Table of Contents

- [What Does a Surgical Oncologist Do?](#what-does-a-surgical-oncologist-do)
- [Average Surgical Oncologist Salary: A Deep Dive](#average-surgical-oncologist-salary-a-deep-dive)
- [Key Factors That Influence a Surgical Oncologist's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Surgical Oncologists](#job-outlook-and-career-growth)
- [How to Become a Surgical Oncologist](#how-to-become-a-surgical-oncologist)
- [Conclusion: Is a Career in Surgical Oncology Right for You?](#conclusion)
---
To stand at the intersection of hope and despair, armed with a scalpel and a profound understanding of human biology, is the unique position of the surgical oncologist. It is a career not for the faint of heart, but for those driven by an unyielding desire to offer patients their best chance at a future. The path is extraordinarily long and demanding, but the rewards—both intangible and financial—are substantial. While the true calling lies in healing, understanding the financial landscape is a critical component of career planning. A surg onc salary reflects not just the years of grueling training, but the immense responsibility and high-stakes nature of the work. The average compensation for this specialty is among the highest in medicine, often ranging from $450,000 to over $750,000 annually, with top earners in private practice exceeding seven figures.
I once had the privilege of speaking with a senior surgical oncologist who described her work not as 'cutting out cancer,' but as 'restoring futures.' That powerful shift in perspective—viewing each procedure as a chance to return a mother to her children or a partner to their spouse—crystallized the profound human impact of this profession. This guide is for those who feel that same pull, providing a transparent, data-driven look into the career, from the operating room to the paycheck. We will dissect the salary data, explore the factors that shape your earning potential, and map out the rigorous journey to becoming a leader in the fight against cancer.
---
What Does a Surgical Oncologist Do?

A surgical oncologist is a highly specialized surgeon who focuses on the surgical management of cancer. They are not simply technicians who remove tumors; they are integral members of a multidisciplinary cancer care team, working alongside medical oncologists, radiation oncologists, pathologists, radiologists, and other specialists. Their expertise lies in understanding the complex biology of cancer and how it interacts with the human body, allowing them to perform intricate procedures that are often the most critical step in a patient's treatment plan.
The role of a surgical oncologist is comprehensive, spanning the entire patient journey:
- Diagnosis and Staging: While a diagnosis may be suspected by another physician, the surgical oncologist often performs the definitive biopsy to confirm the presence of cancer and determine its type. They then use this information, along with imaging studies, to "stage" the cancer, which means determining its size, location, and whether it has spread. This staging is crucial for developing an effective treatment strategy.
- Treatment Planning: The surgical oncologist is a key architect of the patient's overall treatment plan. They collaborate with the oncology team to decide if surgery is the best primary option, or if it should be used in conjunction with other treatments like chemotherapy or radiation (neoadjuvant therapy before surgery, or adjuvant therapy after).
- Surgical Intervention: This is the core of their work. They perform complex operations to remove malignant tumors and, in many cases, nearby lymph nodes or affected tissue to ensure all cancerous cells are eradicated (achieving "clear margins"). These procedures can range from minimally invasive laparoscopic or robotic surgeries to highly complex, open operations lasting many hours.
- Palliative Care: For patients with advanced, incurable cancer, a surgical oncologist may perform palliative surgeries. These procedures are not intended to cure the cancer but to relieve symptoms, such as pain or obstruction caused by a tumor, thereby improving the patient's quality of life.
- Post-Operative Care and Surveillance: After surgery, the surgical oncologist manages the patient's immediate recovery. They also play a vital role in long-term follow-up and surveillance, monitoring the patient for any signs of recurrence through regular check-ups and imaging.
### A Day in the Life of a Surgical Oncologist
To make this role more tangible, consider a typical day, which is often a demanding blend of clinical and surgical responsibilities.
6:00 AM - 7:00 AM: Hospital Rounds
The day begins early at the hospital. The surgeon and their team (residents, fellows, physician assistants) visit patients who underwent surgery the previous day. They check vital signs, review lab results, inspect surgical wounds, and assess pain levels. They also see patients who are being prepared for surgery later in the day, answering last-minute questions and providing reassurance.
7:30 AM - 3:00 PM: Operating Room (OR)
This is the heart of the day. The schedule might include two or three major cases. For example:
- Case 1 (7:30 AM - 11:00 AM): A robotic-assisted low anterior resection for rectal cancer. This minimally invasive procedure requires intense focus and technical precision.
- Case 2 (11:30 AM - 2:30 PM): A complex cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) for peritoneal cancer. This is a long, arduous procedure involving the removal of all visible tumors from the abdominal cavity, followed by a "chemo bath."
Between cases, the surgeon quickly updates the waiting family, dictates operative notes, and consults with the pathologist on intraoperative findings (e.g., frozen sections to check surgical margins).
3:00 PM - 6:00 PM: Afternoon Clinic
After changing out of scrubs, the surgeon heads to their outpatient clinic. This block of time is dedicated to seeing new patient consultations, post-operative follow-ups, and patients with ongoing surveillance.
- New Patient: A 55-year-old woman with a new diagnosis of pancreatic cancer. The surgeon spends an hour reviewing her scans, explaining the diagnosis and staging, and discussing the risks and benefits of a potential Whipple procedure. This conversation requires empathy, clarity, and the ability to manage patient and family anxiety.
- Post-Op: A patient who is four weeks out from a melanoma excision and sentinel lymph node biopsy. The surgeon examines the incision sites and delivers the good news that the final pathology report shows clear margins and negative nodes.
- Follow-Up: A patient who is three years post-treatment for colon cancer. The surgeon reviews recent surveillance scans and bloodwork, confirming no evidence of recurrence.
6:00 PM - 7:30 PM: Administrative Work and Team Coordination
The day isn't over yet. The surgeon must sign off on patient charts, respond to urgent emails, review new referrals, and participate in a virtual multidisciplinary tumor board meeting to discuss complex cases with other oncology specialists.
7:30 PM onwards:
The surgeon heads home, but the work is never truly done. They may be on call for the hospital, meaning they could be paged at any hour to handle a post-operative emergency. This demanding schedule underscores why the compensation is so high; it's a reflection of a life dedicated to the profession.
---
Average Surgical Oncologist Salary: A Deep Dive
The compensation for a surgical oncologist is among the highest across all medical specialties, a direct result of the extensive training required, the technical complexity of the procedures performed, and the high-stakes nature of the work. Salary figures can vary significantly based on a multitude of factors, but it's helpful to start with a baseline understanding of the national averages and typical ranges.
The most reliable sources for physician salary data are industry-specific reports that survey thousands of physicians directly. These provide a much more accurate picture than general salary aggregators.
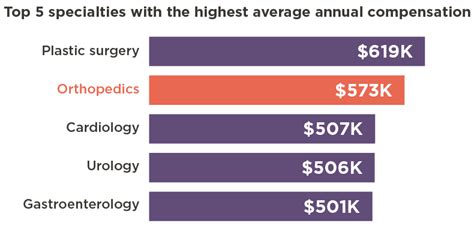
According to the 2023 Medscape Physician Compensation Report, the average salary for general surgeons (the closest broad category tracked) is $412,000. However, surgical oncology is a highly paid subspecialty within surgery. More specialized data provides a clearer view.
The Doximity 2023 Physician Compensation Report, which is highly regarded in the medical community, provides more granular data. While it doesn't always list "Surgical Oncology" as a standalone category every year, it often places it within the top tier of surgical subspecialties. Based on Doximity's data and other industry reports, a more accurate average salary for a surgical oncologist in the United States is approximately $559,000 per year.
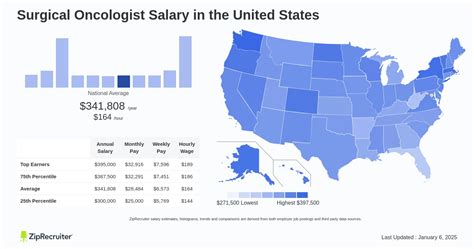
However, an average figure only tells part of the story. The salary range is vast:
- Entry-Level (Post-Fellowship): A surgical oncologist just finishing their fellowship and starting their first attending position can expect a starting salary in the range of $375,000 to $450,000. This is often a guaranteed salary for the first 1-2 years.
- Mid-Career (5-15 years of experience): With established expertise and a strong referral base, a mid-career surgical oncologist can see their income rise significantly, typically earning between $500,000 and $700,000.
- Senior/Late-Career (15+ years of experience): Highly experienced surgeons, especially those in leadership positions (e.g., Chief of Surgery) or partners in lucrative private practice groups, can earn $750,000 or more, with top earners in high-volume private practices potentially exceeding $1,000,000 annually.
Data from salary aggregators aligns with this, though with some variation. For instance, Salary.com reports the median salary for a surgical oncologist in the U.S. to be around $495,274 as of late 2023, with a typical range falling between $419,007 and $583,073. This likely under-represents the top end of the private practice market but provides a solid baseline.
### Surgical Oncologist Salary by Experience Level
The salary growth trajectory for a surgical oncologist is steep, especially in the first decade of practice. Here's a more detailed look at what to expect at each stage:
| Experience Level | Years in Practice | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Resident/Fellow | Training Years | $65,000 - $85,000 | This is the training period. Compensation is a standardized stipend set by the institution and is not reflective of attending-level pay. |
| Entry-Level Attending | 1-3 years | $375,000 - $475,000 | Recently completed fellowship. Typically on a guaranteed salary contract for the first 1-2 years while building a practice. |
| Early Mid-Career | 4-8 years | $480,000 - $600,000 | Transitioned to a productivity-based model (RVUs). Has an established reputation and a steady flow of patient referrals. |
| Peak Mid-Career | 9-20 years | $600,000 - $800,000+ | At the peak of their clinical skills and efficiency. May hold leadership roles or have partnership status in a private group. Highest earning potential. |
| Senior/Late-Career | 20+ years | $550,000 - $750,000+ | May begin to scale back clinical hours. Often involved in mentorship, administration, or research. Income may plateau or slightly decrease from peak levels but remains very high. |
*Note: These are estimates and can vary significantly based on the factors discussed in the next section.*
### Deconstructing the Compensation Package
A surgical oncologist's total compensation is more than just a base salary. Understanding the different components is crucial for evaluating job offers.
- Base Salary: This is the guaranteed portion of your income. In hospital-employed or academic models, this makes up a significant part of the total pay. In the first 1-2 years of a new job, the entire compensation might be a guaranteed base salary.
- Productivity Bonuses (RVU-Based Compensation): This is the most common model after the initial guarantee period. The surgeon earns Work Relative Value Units (wRVUs) for every patient encounter, procedure, and service they provide. The wRVU value for a procedure is set by Medicare and reflects the time, technical skill, and intensity required. The employer pays a certain dollar amount per wRVU earned above a specific threshold. For example, a contract might state a base salary of $400,000, representing 8,000 wRVUs, with a payment of $60 per wRVU earned beyond that. A highly productive surgeon who generates 11,000 wRVUs in a year would earn an additional $180,000 (3,000 x $60), for a total income of $580,000. This model directly rewards hard work and efficiency.
- Performance & Quality Bonuses: Many health systems are incorporating quality metrics into bonus structures. These can be tied to patient outcomes, patient satisfaction scores, adherence to clinical protocols, and citizenship within the hospital (e.g., committee participation). These typically represent a smaller portion of total income (5-15%).
- Signing Bonus: To attract top talent, particularly in underserved areas, hospitals and practices often offer substantial signing bonuses. These can range from $25,000 to $100,000 or more.
- Relocation Assistance: A stipend to cover the costs of moving, often between $10,000 and $20,000.
- Retirement Contributions: Generous 401(k) or 403(b) plans with employer matching are standard. Some private practice models may offer more complex profit-sharing or defined-benefit plans.
- Health and Disability Insurance: Comprehensive health, dental, vision, and, crucially, robust long-term disability and life insurance policies are part of any competitive package. "Own-occupation" disability insurance is a critical benefit for surgeons.
- CME Allowance: An annual stipend (e.g., $5,000 - $10,000) to cover the costs of attending medical conferences, subscribing to journals, and maintaining board certification.
- Malpractice Insurance: The employer almost always covers the full cost of medical malpractice insurance, which is extremely expensive for surgical specialties. "Tail coverage," which covers claims made after the surgeon leaves the practice, is a critical point of negotiation.
---
Key Factors That Influence a Surgical Oncologist's Salary

While the national averages provide a useful benchmark, a surgical oncologist's actual salary is a complex equation with many variables. Understanding these factors is essential for maximizing earning potential throughout one's career. This section delves into the most significant drivers of compensation.
### 1. Geographic Location
Where you practice medicine is arguably one of the most powerful determinants of your income. The dynamic is often counterintuitive: salaries are frequently highest in less "desirable" or more rural locations where the demand for specialists is high and the supply is low. Conversely, highly desirable metropolitan areas on the coasts may have a surplus of physicians, leading to more competition and comparatively lower (though still substantial) salaries.
The Doximity 2023 Physician Compensation Report highlights this trend across specialties. States in the Midwest and Southeast often offer the highest compensation to attract physicians.
- Top-Paying Regions/States: States like Wisconsin, Indiana, Georgia, Oklahoma, and Alabama often appear on lists of highest physician compensation. A surgical oncologist position in a mid-sized city in one of these states could command a salary 10-20% higher than the national average, as health systems must offer premium pay to recruit top-tier talent. For example, a position in Milwaukee might offer a starting package significantly higher than a similar one in Boston.
- Lower-Paying (but still high) Regions/States: States with major, desirable cities and a high concentration of academic medical centers, such as California, Massachusetts, New York, and Maryland, tend to have salaries closer to or slightly below the national average. The appeal of living in these areas, combined with a greater supply of specialists, tempers compensation levels. The cost of living in these areas is also substantially higher, which can erode the take-home value of the salary.
- Metropolitan vs. Rural Divide: Within a single state, there can be significant variation. A position in a rural or underserved community's regional medical center will almost always pay more than a position in that state's major metropolitan hub. The trade-off is often lifestyle, access to amenities, and professional collaboration opportunities.
Example Comparison:
- Surgical Oncologist in Indianapolis, IN: Potential Salary: $650,000+
- Surgical Oncologist in San Francisco, CA: Potential Salary: $525,000
While the San Francisco salary is lower, the competition for that job is fierce. Furthermore, the after-tax, after-cost-of-living income in Indianapolis would be vastly greater.
### 2. Practice Setting and Employment Model
The type of organization a surgeon works for profoundly impacts their compensation structure and earning ceiling. The traditional private practice model is becoming less common, with most new surgeons opting for hospital employment.
- Private Practice (Solo or Group): This model offers the highest earning potential. In a private practice, especially as a partner, the surgeon's income is directly tied to the group's revenue minus its overhead. Efficient, high-volume surgeons in a well-managed group can earn significantly more than their hospital-employed counterparts, often clearing $800,000 - $1,000,000+. However, this comes with the risks and responsibilities of running a business: managing staff, billing, insurance negotiations, marketing, and covering overhead costs (rent, salaries, malpractice).
- Hospital or Health System Employment: This is now the most common model for surgical oncologists. It offers stability, predictable income, and excellent benefits without the administrative headaches of running a business. The hospital handles billing, staffing, and overhead. Compensation is typically a base salary plus a productivity (wRVU) bonus. While the ceiling is generally lower than in private practice, it's a more secure and predictable path, with typical earnings falling in the $450,000 to $700,000 range.
- Academic Medical Centers: Surgeons at university hospitals and academic centers typically earn the least. According to Medscape, physicians in academic settings earn, on average, about 10-15% less than their counterparts in other settings. A surgical oncologist in academia might earn $375,000 to $550,000. The trade-off for lower pay is the opportunity to engage in cutting-edge research, teach medical students and residents, and build a national or international reputation through publications and presentations. The "currency" in academia is a mix of salary, prestige, and intellectual fulfillment.
- Government/VA Hospitals: Working for the Department of Veterans Affairs (VA) or other government entities offers exceptional job security, federal benefits, and a better work-life balance. However, compensation is generally lower than in other sectors and is based on a structured government pay scale.
### 3. Years of Experience and Reputation
As detailed in the previous section, experience is a primary driver of salary growth. This isn't just about time served; it's about the accumulation of expertise, efficiency, and reputation.
- The Learning Curve (Years 1-5): In the first few years, a surgeon is still refining their techniques, building speed in the operating room, and establishing a referral network with other physicians in the community. Their productivity, and thus their wRVU generation, will naturally be lower than a more seasoned surgeon.
- Peak Earning Years (Years 6-20): A mid-career surgeon has an established name. Referring physicians (gastroenterologists, primary care doctors, medical oncologists) trust them with their most complex cases. They are highly efficient in the OR, able to handle a greater volume of complex cases, which directly translates to higher wRVU generation and, therefore, higher income.
- Senior Leadership (Years 20+): While clinical volume might decrease slightly, senior surgeons often take on paid leadership and administrative roles that supplement their clinical income. These can include being the Chief of Surgery, a Service Line Director, or serving on key hospital committees, all of which come with stipends or salary increases.
### 4. Area of Sub-Specialization
Surgical oncology itself is a specialty, but many practitioners further sub-specialize, focusing on specific disease sites. This can impact compensation based on the complexity and volume of procedures associated with that area.
- High-Complexity/High-RVU Sub-specialties: Fields that involve highly complex, long operations tend to generate more wRVUs and thus higher compensation. Examples include:
- Hepatobiliary (HPB) Surgery: Procedures like liver resections and the Whipple procedure (pancreaticoduodenectomy) are among the most complex in surgery and have very high wRVU values.
- Thoracic Surgical Oncology: Removing cancers of the lung and esophagus.
- Complex Gynecologic Oncology/Pelvic Exenteration: Extremely radical surgeries for advanced cancers.
- High-Volume Sub-specialties:
- Breast Surgical Oncology: While individual procedures may have lower wRVU values than an HPB case, breast cancer is very common. A dedicated breast surgeon can perform a high volume of procedures (lumpectomies, mastectomies, lymph node biopsies), leading to very high overall productivity and excellent compensation.
- Niche Sub-specialties:
- Melanoma/Sarcoma: These surgeons perform wide local excisions, complex limb-sparing surgeries, and lymph node dissections. Compensation is generally strong and depends heavily on the volume and complexity of cases in their referral area.
### 5. In-Demand Skills and Procedural Expertise
Beyond general board certification, specific technical skills can make a surgeon more valuable to a health system and command a higher salary.
- Robotic Surgery Proficiency: Expertise in using the da Vinci Surgical System is no longer a novelty; it's often a requirement. Surgeons proficient in robotic techniques for colorectal, thoracic, or HPB surgery are in high demand. Hospitals invest millions in these systems and need surgeons who can use them effectively to market their cancer programs.
- Minimally Invasive Techniques: Advanced laparoscopic skills are similarly valuable. These techniques lead to shorter hospital stays and faster patient recovery, which are key metrics for hospitals.
- HIPEC and Other Advanced Procedures: Expertise in niche, complex procedures like Hyperthermic Intraperitoneal Chemotherapy (HIPEC) can make a surgeon a regional draw, bringing patients and revenue to the hospital. This unique skill set can be leveraged for higher compensation.
- Leadership and Administrative Acumen: As mentioned, a willingness and ability to take on leadership roles is a clear path to increased income. This involves skills beyond the OR, such as budget management, strategic planning, and personnel management.
---
Job Outlook and Career Growth for Surgical Oncologists

The long-term career outlook for surgical oncologists is exceptionally strong and stable. This positive forecast is driven by a combination of demographic trends, technological advancements, and the fundamental role these specialists play in modern medicine.
### Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) provides projections for physicians and surgeons as a broad category. For the decade spanning 2022-2032, the BLS projects a 3% growth rate for this group, which is about as fast as the average for all occupations. However, this general number belies the specific, more robust demand for specialists like surgical oncologists.
The key drivers fueling the demand are:
1. An Aging Population: The primary risk factor for most cancers is age. As the massive Baby Boomer generation continues to age, the incidence of cancer is projected to rise significantly. The American Cancer Society estimates over 2 million new cancer cases will be diagnosed in 2024 alone. This demographic reality creates a sustained and growing need for all oncology specialists.
2. Advances in Treatment: Paradoxically, better treatments are increasing the demand for surgical oncologists. Improved systemic therapies (chemotherapy, immunotherapy, targeted therapy) can now shrink previously inoperable tumors to a point where surgery becomes a viable, curative option. This expands the pool of patients who can benefit from a surgical oncologist's skills.
3. Physician Shortages: The Association of American Medical Colleges (AAMC) continues to project significant physician shortages across the U.S., including in surgical specialties. As a generation of surgeons nears retirement, there will be a pressing need to replace them, creating ample opportunities for those entering the field.
In short, the need for surgical oncologists is not expected to diminish. The demand is stable and likely to grow, ensuring excellent job security for those who complete the rigorous training path.
### Emerging Trends and Future Challenges
The field of surgical oncology is not static. It is constantly evolving, and success in the future will depend on adapting to new trends and overcoming challenges.
Emerging Trends:
- The Rise of Neoadjuvant Therapy: The trend is shifting toward giving systemic therapy *before* surgery. This requires the surgical oncologist to be even more integrated with the medical oncology team. It also means that surgeons will increasingly operate on patients who have already responded to therapy, which can alter the surgical field and require new approaches.
- Liquid Biopsies and Precision Medicine: The ability to detect circulating tumor DNA (ctDNA) in the blood may revolutionize how cancer is diagnosed, monitored for recurrence, and treated. Surgeons will need to understand and integrate these technologies into their decision-making. For example, a positive ctDNA test after surgery might prompt more aggressive adjuvant therapy.
- Enhanced Role of Artificial Intelligence (AI): AI is poised to impact surgical oncology in several ways:
- Image Analysis: AI algorithms may help radiologists and surgeons better interpret scans, identifying subtle patterns of spread that are invisible to the human eye.
- Surgical Planning: AI could help plan the optimal surgical approach based on a patient's unique anatomy and tumor characteristics.
- Robotic Surgery: AI will be further integrated into robotic platforms, potentially providing real-time feedback, enhancing precision, and automating certain routine tasks.
- De-escalation of Surgery: For some cancers (e.g., certain rectal and breast cancers), research is exploring whether excellent responses to chemotherapy and radiation might allow for a "watch and wait" approach, avoiding major surgery altogether. Successful surgeons will be those who lead these trials and can judiciously determine which patients truly need an operation.
Future Challenges:
- Burnout: The intense demands of the job—long hours, high emotional stress, and administrative burdens—put surgical oncologists at high risk for burnout. Maintaining work-life balance is a critical, ongoing challenge.
- Healthcare Economics: The pressure to control healthcare costs is immense. Surgeons will face increasing scrutiny over the cost-effectiveness of procedures and will need to demonstrate value through excellent outcomes.
- Keeping Pace with Science: The science of oncology is advancing at an explosive rate. Lifelong learning is not just a suggestion; it's a requirement to provide state-of-the-art care.
### How to Stay Relevant and Advance in the Field
Advancement in surgical oncology can take many forms: clinical excellence, academic leadership, or administrative power.
- **Become a Master Clin