Introduction

Imagine a career that sits at the absolute apex of medical science, human skill, and profound responsibility. A field where the patients are the most vulnerable among us—children—and the stakes are, quite literally, life and the quality of life itself. This is the world of the pediatric neurosurgeon. It is a path defined by a decade and a half of relentless training, unwavering dedication, and the unique ability to navigate the most complex organ in the human body: the developing brain.
For those with the intellectual horsepower, emotional fortitude, and technical mastery to pursue this calling, the rewards are commensurate with the challenges. The financial compensation is, without question, among the highest in any profession. A typical salary of a pediatric neurosurgeon often starts well above $500,000 and can easily soar past the $1,000,000 mark for experienced practitioners in high-demand settings. Yet, to focus solely on the numbers is to miss the true essence of the role.
I once had the privilege of speaking with a senior pediatric neurosurgeon about a particularly complex case involving a newborn with a rare brain malformation. He didn't speak of the technical difficulty or the long hours. Instead, he described the moment, weeks after the surgery, when he watched the child’s parents hold their baby, now thriving, with tears of pure relief. "That," he said, "is the real paycheck. The rest just keeps the lights on." That profound sense of purpose is the unquantifiable bonus that draws a rare few to this extraordinary field.
This guide is designed to be your definitive resource, whether you are a high school student dreaming of a medical career, a medical student considering a specialization, or a healthcare professional seeking to understand this unique niche. We will dissect every facet of this career, from the day-to-day responsibilities to the intricate factors that shape a pediatric neurosurgeon's salary and long-term career trajectory.
### Table of Contents
- [What Does a Pediatric Neurosurgeon Do?](#what-does-a-pediatric-neurosurgeon-do)
- [Average Pediatric Neurosurgeon Salary: A Deep Dive](#average-pediatric-neurosurgeon-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
---
What Does a Pediatric Neurosurgeon Do?

A pediatric neurosurgeon is a highly specialized medical doctor who diagnoses, treats, and surgically manages disorders of the central and peripheral nervous systems in children, from the fetal stage through adolescence. Their domain encompasses the brain, spinal cord, nerves, and skull. Unlike general neurosurgeons who may occasionally treat children, pediatric neurosurgeons have undergone specific fellowship training focused exclusively on the unique anatomical, physiological, and disease-related aspects of the developing nervous system.
The scope of their work is breathtakingly broad. They are not just "brain surgeons" for kids; they are comprehensive specialists who manage a wide array of conditions, many of which are congenital (present at birth) or developmental.
Core Responsibilities and Conditions Treated:
- Congenital Malformations: Treating conditions like spina bifida (myelomeningocele), hydrocephalus (the buildup of fluid in the brain, often requiring the placement of a shunt), encephalocele, and tethered spinal cords.
- Neuro-Oncology: Diagnosing and surgically removing benign and malignant brain and spinal cord tumors, such as medulloblastomas, astrocytomas, and ependymomas. This often involves collaborating closely with pediatric oncologists and radiation oncologists.
- Epilepsy Surgery: For children with intractable seizures that don't respond to medication, these surgeons perform complex procedures like temporal lobectomies, hemispherectomies, or corpus callosotomies to control or eliminate seizure activity.
- Craniofacial Abnormalities: Working as part of a multidisciplinary team to surgically correct conditions like craniosynostosis (premature fusion of skull sutures) that can restrict brain growth and cause cosmetic deformities.
- Vascular Abnormalities: Managing complex and dangerous conditions such as arteriovenous malformations (AVMs), cavernomas, and Moyamoya disease, which can cause strokes or brain hemorrhages in children.
- Trauma: Providing emergency surgical care for traumatic brain injuries (TBIs) and spinal cord injuries resulting from accidents, falls, or abuse.
- Spasticity Management: Performing procedures like selective dorsal rhizotomy (SDR) or implanting baclofen pumps to help manage severe muscle spasticity associated with conditions like cerebral palsy.
### A "Day in the Life" Example
To make this tangible, let's walk through a hypothetical day for Dr. Anya Sharma, a pediatric neurosurgeon at a major children's hospital.
- 5:30 AM: Wake up. Review patient charts and imaging scans for the day's cases from home.
- 6:30 AM: Arrive at the hospital. Begin morning rounds on post-operative patients and those in the Pediatric Intensive Care Unit (PICU). This involves checking neurological status, reviewing vitals, adjusting medication, and speaking with the night-shift residents and nurses.
- 7:30 AM: Pre-operative conference. Dr. Sharma meets with her team—including anesthesiologists, surgical nurses, and residents—to review the plan for the day's main case: the resection of a 4cm ependymoma from the brainstem of a 6-year-old boy. They discuss potential complications and contingency plans.
- 8:00 AM: Meet with the 6-year-old's family. She calmly and empathetically explains the procedure one last time, answers their questions, and provides reassurance before their child is taken to the operating room.
- 8:30 AM - 4:30 PM: The Surgery. This is eight hours of intense, microscopic work. Using a high-powered microscope and advanced neuro-navigation technology, Dr. Sharma and her team meticulously work to remove the tumor while preserving critical brain function. Every millimeter matters.
- 4:30 PM: Scrub out. Dr. Sharma immediately goes to speak with the family to inform them the surgery went as planned.
- 5:00 PM: Post-operative work. She dictates the operative note, writes orders for the patient's care in the PICU, and checks the post-op MRI scan to confirm the extent of resection.
- 6:00 PM: Afternoon Clinic. She sees a handful of patients for follow-up appointments and new consultations. This includes a 3-month-old with newly diagnosed hydrocephalus and a teenager recovering from a spinal cord injury.
- 7:30 PM: Evening rounds. A final check on her post-op patient and other critical patients in the hospital.
- 8:30 PM: Head home, but the work isn't over. She may spend another hour reading recent medical journals or preparing for a presentation. As she is on call tonight, her phone is never far away, ready for a potential emergency admission from the ER.
This demanding schedule underscores that the role is far more than a job; it is a life commitment.
---
Average Pediatric Neurosurgeon Salary: A Deep Dive
The path to becoming a pediatric neurosurgeon is one of the longest and most arduous in all of medicine, typically requiring 15-16 years of post-high school education and training. The compensation structure reflects this immense investment of time, intellect, and personal sacrifice. Salaries for pediatric neurosurgeons are consistently ranked among the highest for any profession.
It's important to note that the U.S. Bureau of Labor Statistics (BLS) groups all "Physicians and Surgeons" together, providing a median salary of $239,200 per year as of May 2023. While useful for a general overview, this figure is not representative of a highly specialized surgical field like pediatric neurosurgery. For accurate data, we must turn to specialized industry reports and salary aggregators that survey physicians directly.
According to Salary.com, as of late 2023, the median annual salary for a pediatric neurosurgeon in the United States is an impressive $823,700. The salary range is exceptionally wide, reflecting the significant impact of experience, location, and practice type:
- Bottom 10%: $455,800
- 25th Percentile: $631,000
- 50th Percentile (Median): $823,700
- 75th Percentile: $1,036,500
- Top 10%: $1,213,200
Data from other sources corroborates these high figures. The 2023 Doximity Physician Compensation Report, a highly respected source in the medical community, places Neurosurgery as the #1 highest-paid specialty overall, with an average compensation of $788,313. While this figure combines adult and pediatric specialists, it confirms the top-tier earning potential of the field.
### Salary by Experience Level
Salary growth in this field is steep, especially in the first decade of practice as a surgeon builds their reputation, efficiency, and ability to handle more complex cases.
| Experience Level | Typical Years Post-Fellowship | Typical Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level / Early Career | 0-3 Years | $450,000 - $650,000 | Often in an academic setting with a guaranteed salary. Focus is on building clinical volume and establishing a reputation. May have a higher call burden. |
| Mid-Career | 4-10 Years | $650,000 - $950,000 | Has established a strong reputation. More efficient in the OR. May be taking on more complex, higher-value cases. Compensation is often heavily tied to productivity (wRVUs). |
| Senior / Late Career | 11-20+ Years | $900,000 - $1,200,000+ | At the peak of their career. May hold leadership positions (e.g., Division Chief, Department Chair). Highly sought after for their expertise. Compensation can exceed these figures in high-volume private practice settings. |
*Source: Aggregated data from Salary.com, Doximity reports, and medical recruiting firm analyses like Merritt Hawkins.*
### Deconstructing the Compensation Package
The final take-home pay is more complex than just a base salary. A pediatric neurosurgeon's total compensation package is a multi-layered structure designed to attract and retain elite talent.
- Base Salary: This is the guaranteed portion of income, often higher in the first 1-2 years of practice before a physician transitions to a productivity-based model.
- Productivity Bonuses (wRVUs): This is the most significant variable component. The wRVU (work Relative Value Unit) is a metric used by Medicare and commercial insurers to value the work involved in a medical service. Each procedure (e.g., a shunt placement, a tumor resection) is assigned a specific wRVU value. Surgeons are often paid a certain dollar amount per wRVU generated above a set threshold. This model directly rewards high-volume, efficient surgeons.
- Sign-On Bonus: To attract top fellows straight out of training, hospitals often offer substantial sign-on bonuses, which can range from $25,000 to over $100,000.
- Call Pay: Neurosurgeons are frequently on call for emergencies. Many hospitals provide a daily stipend (per diem) for being on call, plus additional payment if they are called in to operate.
- Performance & Quality Bonuses: Increasingly, a portion of compensation is tied to quality metrics, such as patient outcomes, complication rates, and patient satisfaction scores.
- Academic & Administrative Stipends: Surgeons in academic settings receive stipends for leadership roles like being the Fellowship Program Director or Division Chief.
- Relocation Assistance: A package to cover moving expenses, often worth $10,000-$20,000.
- Retirement Benefits: Robust packages including 401(k) or 403(b) plans with significant employer matching contributions.
- Insurance: This is a critical, high-value benefit.
- Malpractice Insurance: Fully paid "claims-made" or "occurrence" policies with liability limits in the millions. "Tail coverage," which protects a physician after they leave a practice, is a crucial and expensive negotiation point.
- Health, Dental, and Vision Insurance: Comprehensive family plans.
- Disability and Life Insurance: High-limit policies to protect the surgeon's substantial income in case of career-ending injury or illness.
This comprehensive package means the total value of a pediatric neurosurgeon's employment can be tens of thousands of dollars more than the salary figure alone suggests.
---
Key Factors That Influence Salary

The vast salary ranges presented above are not arbitrary. They are the result of a complex interplay of factors that can dramatically influence a surgeon's earning potential. Understanding these variables is critical for anyone planning a career in this field.
###
1. Years of Experience and Reputation
This is arguably the most powerful driver of salary growth. In surgery, experience directly correlates with skill, efficiency, and reputation.
- Early Career (Years 1-3): Surgeons fresh out of fellowship are highly skilled but are still building their speed, refining their techniques, and establishing referral patterns. Their initial contracts are often heavily guaranteed to provide stability. An initial salary might be in the $500,000 to $650,000 range.
- Mid-Career (Years 4-10): By this stage, the surgeon has a proven track record. They can handle a higher volume of cases and take on more complex procedures that carry higher wRVU values. Their compensation model shifts heavily towards productivity. Earnings often climb to the $700,000 to $950,000 range. Reputation begins to play a major role, as primary care physicians and pediatric neurologists refer their most challenging cases to them.
- Senior Career (11+ Years): These are the masters of the craft. A senior pediatric neurosurgeon's value is immense. They are not only highly productive clinicians but also mentors, leaders, and institutional assets. Many take on administrative roles like Chief of Pediatric Neurosurgery or Chair of the Department of Neurological Surgery, which come with significant administrative stipends on top of their clinical income. It is at this stage that salaries can comfortably exceed $1,000,000 per year. Their reputation may be national or even international, attracting patients from far and wide.
###
2. Geographic Location
Where a surgeon practices has a profound impact on their salary, driven by supply and demand, cost of living, and the local healthcare market.
- High-Paying Regions: Often, the highest raw salaries are not in the most glamorous coastal cities but in the Midwest, Southeast, and less-populated states. This is a classic supply-and-demand issue. There are fewer specialists to cover large geographic areas, forcing hospitals in these regions to offer highly competitive compensation packages to attract talent. States like North Dakota, Wisconsin, Alabama, and Florida often appear on lists of top-paying states for physicians. A surgeon in one of these regions might command a salary 15-25% higher than the national median.
- Moderate-to-Low Paying Regions: Conversely, major metropolitan areas with a high density of academic medical centers (e.g., Boston, New York City, San Francisco) may have slightly lower median salaries. While the cost of living is extremely high, the desirability of these locations and the prestige of the institutions create a large supply of top-tier candidates. The compensation trade-off is often for a more academic environment, research opportunities, and quality of life.
- The Urban vs. Rural Dynamic: A pediatric neurosurgeon at a standalone children's hospital in a mid-sized city in the Midwest could easily earn more than a counterpart at a world-famous university hospital in the Northeast. The former is likely paid purely on productivity in a high-volume setting, while the latter may have protected time for research and teaching, which lowers their clinical wRVU generation.
Example Salary Variation by State (Illustrative):
| State | Typical Median Salary | Market Dynamics |
| :--- | :--- | :--- |
| Wisconsin | ~$950,000+ | High demand, fewer specialists, favorable malpractice climate. |
| Florida | ~$920,000+ | High patient volume, competitive private and hospital markets. |
| Texas | ~$880,000+ | Large population, major medical centers, favorable business environment. |
| California | ~$850,000+ | High cost of living, but also high reimbursement rates. Very competitive. |
| New York | ~$800,000+ | Dense with academic centers, prestige factor can slightly suppress salaries relative to COL. |
*Note: These are estimates based on aggregated market data and can fluctuate significantly.*
###
3. Type of Practice
The organizational structure in which a surgeon works is a fundamental determinant of their compensation model and ultimate earning potential.
- Academic Medical Centers: These are university-affiliated hospitals.
- Salary Model: Often a lower base salary plus more modest productivity bonuses compared to private settings. The overall compensation tends to fall at the lower end of the national range.
- Pros: Access to cutting-edge research, teaching responsibilities (training residents and fellows), institutional prestige, and often better benefits and work-life balance (e.g., less call burden). The "currency" here is partially financial and partially academic.
- Earning Potential: Generally $550,000 - $850,000.
- Private, Physician-Owned Practice (Solo or Group):
- Salary Model: This offers the highest earning *potential*. After an initial guaranteed period, compensation is directly tied to the practice's revenue and collections. The surgeon is a business owner.
- Pros: Autonomy, direct financial reward for hard work ("eat what you kill").
- Cons: Enormous administrative burden (billing, staffing, marketing, managing overhead), higher personal financial risk, and responsibility for covering malpractice insurance and retirement benefits.
- Earning Potential: Highly variable, but successful private practice surgeons can earn $1,000,000 to $2,000,000+ per year.
- Hospital-Employed (Large Children's Hospital or Health System):
- Salary Model: This is the most common model today. It's a hybrid, offering the security of employment with a compensation plan heavily based on productivity (wRVUs).
- Pros: The hospital handles all administrative overhead, allowing the surgeon to focus solely on clinical medicine. They get the benefits of being an employee (paid malpractice, retirement plans) while still being rewarded for high volume.
- Cons: Less autonomy than private practice.
- Earning Potential: This model offers a very high and stable income, typically in the $700,000 to $1,200,000 range for experienced surgeons.
###
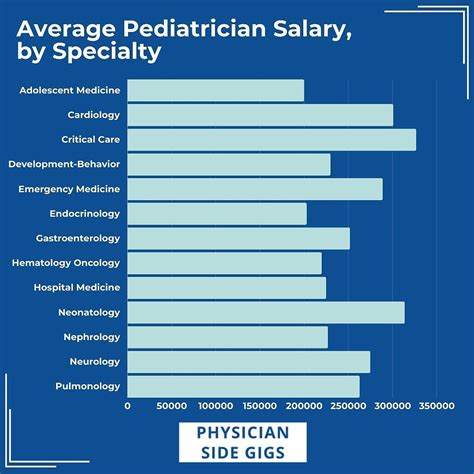
4. Sub-Specialization
While pediatric neurosurgery is already a sub-specialty, further fellowship training in a high-demand niche can increase a surgeon's value and earning potential.
- Pediatric Epilepsy Surgery: This requires highly specialized training and technology (e.g., stereo-EEG, laser ablation). As one of a few regional experts, a surgeon can command higher compensation.
- Fetal Neurosurgery: An emerging and incredibly complex field, operating on babies *in utero* to correct conditions like spina bifida. Only a handful of centers in the world offer this, making these surgeons exceptionally valuable.
- Pediatric Neuro-Oncology: Surgeons who specialize in the most complex brain tumors, particularly those integrated with advanced research and clinical trials, are critical assets to top-tier children's hospitals.
- Craniofacial Surgery: Expertise in complex skull reconstruction is a highly marketable skill that can lead to a lucrative practice.
###
5. In-Demand Skills and Academic Profile
Beyond the scalpel, other skills contribute to a surgeon's value.
- Minimally Invasive Techniques: Proficiency in endoscopic and endovascular neurosurgery can lead to better patient outcomes, shorter hospital stays, and are attractive skills for hospitals to market.
- Research and Grant Funding: A surgeon who is also a successful researcher with a portfolio of publications and, most importantly, NIH (National Institutes of Health) grant funding, is a huge asset to an academic institution. This can lead to protected research time and a higher academic rank (e.g., full Professor), which translates to higher salary and institutional influence.
- Leadership and Administrative Acumen: As mentioned, taking on roles like Division Chief, Department Chair, or Surgeon-in-Chief of a children's hospital involves a significant step up in responsibility and compensation. These roles require skills in budgeting, strategy, and personnel management.
---
Job Outlook and Career Growth

The career outlook for pediatric neurosurgeons is exceptionally stable and positive. While the overall number of positions is small due to the hyper-specialized nature of the field, the demand for their services is consistent and driven by factors that are insulated from economic fluctuations.
### Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) projects that employment for all physicians and surgeons will grow by 3% from 2022 to 2032, which is about the average for all occupations. However, this general statistic doesn't capture the full picture for pediatric neurosurgery.
The demand is not about explosive growth but about sustained need. There are only a few hundred board-certified pediatric neurosurgeons practicing in the entire United States. The pipeline for creating new ones is long and narrow, with only about 20-25 fellowship positions available each year. This limited supply, coupled with a steady demand driven by birth rates and the incidence of pediatric neurological conditions, ensures that qualified specialists will always be highly sought after.
Factors ensuring a stable demand include:
- Population Growth: A growing population means more children, and thus a consistent number of patients requiring care.
- Medical Advances: Advances in neonatology and pediatric care mean that more children with complex congenital conditions are surviving, and these children often require lifelong neurosurgical management.
- Centralization of Care: Pediatric care is increasingly centralized in specialized children's hospitals. These institutions are constantly competing to have the best specialists on staff, creating a competitive hiring market.
### Emerging Trends and Future Challenges
The field is not static. A pediatric neurosurgeon's career will be shaped by several evolving trends and persistent challenges.
Emerging Trends:
1. Technological Integration: The operating room of the future will be even more technologically advanced. Robotics, augmented reality for surgical navigation, AI for interpreting imaging and predicting outcomes, and advanced intraoperative monitoring will become standard. Staying proficient with these technologies will be essential.
2. Genomics and Personalized Medicine: The treatment of brain tumors and other conditions will become increasingly personalized based on the genetic makeup of the patient and their disease. Neurosurgeons will need to be well-versed in molecular biology and work closely with geneticists.
3. Rise of Fetal Surgery: Operating on a fetus to correct defects before birth is a revolutionary frontier that will continue to expand, requiring a unique and highly collaborative skillset.
4. Minimally Invasive Approaches: The push towards less invasive procedures will continue, with more conditions being treated endoscopically (through the nose or small incisions) or endovascularly (through blood vessels), reducing recovery time and risk for patients.
Future Challenges:
1. Physician Burnout: The immense pressure, long hours, high stakes, and emotional toll of
