about compensation and long-term viability. This guide is designed to answer that question and many more.
While the emotional and intellectual rewards are immeasurable, the financial compensation is also significant, reflecting the years of intensive training and the critical nature of the work. A pediatric gastroenterologist's salary typically ranges from $250,000 to well over $400,000 annually, with top earners in high-demand areas exceeding this. I once spoke with a seasoned pediatric GI who shared a story not about a complex procedure, but about the simple, profound joy on a parent's face when their child, who had been in constant, unexplained pain for years, finally ate a meal and smiled. It’s in those moments, she explained, that the true "value" of the profession is realized—a value that transcends any paycheck but is rightly supported by a competitive one.
This comprehensive article will serve as your definitive resource on the pediatric gastroenterologist salary, career outlook, and the steps required to enter this esteemed profession. We will delve into the granular data, explore the factors that dictate earning potential, and provide a clear roadmap for your journey ahead.
### Table of Contents
- [What Does a Pediatric Gastroenterologist Do?](#what-does-a-pediatric-gastroenterologist-do)
- [Average Pediatric Gastroenterologist Salary: A Deep Dive](#average-pediatric-gastroenterologist-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Pediatric Gastroenterologist Do?

A pediatric gastroenterologist is a highly specialized medical doctor who focuses on the diagnosis, treatment, and management of diseases concerning the gastrointestinal (GI) tract, liver, and pancreas in children, from newborns to young adults. Their scope is vast, addressing everything from common issues like chronic constipation and reflux to life-altering conditions such as Crohn's disease, ulcerative colitis, celiac disease, and liver failure.
This specialty is unique in its blend of cognitive and procedural medicine. A pediatric GI must be an astute diagnostician, piecing together clues from patient histories, physical exams, and complex lab results. They are "medical detectives" for a patient population that often cannot articulate its own symptoms clearly. Simultaneously, they are skilled technicians, performing intricate, minimally invasive procedures like endoscopies and colonoscopies to visualize the GI tract, obtain biopsies, and sometimes perform therapeutic interventions.
Core Responsibilities and Daily Tasks:
- Diagnosis and Management: Evaluating and treating a wide array of conditions, including inflammatory bowel disease (IBD), eosinophilic esophagitis, food allergies, short bowel syndrome, chronic diarrhea, abdominal pain, and feeding disorders.
- Procedural Work: Performing upper endoscopies (examining the esophagus, stomach, and duodenum) and colonoscopies (examining the large intestine). This can also include more advanced procedures like video capsule endoscopy or polypectomy (removing polyps).
- Nutritional Support: Managing complex nutritional needs for children who cannot eat normally, often involving feeding tubes or intravenous nutrition (Total Parenteral Nutrition - TPN).
- Hepatology (Liver Care): Diagnosing and managing liver diseases such as cholestasis, autoimmune hepatitis, and fatty liver disease, and often working with transplant teams for children requiring liver transplantation.
- Patient and Family Counseling: A significant part of the job involves educating and supporting families. They explain complex diagnoses, outline long-term treatment plans, and provide guidance on diet and lifestyle, which is crucial for managing chronic GI conditions.
- Collaboration: Working as part of a multidisciplinary team that can include pediatric surgeons, dietitians, social workers, psychologists, and other subspecialists.
- Research and Academics: Many pediatric gastroenterologists, especially those in academic medical centers, are actively involved in clinical research, teaching medical students and residents, and publishing scientific papers to advance the field.
### A Day in the Life: An Illustrative Example
To make this role more tangible, consider a typical day for a pediatric gastroenterologist in a hospital-based practice:
- 7:00 AM - 8:30 AM: Hospital Rounds. The day begins at the hospital, rounding on inpatients. This might include a teenager having a severe Crohn's disease flare-up, a toddler admitted for "failure to thrive" who needs a nutritional plan, and a newborn with a complex liver condition. The doctor reviews charts, checks lab results, examines the patients, and discusses the plan of care with the nursing staff and resident physicians.
- 8:30 AM - 12:00 PM: Outpatient Clinic. The scene shifts to the outpatient clinic. Here, the doctor sees a series of scheduled patients. Appointments could range from a 15-minute follow-up for a child with well-managed celiac disease to a 60-minute new patient consultation for a child with debilitating, undiagnosed abdominal pain. This part of the day is fast-paced and requires exceptional communication skills.
- 12:00 PM - 1:00 PM: Lunch & Administrative Tasks. This hour is often a working lunch, used for catching up on charting, answering emails from concerned parents, and coordinating care with other specialists via phone or the electronic medical record (EMR).
- 1:00 PM - 4:00 PM: Procedure Block. The afternoon is dedicated to procedures in the endoscopy suite. The doctor might perform two upper endoscopies and a colonoscopy. Each procedure involves a pre-procedure consultation with the family, performing the scope with an anesthesiology team, and a post-procedure discussion to explain the initial findings.
- 4:00 PM - 6:00 PM: Charting and Follow-up. The final hours are spent completing detailed procedure reports, updating patient charts from the morning clinic, reviewing biopsy results as they come in, and returning urgent phone calls. For those in academic medicine, this time might also be dedicated to research protocols or preparing for a lecture.
This "typical" day highlights the dynamic nature of the profession—a constant shift between deep analytical thinking, technical procedural skill, and empathetic human connection.
Average Pediatric Gastroenterologist Salary: A Deep Dive
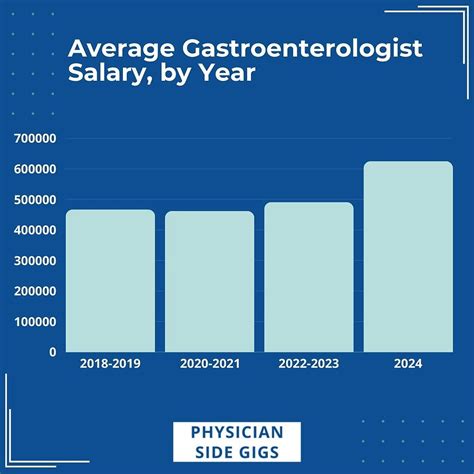
The journey to becoming a pediatric gastroenterologist is long and arduous, requiring at least 14 years of post-secondary education and training. The compensation for this level of expertise is, accordingly, among the highest in the medical field. While salary figures can vary significantly based on the factors we'll explore in the next section, we can establish a clear and data-backed baseline for what a professional in this field can expect to earn.
According to the most recent physician compensation surveys, the national average salary for a pediatric gastroenterologist falls between $280,000 and $350,000 per year.
Let's break this down with data from reputable sources:
- Medscape's 2023 Physician Compensation Report, a highly respected industry benchmark, places the average salary for general Gastroenterologists at $501,000. However, it's crucial to note that pediatric subspecialists often earn slightly less than their adult-focused counterparts due to differences in procedure volume and reimbursement rates. Based on this, and data from other aggregators, a more realistic range for pediatrics is derived.
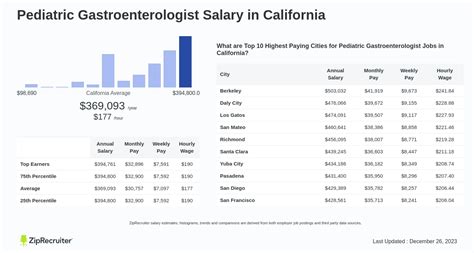
- Salary.com reports the median salary for a Pediatric Gastroenterologist in the United States as $299,107 as of late 2023, with a typical range falling between $254,166 and $356,862.
- Doximity's 2023 Physician Compensation Report indicates that pediatric subspecialties have seen significant growth in compensation. While it doesn't always break out pediatric gastroenterology specifically, its data on related fields and overall pediatric subspecialist trends supports an average in the low-to-mid $300,000s.
It is essential to understand that the "average" salary is just a midpoint. The actual take-home pay can be significantly influenced by experience, location, and practice setting.
### Salary by Experience Level
A physician's salary is not static; it grows substantially from the conclusion of fellowship to the peak of their career.
| Career Stage | Years of Experience | Typical Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level (Post-Fellowship) | 0-3 years | $230,000 - $280,000 | Initial positions, often in academic centers or as salaried employees in larger groups. Focus is on building a patient panel. |
| Mid-Career | 4-10 years | $280,000 - $360,000 | Increased efficiency, established reputation, and potential for partnership track in private practice. May take on minor leadership roles. |
| Senior/Experienced | 11-20+ years | $350,000 - $450,000+ | Peak earning years. Often partners in private practice or senior faculty/division chiefs in academic settings. High patient volume and procedural efficiency. |
*(Source: Data compiled and synthesized from Salary.com, Medscape, and anecdotal reports from physician recruiting agencies.)*
### A Closer Look at the Compensation Package
The annual salary figure is only one part of the total compensation story. A comprehensive package for a pediatric gastroenterologist often includes several other valuable components.
- Base Salary: This is the guaranteed income you receive, regardless of patient volume. In academic or hospital-employed models, this makes up the bulk of compensation.
- Production Bonus (RVU-Based): This is a critical component, especially in private practice and many hospital-employed models. Compensation is tied to Relative Value Units (RVUs), a measure used by Medicare to determine the value of physician services. Every procedure, consultation, and hospital visit is assigned an RVU value. The more patients a doctor sees and the more procedures they perform, the more RVUs they generate, leading to a higher bonus. This model directly incentivizes productivity.
- Signing Bonus: To attract top talent in a competitive market, many hospitals and private groups offer a one-time signing bonus. This can range from $15,000 to $50,000 or more.
- Relocation Allowance: To help with the cost of moving, employers often provide a relocation stipend, which can be a lump sum or a reimbursement-based package.
- Retirement Benefits: This almost always includes a 401(k) or 403(b) plan, often with a generous employer match (e.g., 3-6% of salary). In some academic or hospital systems, a pension plan may also be offered.
- Health and Disability Insurance: Comprehensive health, dental, vision, and life insurance are standard. Critically, high-quality long-term disability insurance is a non-negotiable part of a physician's benefits package to protect their high income in case of illness or injury.
- Malpractice Insurance: The employer almost universally covers the cost of medical malpractice insurance, which is substantial in a procedural specialty. It's important to know whether this is "claims-made" or "occurrence" coverage and who pays for the "tail" coverage if you leave.
- Continuing Medical Education (CME) Stipend: Physicians are required to complete a certain number of hours of continuing education each year to maintain their license. Employers typically provide an annual stipend of $2,000 to $5,000 and paid time off to attend conferences or workshops.
- Paid Time Off (PTO): This typically ranges from 4 to 6 weeks per year, covering vacation and sick leave.
When evaluating a job offer, it's crucial to look beyond the base salary and assess the total value of the entire compensation and benefits package. A slightly lower base salary at an institution with a generous retirement match and excellent benefits may be more valuable long-term than a higher salary with a weak benefits package.
Key Factors That Influence a Pediatric Gastroenterologist Salary

The wide salary ranges presented above are not arbitrary. They are the result of a complex interplay of several key factors. For anyone aiming to maximize their earning potential in this field, understanding these variables is paramount. This section provides a granular breakdown of what drives a pediatric gastroenterologist's salary up or down.
###
The Impact of Geographic Location
Where you choose to practice is arguably one of the most significant determinants of your salary. The principle of supply and demand is in full effect in the physician job market. Areas that are less "desirable" to live in or have a greater shortage of specialists must offer higher salaries to attract talent. Conversely, major metropolitan areas with numerous academic centers and a high quality of life may have more competition for jobs, which can temper salary offers.
High-Paying Regions:
- The Southeast and Midwest: States in these regions consistently offer higher-than-average compensation for medical specialists. This is due to a large patient population, fewer specialists per capita, and a favorable payer mix. States like Alabama, Kentucky, Indiana, and Oklahoma often appear on lists of top-paying states for physicians.
- Rural and Underserved Areas: Hospitals in smaller cities or rural locations struggle the most to recruit subspecialists. To compensate, they offer aggressive salaries, substantial loan repayment programs (sometimes from state or federal grants), and large signing bonuses. A pediatric gastroenterologist might earn 20-30% more in a non-metropolitan setting in the Midwest than in a major coastal city.
Lower-Paying (but still high) Regions:
- The Northeast and West Coast: Major cities like Boston, New York City, San Francisco, and Los Angeles are saturated with prestigious academic medical centers. The allure of living in these cities and the prestige of working at these institutions means they don't have to compete as heavily on salary. While the raw dollar amount is still high, the cost of living in these areas is often dramatically higher, meaning the effective take-home pay can be lower than in other regions.
Illustrative State-by-State Salary Variation (for general physicians, trends apply to specialists)
| State | Average Physician Salary (All Specialties) | Cost of Living Index | Notes |
| :--- | :--- | :--- | :--- |
| Wisconsin | ~$397,000 | 97.9 | High pay, reasonable cost of living. |
| Indiana | ~$380,000 | 90.6 | Excellent earning potential relative to expenses. |
| Georgia | ~$375,000 | 92.4 | Strong demand in a growing state. |
| California | ~$360,000 | 139.8 | High salary but eroded by extremely high cost of living. |
| New York | ~$350,000 | 126.5 | Similar to California, especially in the NYC metro area. |
| Maryland | ~$320,000 | 111.4 | Saturated market due to proximity to D.C. and major academic centers. |
*(Source: Data trends compiled from Doximity, Medscape, and World Population Review Cost of Living data.)*
The takeaway is clear: being geographically flexible can unlock significantly higher earning potential and a faster path to financial independence.
###
Practice Setting: Academic vs. Private Practice vs. Hospital-Employed
The type of organization you work for creates distinctly different career paths and compensation structures. This is perhaps the most critical choice a physician makes after fellowship.
1. Academic Medical Centers:
- Description: These are universities and their associated teaching hospitals. The mission is a "tripartite" one: clinical care, education, and research.
- Salary Structure: Typically a fixed base salary with smaller, more structured bonuses. The base salary is generally lower than in private practice. Compensation is often determined by academic rank (Instructor, Assistant Professor, Associate Professor, Full Professor).
- Pros:
- Prestige and intellectual stimulation.
- Opportunities to teach medical students, residents, and fellows.
- Protected time for research, with access to institutional resources and grants.
- Often better benefits, including more generous retirement plans and sometimes tuition benefits for children.
- Typically a more predictable schedule and call burden.
- Exposure to the most complex and rare "zebras" of the medical world.
- Cons:
- Lower overall earning potential.
- Slower career progression, often tied to a "publish or perish" academic promotion track.
- Can be more bureaucratic and less autonomous than private practice.
2. Private Practice:
- Description: A business owned by one or more physicians. This can be a single-specialty group (only pediatric GIs) or a large multi-specialty group. The focus is primarily on efficient and high-quality clinical care.
- Salary Structure: This model offers the highest earning potential. Typically, a physician starts with a guaranteed salary for 1-2 years. After this period, they move to a production-based model (100% RVUs) and become eligible for partnership. As a partner, they share in the profits of the entire practice, including ancillary services like an in-house infusion center or pathology lab.
- Pros:
- Highest income ceiling. A partner in a successful private practice can earn well over $450,000 - $500,000.
- Greater autonomy in clinical and business decisions.
- Direct financial reward for hard work and efficiency.
- Cons:
- Requires business acumen. You are not just a doctor; you are a small business owner.
- Higher personal financial risk. Income can fluctuate with patient volume and insurance reimbursement rates.
- Responsible for administrative burdens: hiring staff, managing payroll, dealing with billing and collections.
- Call burden can be more demanding, especially in a smaller group.
3. Hospital-Employed (Non-Academic):
- Description: This is a hybrid model that has become increasingly common. The physician is a direct employee of a hospital or a large, integrated healthcare system.
- Salary Structure: A blend of the academic and private models. There's a competitive base salary, often higher than in academia, coupled with a production bonus based on RVUs. It provides security without sacrificing productivity incentives entirely.
- Pros:
- Strong, competitive salary with less risk than private practice.
- Relief from administrative and business burdens; the hospital handles billing, staffing, and overhead.
- Stable work environment with predictable schedules and excellent benefits.
- Built-in referral network from the hospital's primary care physicians.
- Cons:
- Less autonomy than private practice. You must abide by the hospital's rules, use its EMR, and follow its protocols.
- Earning potential is capped and generally lower than a successful private practice partner.
- Can feel like a "cog in a machine" in very large health systems.
###
Years of Experience and Career Progression
As detailed in the salary table, experience is a powerful driver of income. This isn't just about annual raises; it's about a fundamental shift in a physician's value and role.
- Early Career (Years 0-3): The focus is on building clinical speed and confidence. You are establishing a reputation among referring pediatricians. Your salary is often guaranteed as you ramp up your practice.
- Mid-Career (Years 4-10): You are now a highly efficient clinician. In a private practice setting, this is when you become a partner, and your income sees a significant jump as you begin sharing in the group's profits. In an academic setting, you may be promoted to Associate Professor, which comes with a salary increase and potentially leadership roles like clinic director or fellowship program director.
- Late Career (Years 11+): You are a senior figure. Your reputation drives complex referrals. In private practice, you are a senior partner, reaping the rewards of a practice you helped build. In academia, you may be a Division Chief or Department Chair, roles that come with significant administrative stipends on top of your clinical salary.
###
Sub-Specialization and Niche Expertise
While pediatric gastroenterology is already a specialty, further sub-specialization can impact earning potential, primarily by driving a higher volume of specific, high-value referrals and procedures.
- Advanced/Therapeutic Endoscopy: Some pediatric GIs complete a fourth year of fellowship training in advanced procedures like Endoscopic Retrograde Cholangiopancreatography (ERCP) and Endoscopic Ultrasound (EUS). These are complex, high-RVU procedures, and physicians with these skills are in high demand, commanding a salary premium.
- Hepatology (Liver Disease): Specialists who focus on pediatric liver disease, particularly those affiliated with a liver transplant center, manage incredibly complex patients. Their expertise is rare and highly valued.
- Inflammatory Bowel Disease (IBD): Creating a dedicated IBD center can be very successful. It often involves managing patients on high-cost biologic infusions, which can be a significant revenue source for a practice with its own infusion center.
- Motility Disorders: Focusing on complex motility issues (e.g., gastroparesis, pseudo-obstruction) requires specialized diagnostic equipment and expertise, attracting referrals from a wide geographic area.
###
In-Demand Skills: Procedural vs. Clinical
Ultimately, a pediatric gastroenterologist's salary, particularly in production-based models, is heavily influenced by the services they provide.
- Procedural Volume and Efficiency: The ability to perform procedures like endoscopies and colonoscopies safely and efficiently is a direct driver of revenue. A doctor who can comfortably perform 10-12 procedures in a day will generate significantly more RVUs than one who does 5-6.
- Leadership and Administrative Skills: Taking on roles like Medical Director of the Endoscopy Unit, Division Chief, or serving on key hospital committees often comes with an administrative stipend. This can add $10,000 to $75,000+ to an annual salary, depending on the scope of the responsibility.
- Research Acumen: In academia, the ability to secure external grant funding (e.g., from the National Institutes of Health - NIH) is highly prized. A portion of the grant money can be used to cover the researcher's salary (known as "buying down your time"), freeing them from some clinical duties and increasing their value to the institution.
Job Outlook and Career Growth

For those investing nearly a decade and a half in training, the long-term career outlook is a critical consideration. The good news is that the demand for pediatric gastroenterologists, and physicians in general, is robust and projected to grow significantly.
The U.S. Bureau of Labor Statistics (BLS) projects that employment for all physicians and surgeons will grow by 3% from 2022 to 2032, which is about as fast as the average for all occupations. However, this overall number masks a more urgent need within specific subspecialties. The Association of American Medical Colleges (AAMC) continues to project a significant physician shortage over the next decade, driven by an aging population (which increases the need for all types of doctors) and a large number of physicians nearing retirement age.
For pediatric gastroenterology specifically, the demand is fueled by several powerful trends:
- Increasing Prevalence of Chronic GI Conditions: There is a well-documented rise in the incidence and prevalence of conditions like inflammatory bowel disease (Crohn's and ulcerative colitis), eosinophilic esophagitis, celiac disease, and food allergies in children. These are chronic, lifelong conditions that require continuous management by a specialist.
- Advances in Diagnosis and Treatment: Decades ago, many GI conditions in children were either misdiagnosed or untreatable. Today, with advanced diagnostic tools and revolutionary treatments like biologic therapies, more children are being accurately diagnosed and are living longer, healthier lives, which paradoxically increases