Introduction

In the intricate and high-stakes world of modern medicine, few roles carry the weight, responsibility, and profound impact of a critical care doctor. These physicians, also known as intensivists, are the steadfast guardians of the Intensive Care Unit (ICU), navigating the turbulent waters of life-threatening illnesses and injuries. They are the leaders of a highly-specialized team, making split-second decisions that can alter the course of a human life. For those drawn to the intellectual challenge, the procedural mastery, and the deep, human connection of this specialty, the question of compensation is a practical and crucial consideration. A career as a critical care doctor is not only one of the most demanding in medicine, but it is also one of the most financially rewarding, with average salaries often ranging from $350,000 to well over $500,000 annually.
This guide is designed to be your definitive resource, moving beyond simple salary numbers to explore the complex factors that shape an intensivist's earnings, career trajectory, and long-term professional satisfaction. We will dissect the nuances of compensation, from the impact of your geographic location and primary specialty to the financial benefits of leadership roles and in-demand skills. During a difficult time for my own family, I witnessed firsthand the calm, commanding presence of an intensivist coordinating a whirlwind of medical activity around a loved one. That experience cemented my understanding that their value isn't just measured in dollars, but in the moments of clarity, compassion, and hope they provide during life's most critical junctures.
Whether you are a medical student weighing your options, a resident deep in training, or a practicing physician considering a fellowship, this article will provide the authoritative, data-driven insights you need to understand the financial landscape of a career in critical care medicine.
### Table of Contents
- [What Does a Critical Care Doctor Do?](#what-does-a-critical-care-doctor-do)
- [Average Critical Care Doctor Salary: A Deep Dive](#average-critical-care-doctor-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
---
What Does a Critical Care Doctor Do?

A critical care doctor, or intensivist, is a physician who has completed a fellowship and achieved board certification in the subspecialty of critical care medicine. They are the primary physicians and leaders within the Intensive Care Unit (ICU), a specialized hospital department that provides comprehensive, around-the-clock care for patients with life-threatening conditions. Their patients are the sickest in the hospital, often suffering from multi-organ failure, severe trauma, complex post-surgical complications, or acute illnesses like septic shock or acute respiratory distress syndrome (ARDS).
The role of an intensivist is multifaceted, blending deep medical knowledge, procedural skill, and exceptional leadership. They are experts in managing the delicate interplay of the body's organ systems and are proficient in the use of sophisticated life-support technologies.
Core Responsibilities Include:
- Diagnosis and Management: Diagnosing and treating a wide spectrum of complex, acute, and often unstable medical conditions.
- Life Support Management: Overseeing the use of advanced technologies, including mechanical ventilators (breathing machines), dialysis machines for kidney failure, and vasoactive medications to support blood pressure.
- Procedural Expertise: Performing invasive procedures necessary for monitoring and treatment, such as placing central venous catheters (central lines), arterial lines, and endotracheal tubes for intubation.
- Team Leadership: Leading and coordinating a multidisciplinary team of healthcare professionals, which includes ICU nurses, respiratory therapists, pharmacists, physical therapists, and other physician specialists (e.g., cardiologists, nephrologists, infectious disease specialists).
- Communication and End-of-Life Care: Communicating complex medical information and prognoses to patients and their families in a clear and compassionate manner. A significant part of the role involves facilitating difficult conversations about goals of care, palliative options, and end-of-life decisions.
- Quality and Safety: Developing and implementing protocols to ensure patient safety, prevent hospital-acquired infections, and improve outcomes in the ICU.
### A Day in the Life of an Intensivist
To truly understand the role, consider a typical 12-hour shift:
- 7:00 AM - Sign-out: The day begins by receiving a detailed "sign-out" or handoff from the overnight intensivist. This is a comprehensive review of every patient in the ICU, covering overnight events, changes in condition, new admissions, and pending issues.
- 7:30 AM - Pre-Rounds Review: The intensivist reviews new lab results, imaging studies (X-rays, CT scans), and vital sign trends for all patients. They physically check the settings on ventilators and infusion pumps, preparing a preliminary plan for the day.
- 9:00 AM - Multidisciplinary Rounds: This is the heart of the day. The intensivist leads the entire ICU team (nurses, pharmacist, respiratory therapist, dietician, social worker) from bedside to bedside. For each patient, the team discusses the progress, reviews all organ systems, and collaborates to create a comprehensive care plan for the next 24 hours. The intensivist makes the final decisions on medication adjustments, ventilator changes, and plans for further testing.
- 12:00 PM - Procedures and Consults: The post-rounds period is dedicated to action. The intensivist may perform procedures like placing a central line in a new admission or a bronchoscopy to investigate a lung issue. They also spend time on the phone, consulting with surgeons, cardiologists, or other specialists about shared patients.
- 2:00 PM - Family Meetings: The afternoon is often when intensivists meet with families. These can be simple updates or profound, difficult conversations about a patient's poor prognosis and the transition to comfort-focused care.
- 4:00 PM - Managing New Admissions and "Codes": The ICU is a dynamic environment. A new, critically ill patient may arrive from the emergency department or operating room, requiring immediate assessment and stabilization. The intensivist must also respond instantly to any "Code Blue" (cardiac arrest) or other medical emergencies on the unit.
- 6:00 PM - Documentation and Evening Prep: The intensivist meticulously documents the day's events, decisions, and care plans in each patient's electronic health record. They review final lab results and ensure all plans are in motion before the night shift arrives.
- 7:00 PM - Sign-out: The cycle completes as the intensivist gives a thorough sign-out to the incoming nighttime physician, ensuring a safe and seamless transition of care.
This "typical" day is frequently interrupted by crises, requiring the intensivist to be adaptable, resilient, and capable of extreme focus under immense pressure.
---
Average Critical Care Doctor Salary: A Deep Dive
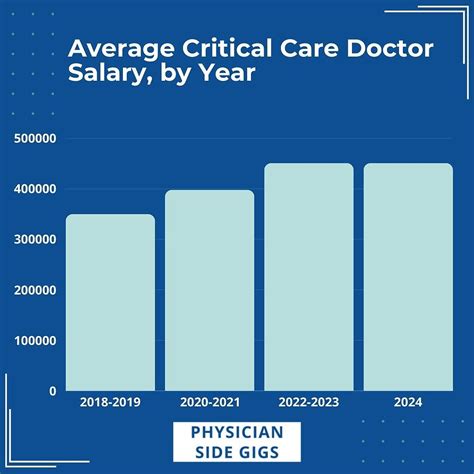
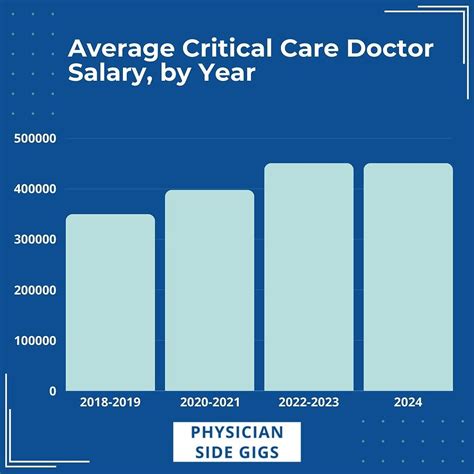
The compensation for critical care physicians reflects the extensive training, long hours, and high-stress nature of the specialty. It is consistently ranked among the higher-paying medical fields. While exact figures vary based on numerous factors we'll explore later, we can establish a strong baseline using data from the industry's most reputable sources.
According to the 2023 Medscape Physician Compensation Report, which surveys thousands of physicians across the United States, critical care is a top-earning specialty. The report found the average annual income for a critical care physician to be $406,000.
Similarly, the Doximity 2023 Physician Compensation Report, another widely respected industry benchmark, places the average annual compensation for Critical Care specialists at $403,969. It's important to note that these figures represent total compensation, which often includes a base salary plus bonuses and other incentives.
The typical salary range for a critical care doctor is broad, starting around $300,000 for those just finishing their fellowship and entering their first attending position, and climbing to $550,000 or more for experienced physicians in high-demand locations or leadership roles.
### Salary by Experience Level
Like all professions, compensation in critical care medicine grows significantly with experience. As physicians gain clinical expertise, efficiency, and potentially take on administrative or teaching responsibilities, their value to a hospital or practice group increases.
Here is a breakdown of expected salary brackets based on career stage, synthesized from data provided by sources like Salary.com, Payscale, and industry reports:
| Career Stage | Years of Experience | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level (Junior Attending) | 0-4 Years | $300,000 - $380,000 | Just completed fellowship. Focus is on building clinical confidence and efficiency. Lower end of the pay scale but often receives significant signing bonuses. |
| Mid-Career | 5-14 Years | $380,000 - $450,000 | Established clinical expert. Highly efficient and comfortable managing complex cases. May begin to take on mentorship or committee roles. |
| Senior/Experienced | 15+ Years | $450,000 - $550,000+ | A leader in the ICU. Often holds formal leadership positions (e.g., ICU Medical Director). May be involved in hospital-level administration, research, or fellowship program direction. |
*Note: These ranges are illustrative and can be influenced heavily by the factors discussed in the next section.*
### Beyond the Base Salary: Understanding Total Compensation
An intensivist's offer letter is rarely just a single salary figure. Total compensation is a package that includes various components, significantly boosting the overall financial picture. When evaluating a job offer, it's crucial to look at the entire package.
Common Components of a Critical Care Doctor's Compensation Package:
- Base Salary: The guaranteed annual income for clinical work.
- Productivity Bonuses: This is a major component of many contracts. Bonuses can be tied to a physician's productivity, often measured in Relative Value Units (RVUs). An RVU is a measure used by Medicare to determine the value of physician services. The more patients a doctor sees and the more complex their care, the more RVUs they generate, leading to higher bonus potential.
- Quality Bonuses: An increasing number of hospitals are tying a portion of compensation to quality metrics. This can include metrics like low rates of central line-associated bloodstream infections (CLABSIs), ventilator-associated pneumonia (VAP), or high patient/family satisfaction scores.
- Signing Bonus: To attract top talent in a competitive market, many hospitals offer a substantial one-time signing bonus, which can range from $20,000 to $50,000 or more. This is particularly common for physicians relocating or joining practices in less urban areas.
- Relocation Assistance: A stipend, often between $10,000 and $20,000, to cover the costs of moving.
- Call Pay: Some contracts include extra pay for being "on call" from home or for working additional nights or weekends beyond the contracted schedule.
- Retirement Plans: This is a critical long-term benefit. Employers typically offer a 401(k) or 403(b) plan with a matching contribution. A common match might be 50% of the physician's contribution up to 6% of their salary, effectively adding thousands of dollars of "free money" to their retirement savings each year.
- Continuing Medical Education (CME) Stipend: A yearly allowance (e.g., $3,000 - $7,500) to cover the cost of attending medical conferences, subscribing to journals, and fulfilling state licensing requirements for ongoing education.
- Health and Disability Insurance: Comprehensive health, dental, and vision insurance for the physician and their family. Crucially, this also includes robust long-term disability and life insurance policies, which are essential for a high-income earner.
- Malpractice Insurance: The employer almost always covers the full cost of medical malpractice insurance, which can be a significant expense (tens of thousands of dollars per year). Understanding the type of policy (claims-made vs. occurrence) and whether "tail coverage" is included is vital.
---
Key Factors That Influence Salary

The national average salary of over $400,000 is a useful starting point, but the reality is that an individual critical care doctor's earnings are determined by a complex interplay of variables. Understanding these factors is essential for any aspiring or practicing intensivist looking to maximize their earning potential and make informed career decisions. This section provides a detailed examination of the primary drivers of salary variation.
###
Education and Board Certification: The Foundation of Value
In medicine, the educational and certification pathway is rigidly defined and directly correlates with earning power. For a critical care doctor, this is non-negotiable.
- Medical Degree (MD or DO): The foundational step is graduating from an accredited medical school, earning either a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree. For compensation purposes in the U.S., there is no significant, consistent difference in salary between physicians holding an MD versus a DO.
- Residency and Board Certification in a Primary Specialty: After medical school, a physician must complete a residency program, which typically lasts from three to seven years. A critical care fellowship can be entered from several primary specialties. The most common pathways are:
- Internal Medicine (3 years)
- Anesthesiology (4 years)
- Emergency Medicine (3-4 years)
- General Surgery (5 years)
- Critical Care Fellowship: This is the key step that defines the intensivist. It is a one-to-two-year period of subspecialty training focused exclusively on the management of critically ill patients.
- Double Board Certification: The ultimate mark of qualification and a prerequisite for nearly all high-paying jobs is achieving board certification from the relevant medical boards. An intensivist will be board-certified in their primary specialty (e.g., by the American Board of Internal Medicine) *and* in the subspecialty of Critical Care Medicine. Lacking these certifications would severely limit job opportunities and drastically reduce earning potential. An uncertified physician would be unable to command the salaries discussed in this article.
###
Years of Experience and Career Progression: The Upward Trajectory
As detailed in the previous section, experience is one of the most direct and predictable drivers of salary growth. This progression isn't just about longevity; it's about the accumulation of value.
- 0-4 Years (The Learning Curve): Early-career intensivists are paid well but are on the lower end of the specialty's spectrum. Their focus is on translating fellowship knowledge into real-world practice, becoming faster and more confident with procedures, and mastering the leadership of the ICU team. Hospitals invest in these physicians, knowing their value will increase.
- 5-14 Years (The Prime Earning Years): By this stage, the intensivist is a seasoned, efficient, and highly competent clinician. They can manage multiple complex patients simultaneously and serve as a resource for junior colleagues. Their productivity (in RVU terms) is often at its peak, directly translating to higher bonus potential. Many in this group begin to take on extra-curricular responsibilities that add to their compensation.
- 15+ Years (Leadership and Legacy): Senior physicians often transition some of their focus from pure clinical volume to leadership and administrative roles. Taking on the position of ICU Medical Director, for example, typically comes with a significant administrative stipend (e.g., an additional $50,000 - $100,000+ per year) on top of their clinical salary. Other roles include leading a fellowship program, heading a hospital ethics committee, or moving into higher-level hospital administration like a Chief Medical Officer (CMO) role, which carries a completely different and often much higher pay scale.
###
Geographic Location: The Pay-Per-Place Phenomenon
Where you practice medicine has a colossal impact on your salary. This is driven by supply and demand, cost of living, and the concentration of healthcare systems. Interestingly, physician salaries often have an inverse relationship with the perceived desirability of a location. Major, popular coastal cities have a high supply of physicians wanting to live there, which can suppress salaries, while less populated or rural areas must offer higher compensation to attract talent.
According to Doximity's 2023 report, compensation is generally higher in the Southeast and Midwest and lower in the Northeast.
Examples of High-Paying vs. Lower-Paying Regions (Illustrative):
| High-Paying States/Areas | Typical Reported Salary Range | Why It's High |
| :--- | :--- | :--- |
| Midwest States (e.g., Wisconsin, Indiana, Iowa) | $430,000 - $500,000+ | High demand, particularly in non-metropolitan areas. Lower supply of specialists. Lower cost of living means take-home pay is even greater. |
| Southeast States (e.g., Alabama, Georgia, Florida) | $420,000 - $490,000 | Growing populations and a high burden of chronic disease create strong demand for intensivists. |
| Rural/Underserved Areas | $450,000 - $550,000+ | Extreme demand and very low supply. Hospitals must offer top-tier compensation, loan forgiveness, and large signing bonuses to recruit physicians. |
| Lower-Paying States/Areas | Typical Reported Salary Range | Why It's Lower |
| :--- | :--- | :--- |
| Northeast (e.g., Massachusetts, Maryland, New York) | $350,000 - $410,000 | High concentration of prestigious academic medical centers, which traditionally pay less. A very high supply of physicians want to live and train in these areas. |
| Major West Coast Cities (e.g., SF, LA) | $360,000 - $420,000 | Similar to the Northeast, high desirability and an oversupply of specialists can drive down compensation relative to the extremely high cost of living. |
*Source: Synthesized from Doximity, Medscape, and various physician recruiting firm data.*
###
Practice Setting and Employer Type: Who Signs the Paycheck
The type of institution an intensivist works for is another major determinant of their salary and overall compensation structure.
- Academic Medical Centers: These are large hospitals affiliated with a medical school.
- Salary: Generally on the lower end of the spectrum. A starting salary might be closer to $300,000-$350,000.
- Pros: Excellent benefits (pension plans, generous retirement matches), prestige, and opportunities for teaching, research, and educating residents and fellows. The work can be intellectually stimulating, focusing on rare and complex cases.
- Cons: Lower base pay and often less potential for productivity-based bonuses. Career advancement can be tied to academic output (publications) rather than just clinical excellence.
- Private Practice Groups: These are physician-owned groups that contract their services to one or more hospitals.
- Salary: High income potential, often exceeding $500,000 for partners.
- Pros: After a few years as an employee, physicians may have a "partnership track" opportunity. As a partner, they share in the profits of the group, leading to the highest earning potential. More autonomy in decision-making.
- Cons: Requires business acumen. Partners are small business owners, responsible for overhead, billing, and administration. Benefits packages might be less robust than those at large hospitals. Income can be more variable.
- Hospital-Employed (Large Health Systems): The most common model today. Physicians are direct employees of a large hospital or a multi-state health system (e.g., HCA, Kaiser Permanente, Mayo Clinic Health System).
- Salary: Strong and competitive, often falling in the middle-to-high range ($380,000 - $480,000). Compensation is typically a base salary plus a heavily weighted productivity (RVU) bonus.
- Pros: Stability, predictable income, strong benefits, and relief from the administrative burdens of running a practice. Large systems offer significant resources and a built-in referral network.
- Cons: Less autonomy. Physicians are subject to the policies and directives of a large corporate entity.
- Locum Tenens: This means "to hold the place of." Locum tenens physicians work as temporary, independent contractors to fill short-term staffing gaps.
- Salary: The highest hourly/daily rate of pay. Rates can be $2,500 - $4,000+ per 12-hour shift.
- Pros: Maximum flexibility and extremely high pay. A way to "test drive" different locations and practice settings. Malpractice insurance, housing, and travel are typically covered by the staffing agency.
- Cons: No benefits (retirement, health insurance), no paid time off. Instability and constant travel. It can be challenging to integrate into a new team for a short period.
###
Primary Specialty Pathway and Additional Fellowships
The residency path taken *before* the critical care fellowship can influence the scope of practice and, in some cases, compensation.
- Pulmonary/Critical Care: This is the most common pathway from Internal Medicine. Physicians complete a combined fellowship (usually 3 years) and are board-certified in both Pulmonary Medicine and Critical Care. This allows them to see patients in the ICU, but also run an outpatient pulmonary clinic and perform procedures like bronchoscopy. This dual skill set can create more revenue streams for a practice, sometimes leading to higher compensation packages.
- Surgical Critical Care: Surgeons who complete a surgical critical care fellowship are experts in managing critically ill surgical and trauma patients. They often work in dedicated Surgical or Trauma ICUs (SICU/TICU). Their compensation may be benchmarked against other surgeons, which are often among the highest-paid physicians.
- Anesthesiology Critical Care: Anesthesiologists are experts in physiology, pharmacology, and airway management, making for a natural transition to the ICU. They are highly sought after for all types of ICUs. Their compensation tends to align closely with the national average for intensivists.
- Neurocritical Care: A further sub-specialization involving a dedicated fellowship in managing patients with critical neurological illnesses (e.g., severe stroke, brain hemorrhage, status epilepticus). This highly specialized expertise can command a premium salary, particularly at comprehensive stroke centers.
###
In-Demand Skills and Additional Responsibilities
Finally, physicians who cultivate skills and take on roles that add value beyond standard clinical duties can significantly increase their income.
- Advanced Procedural Skills: Expertise in highly specialized technologies like ECMO (Extracorporeal Membrane Oxygenation) is in high demand. Physicians who can manage ECMO patients are a major asset to a hospital's cardiac or transplant programs and can command higher salaries. Advanced proficiency in critical care ultrasound is another highly valued skill.
- Administrative Leadership: As mentioned, becoming the ICU Medical Director is the most common path to a significant salary boost. This role involves administrative oversight, quality improvement initiatives, staff scheduling, and budget management.
- Informatics/IT Roles: A physician who is also an expert in the Electronic Health Record (EHR) system can become a "physician champion" or take on a role in clinical informatics, receiving a stipend for helping to optimize the system for clinical use.
- Research and Publications: In academic settings, a strong research portfolio, particularly one that secures external grant funding (e.g., from the NIH), can lead to a protected portion of time for research and a higher academic rank and salary.
---
Job Outlook and Career Growth

For those investing more than a decade in education and training, the long-term viability of their chosen profession is a paramount concern. Fortunately, the job outlook for critical care physicians is exceptionally strong and is projected to remain so for the foreseeable future. The demand for their unique expertise is being driven by several powerful, long-term demographic and medical trends.
The U.S. Bureau of Labor Statistics (BLS) projects that overall employment for Physicians and Surgeons will grow by 3% from 2022 to 2032, which is about as fast as the average for all occupations. However, this aggregate figure masks the much higher demand within specific specialties. The demand for intensivists is expected to significantly outpace this average due to a confluence of factors creating a "perfect storm" of need.
A landmark 2021 study published by the U.S. Department of Health and Human Services (HHS) projected a substantial shortage of critical care physicians. The report highlighted that demand for intensivists would grow by as much as 35% over the coming decade, while the supply of these specialists would grow at a much slower rate, creating a significant workforce gap.
Key Drivers of High Demand for Intensivists:
1. The Aging Population: The "baby boomer" generation is aging into a period of life where complex and critical illnesses become more common. Older patients are more likely to suffer from conditions like sepsis, heart failure, and respiratory failure that necessitate ICU-level care. This demographic shift is the single largest driver of demand.
2. Advances in Medical Technology: Modern medicine is now able to sustain patients with illnesses that were once rapidly fatal. Advances in surgery, oncology, and organ transplantation mean that more patients survive their initial insult but require prolonged, complex support in an ICU. This creates a larger and sicker population of potential ICU patients.
3. The Rise of "ICU without Walls": Intensivists are increasingly being asked to consult on critically ill patients outside the traditional ICU, leading rapid response teams and co-managing sick patients on general medical floors. This expands their scope and increases the number of intensivists a hospital needs