Table of Contents

- [Introduction: The Demanding Path to a Rewarding Career](#introduction)
- [What Does a Surgeon Do? A Glimpse Behind the Scrubs](#what-does-a-surgeon-do)
- [Average Surgeon Salary: A Deep Dive into Compensation](#average-surgeon-salary)
- [Key Factors That Influence a Surgeon's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Surgeons](#job-outlook-and-career-growth)
- [How to Become a Surgeon: Your Step-by-Step Roadmap](#how-to-become-a-surgeon)
- [Conclusion: Is the Long Journey to Becoming a Surgeon Worth It?](#conclusion)
Introduction: The Demanding Path to a Rewarding Career

For many, the word "surgeon" evokes images of high-stakes operating rooms, life-saving procedures, and an unparalleled level of medical expertise. It's a profession that sits at the apex of healthcare, demanding a unique combination of intellectual rigor, manual dexterity, and profound resilience. The journey is famously long and arduous, a crucible of education and training that forges some of the most skilled professionals in the world. But for those with the calling, the rewards—both intrinsic and financial—are substantial. If you're standing at the beginning of this path, wondering what lies at the end of more than a decade of preparation, one of the most practical questions on your mind is undoubtedly: what is a surgeon's starting salary?
While the figures are impressive, they represent the culmination of immense investment. A first-year attending surgeon, fresh out of residency or fellowship, can expect a starting salary that often ranges from $250,000 to over $500,000, depending heavily on their chosen specialty, the location of their practice, and the type of institution they join. This number, however, is just the beginning of a steep upward trajectory. I once had the privilege of speaking with a recently graduated neurosurgery resident. He described his first paycheck not as a prize, but as the first tangible return on a decade-long investment of sleepless nights, missed life events, and hundreds of thousands of dollars in educational debt. It was a powerful reminder that in this field, compensation is directly tied to an almost unimaginable level of dedication and sacrifice.
This article serves as your definitive guide to understanding a surgeon's compensation, career path, and the future of the profession. We will dissect not only the starting salaries but every factor that shapes a surgeon's earning potential over a lifetime. From the impact of your chosen specialty to the financial nuances of different practice models, we will provide a comprehensive, data-driven look at what it truly means to build a career in surgery. Whether you are a high school student with a dream, a pre-med undergraduate, or a medical student weighing your options, this guide will equip you with the knowledge to make informed decisions about one of society's most challenging and respected careers.
What Does a Surgeon Do? A Glimpse Behind the Scrubs
At its core, a surgeon is a physician who specializes in treating diseases, injuries, and deformities through operative procedures. They are masters of anatomy, pathology, and critical care, using invasive, minimally-invasive, or non-invasive surgical methods to physically alter body tissues and organs. However, the dramatic moments in the operating room (OR) that are so often glamorized in media represent only a fraction of a surgeon's comprehensive responsibilities. Their work is a meticulous blend of diagnosis, patient consultation, procedural execution, and long-term post-operative management.
Core Roles and Responsibilities:
- Diagnosis and Patient Evaluation: Before a scalpel is ever considered, a surgeon's primary role is to be an expert diagnostician. They review patients' medical histories, conduct physical examinations, and interpret complex imaging studies (X-rays, CT scans, MRIs) and lab results to determine the necessity and feasibility of a surgical intervention.
- Pre-Operative Care: This involves detailed consultations with patients and their families. The surgeon explains the diagnosis, the proposed procedure, the potential risks and benefits, and alternative treatment options. This is a critical phase for building trust and ensuring the patient provides informed consent.
- Surgical Performance: This is the technical heart of the job. Surgeons lead a highly skilled team—including anesthesiologists, surgical nurses, and technicians—to perform the operation. This requires immense concentration, precision, and the ability to make critical decisions under pressure, especially when unexpected complications arise.
- Post-Operative Management: A surgeon's responsibility does not end when the final suture is placed. They meticulously monitor the patient's recovery, manage pain, address complications like infections or bleeding, and oversee the rehabilitation process. This includes follow-up appointments that can continue for weeks, months, or even years.
- Collaboration and Administration: Surgeons work as part of a larger healthcare ecosystem. They collaborate with primary care physicians, specialists, radiologists, and pathologists. Many also take on administrative duties, such as serving on hospital committees, participating in peer reviews, and managing the business aspects of a private practice.
- Continuous Learning and Research: Medicine is constantly evolving. Surgeons must dedicate significant time to staying abreast of the latest surgical techniques, technologies (like robotics and AI-assisted imaging), and research findings. Many academic surgeons also conduct their own research and publish in medical journals to advance the field.
### A Day in the Life: Dr. Eva Rostova, General Surgeon
To make this tangible, let's follow a hypothetical day for Dr. Eva Rostova, a general surgeon in her fifth year of practice at a mid-sized community hospital.
- 5:30 AM - Wake-Up & Review: Dr. Rostova is up before the sun. She checks her phone for any urgent overnight pages from the hospital while having a quick coffee. She mentally reviews her day: two scheduled surgeries, a block of afternoon clinic appointments, and hospital rounds.
- 6:30 AM - Hospital Rounds: She arrives at the hospital and begins rounding on her post-operative patients. She visits a patient who had a colectomy two days ago, checking his vitals, examining the incision site, and speaking with the floor nurse about his pain management. She then sees a patient she operated on yesterday for an emergency appendectomy, confirming he is stable for discharge later today.
- 7:45 AM - Pre-Op for First Case: Dr. Rostova heads to the pre-operative holding area to meet her first patient of the day: a 65-year-old man scheduled for a laparoscopic cholecystectomy (gallbladder removal). She greets him and his anxious wife, answers their last-minute questions, confirms the surgical plan, and makes a final mark on the surgical site.
- 8:15 AM - 10:00 AM - Surgery #1: In the OR, she leads the "time-out"—a final safety check where the entire team confirms the patient's identity, the procedure, and the surgical site. The surgery proceeds smoothly. Dr. Rostova expertly navigates the laparoscopic instruments, her movements precise and efficient while she communicates calmly with the anesthesiologist and her team.
- 10:00 AM - 10:30 AM - Post-Op and Charting: After speaking with the patient's family, she dictates her operative notes, detailing every step of the procedure, her findings, and the post-operative plan. Accuracy here is paramount for patient care, billing, and legal records.
- 10:30 AM - 1:00 PM - Surgery #2 (Emergency): Just as she's about to grab a quick lunch, the Emergency Department pages her. A 30-year-old victim of a car accident has internal bleeding. Her scheduled hernia repair is postponed. Dr. Rostova rushes to the ED, quickly assesses the patient and the trauma scans, and makes the call: an emergency exploratory laparotomy is needed immediately. This surgery is tense and unpredictable, requiring her to rapidly identify and repair a splenic laceration to save the patient's life.
- 1:30 PM - 5:00 PM - Afternoon Clinic: After a whirlwind emergency case, she transitions to her outpatient clinic. Here, the pace is different but equally demanding. She sees a mix of new patient consultations for issues like hernias and GERD, and post-op follow-ups for patients she operated on weeks ago, checking their healing and progress. Each 15-20 minute slot is a focused interaction of examination, explanation, and planning.
- 5:00 PM - 6:30 PM - Administrative Tasks: The last patient has left, but the day isn't over. Dr. Rostova has a mountain of paperwork: reviewing lab results, signing off on charts, answering messages from referring physicians, and dealing with insurance pre-authorization requests.
- 6:30 PM - Homeward Bound (On Call): She finally leaves the hospital, but she's not truly off the clock. She is the surgeon on call for the night, meaning any surgical emergency that comes into the hospital is her responsibility. Her phone stays on, and she knows that a call could send her rushing back to the OR at any moment.
This depiction, while intense, is a realistic portrayal of the immense scope of a surgeon's duties, extending far beyond the sterile confines of the operating room.
Average Surgeon Salary: A Deep Dive into Compensation
Surgeons are among the highest-paid professionals in any industry, a reflection of their extensive education, specialized skills, long hours, and the high-stakes nature of their work. However, the term "surgeon salary" is incredibly broad. Compensation varies dramatically based on specialty, location, experience, and practice type. Understanding these nuances is key to grasping the full financial landscape of a surgical career.
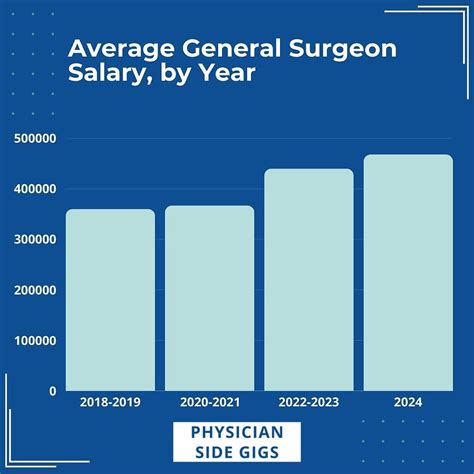
It's crucial to distinguish between a surgeon's starting salary—what a physician earns in their first year after completing residency—and the average salary for all surgeons, which includes those with decades of experience.
- Surgeon Starting Salary (First Year): A surgeon just finishing their training (typically in their early to mid-30s) can expect to earn anywhere from $250,000 to over $500,000. General surgeons may start in the $250,000 to $350,000 range, while those in high-demand, high-reimbursement specialties like neurosurgery or orthopedic surgery can command starting offers exceeding $500,000 or even $600,000, particularly in underserved areas.
- Overall Average Surgeon Salary: When all experience levels are averaged, the figures are significantly higher. Different sources provide slightly different data, but all point to a lucrative profession.
- U.S. Bureau of Labor Statistics (BLS): The BLS groups "Physicians and Surgeons, All Other" and "Surgeons, Except Ophthalmologists" together. As of May 2022, the BLS reports that the median annual wage for this group was greater than or equal to $239,200 per year. The BLS data often appears lower than industry-specific reports because it has an upper limit on its reporting scale and may not fully capture bonuses and other compensation.
- Doximity 2023 Physician Compensation Report: This report, based on data from over 190,000 U.S. physicians, is a highly respected industry source. It shows an average annual compensation for all surgeons in the U.S. at $402,233. However, it breaks this down by specialty, with Neurosurgery ($788,313) and Thoracic Surgery ($706,775) at the top.
- Medscape Physician Compensation Report 2023: This is another key industry report. It found the average overall physician salary was $352,000, but specialists earned far more ($382,000 on average). For surgeons specifically, the average income was $404,000. Plastic surgeons averaged $619,000, and orthopedic surgeons averaged $573,000.
- Salary.com: As of late 2023, Salary.com reports the median salary for a General Surgeon in the United States is $447,290, with the salary range typically falling between $378,390 and $531,390.
### Surgeon Salary by Experience Level
Salary growth in surgery is significant after the initial post-residency years. A surgeon's value increases as they build a reputation, refine their skills, become more efficient in the OR, and develop a referral network.
| Career Stage | Years of Experience | Typical Annual Salary Range | Key Drivers |
| :--- | :--- | :--- | :--- |
| Entry-Level (Attending Year 1-3) | 0-3 years post-residency/fellowship | $250,000 - $550,000+ | Initial contract, often with a guaranteed base salary. Negotiating power depends heavily on specialty and location. |
| Mid-Career (Attending Year 4-10) | 4-10 years post-residency | $350,000 - $750,000+ | Transition from guaranteed salary to productivity-based models (RVUs). Reputation is established, surgical volume increases. Potential for partnership in private practice. |
| Senior/Late-Career (Attending Year 11+) | 11+ years post-residency | $400,000 - $1,000,000+ | Peak earning years. Highly efficient, strong referral base. May take on leadership roles (Chief of Surgery), which come with stipends. Some may scale back clinical work, affecting income. |
*Note: These are general estimates. A neurosurgeon could easily exceed $1M annually in their mid-career, while a general surgeon in a lower-paying state may peak around $450,000.*
### Beyond the Base Salary: Understanding the Full Compensation Package
A surgeon's income is rarely just a flat salary. The total compensation package is a complex mix of components that can significantly increase a surgeon's take-home pay and overall financial well-being.
- Base Salary: This is the guaranteed portion of pay. In the initial years of practice, this is often the largest component. Hospital-employed surgeons and those in academic medicine typically have a more predictable base salary.
- Productivity Bonuses (RVU-Based Compensation): This is the most common model after the first few years. Compensation is tied to Work Relative Value Units (wRVUs). An RVU is a measure of physician work assigned by Medicare to every medical procedure and service. The more complex and time-consuming the surgery, the more wRVUs it generates. The surgeon is paid a certain dollar amount per wRVU they generate, incentivizing efficiency and a high volume of work.
- Sign-On Bonus: To attract top talent, especially in high-need areas or specialties, hospitals and practices offer substantial sign-on bonuses. These can range from $20,000 to well over $100,000.
- Performance Bonuses: These can be tied to quality metrics, such as patient outcomes, low complication rates, and patient satisfaction scores.
- Profit Sharing / Partnership Track (Private Practice): In private practice, after a few years as an employee, a surgeon may be offered the opportunity to "buy-in" and become a partner. This means they share in the practice's profits, which can lead to a significant increase in income but also involves taking on business risk and administrative responsibility.
- Relocation Assistance: Often called a "relocation stipend," this is a payment (e.g., $10,000 - $15,000) to cover the costs of moving to a new city for the job.
- Student Loan Repayment: Given the enormous debt burden of medical school (often $200,000-$400,000), student loan repayment assistance is a highly attractive benefit. Some employers, particularly in underserved rural or urban areas, may offer tens or even hundreds of thousands of dollars in loan forgiveness over a set number of years.
- Benefits Package:
- Health, Dental, and Vision Insurance: Comprehensive plans for the surgeon and their family.
- Retirement Plans: Access to 401(k) or 403(b) plans, often with a generous employer match.
- Malpractice Insurance: This is a critical and expensive necessity. The employer almost always covers the full cost of "occurrence-based" or "claims-made" malpractice policies, which can be worth tens of thousands of dollars per year.
- Continuing Medical Education (CME) Stipend: An annual allowance (e.g., $5,000 - $15,000) to cover the costs of attending conferences, subscribing to journals, and other activities required to maintain medical licensure.
- Paid Time Off (PTO): Typically 4-6 weeks of vacation, though taking it can be challenging due to call schedules and patient loads.
When evaluating a job offer, a surgeon must look beyond the base salary and consider the entire financial picture, as these additional components can add well over $100,000 in value annually.
Key Factors That Influence a Surgeon's Salary
A surgeon's salary is not a monolith. It is a dynamic figure shaped by a confluence of factors. Two surgeons graduating from the same residency program can have wildly different incomes just a few years later based on the choices they make and the environment they practice in. This section provides an exhaustive breakdown of the variables that have the most significant impact on a surgeon's earnings.
### 1. Area of Specialization
This is, by far, the most significant determinant of a surgeon's earning potential. The differences between specialties can be hundreds of thousands of dollars annually. This variation is driven by several forces: the complexity and risk of procedures, the reimbursement rates from Medicare and private insurers, the length and competitiveness of the required training (residency and fellowship), and patient demand.
Below is a comparative look at average annual compensation for various surgical specialties, based on data from the Doximity, Medscape, and MGMA reports.
| Surgical Specialty | Average Annual Salary Range | Notes on the Specialty |
| :--- | :--- | :--- |
| Neurosurgery | $600,000 - $900,000+ | Consistently the highest-paid specialty. Involves incredibly complex and high-risk operations on the brain and spinal cord. Very long residency (7 years). |
| Thoracic Surgery | $550,000 - $850,000+ | Focuses on the heart, lungs, esophagus, and other organs in the chest. Includes cardiac surgeons. High-risk, high-reimbursement procedures. |
| Orthopedic Surgery | $500,000 - $750,000+ | Specializes in the musculoskeletal system. High volume of lucrative procedures like joint replacements (hip, knee), spine surgery, and sports medicine. |
| Plastic Surgery | $450,000 - $700,000+ | Wide range. Reconstructive surgery is medically necessary and reimbursed by insurance. Cosmetic surgery is often cash-based, offering very high income potential. |
| Vascular Surgery | $400,000 - $650,000+ | Deals with diseases of the arterial, venous, and lymphatic systems. Often involves a mix of high-acuity emergencies and chronic patient management. |
| Urology | $400,000 - $600,000+ | Treats conditions of the male and female urinary tract and male reproductive organs. Good mix of clinical and surgical work, with many well-reimbursed procedures. |
| Otolaryngology (ENT) | $380,000 - $550,000+ | Focuses on conditions of the ear, nose, and throat. Broad scope, with potential for lucrative subspecialties like facial plastics or head and neck cancer surgery. |
| General Surgery | $350,000 - $500,000+ | The "workhorse" of surgery. Broad practice covering the abdomen, digestive tract, and endocrine system. Often the baseline against which other specialties are measured. |
| Ophthalmology | $350,000 - $500,000+ | Surgical and medical care of the eyes. High-volume, quick, and well-reimbursed procedures like cataract surgery can be very profitable. |
| Obstetrics & Gynecology (OB/GYN)| $300,000 - $450,000+ | A unique blend of primary care, medicine, and surgery. Salaries are generally lower than other surgical specialties due to a larger primary care component and higher malpractice insurance costs. |
### 2. Geographic Location
Where a surgeon chooses to practice has a profound impact on their income. This is not simply a matter of cost of living; it's a dynamic of supply and demand. Large, desirable metropolitan areas like New York City, Los Angeles, and Chicago have a high concentration of surgeons, which creates competition and can drive down compensation relative to the high cost of living.
Conversely, less populated states and rural areas often struggle to attract and retain specialized medical talent. To incentivize surgeons to practice there, hospitals and health systems in these regions offer significantly higher salaries, larger sign-on bonuses, and robust student loan repayment packages.
Highest-Paying States/Regions (According to Doximity and other reports):
- Midwest and Southeast: States like Alabama, Kentucky, Oklahoma, Indiana, and Missouri consistently rank among the highest for physician compensation. They combine a lower cost of living with high demand.
- The Dakotas: Both North and South Dakota often appear in the top 10 due to a severe shortage of specialists.
- Wisconsin & Iowa: Strong private practice and hospital systems in these states actively recruit with competitive salaries.
Lowest-Paying States/Regions:
- Northeast: States like Maryland, Massachusetts, and Rhode Island, along with Washington D.C., tend to have the lowest average physician compensation. This is due to a high density of physicians (due to many prestigious academic centers), a higher cost of living, and sometimes lower reimbursement rates from dominant local insurers.
- Pacific Coast: While salaries in California may look high in absolute terms, they are often lower when adjusted for the exceptionally high cost of living, especially in coastal cities.
Example Salary Variation for an Orthopedic Surgeon:
- Charlotte, NC: Average salary might be $620,000
- Des Moines, IA: Average salary might be $605,000
- Boston, MA: Average salary might be $510,000
- San Francisco, CA: Average salary might be $540,000 (but with a vastly higher cost of living than the other cities)
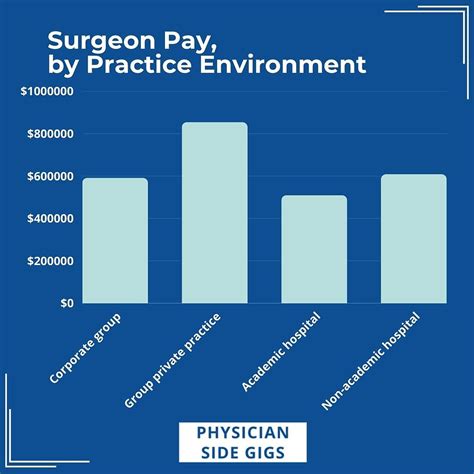
### 3. Practice Type and Employment Model
The setting in which a surgeon works is a critical factor in their compensation structure and overall income.
- Private Practice (Physician-Owned): This model offers the highest long-term earning potential.
- Partner/Owner: Partners share in the profits of the entire practice, including revenue from surgery, clinic visits, and ancillary services like physical therapy or imaging centers. Their income can easily surpass $1,000,000 in some specialties, but they also bear the risks and headaches of running a business (managing staff, billing, overhead, marketing).
- Employee: A surgeon may work as an employee in a private practice, often on a partnership track. They receive a salary plus productivity bonus but don't share in the overall profits until they become a partner.
- Hospital or Health System Employee: This is now the most common employment model. The surgeon is a direct employee of the hospital.
- Pros: High degree of stability, predictable salary (at least initially), no business management responsibilities, excellent benefits, and the hospital covers overhead and malpractice insurance.
- Cons: Less autonomy, earning potential is often capped compared to private practice ownership, and compensation is heavily tied to productivity metrics (wRVUs) that can feel like a treadmill.
- Academic Medical Center: Surgeons at universities work in a tripartite mission: clinical care, teaching, and research.
- Pros: Prestige, opportunities to teach medical students and residents, dedicated time for research, and access to cutting-edge technology.
- Cons: Compensation is almost always lower than in private practice or even some community hospital settings. A portion of their "salary" comes from research grants and institutional funds. The trade-off is lifestyle and academic impact for pure income. A general surgeon at a top university might make $300,000, while their counterpart in a rural private practice makes $450,000.
- Government Employment (e.g., VA Hospitals, Military): Surgeons working for the Department of Veterans Affairs or as active-duty military physicians have the most predictable salaries and exceptional federal benefits, including pensions.
- Pros: Incredible job security, regular hours (less so for military surgeons on deployment), and a sense of service.
- Cons: Salaries are significantly lower than in the private sector. The compensation structure is rigid and based on government pay scales, not productivity.
- Locum Tenens: This involves working as a temporary, independent contractor to fill in for surgeons who are on vacation, on leave, or to cover staffing shortages.
- Pros: Very high daily or weekly pay rates, travel expenses covered, and extreme flexibility. A way to "test out" different locations or practice types.
- Cons: No job stability, no benefits (have to buy your own health and malpractice insurance), and constant travel.
### 4. Years of Experience and Reputation
As detailed in the previous section, experience is a powerful driver of salary. An entry-level surgeon is still building speed, efficiency, and a referral base. A surgeon with 10 years of experience has a well-oiled practice, a strong reputation among referring physicians, and the skills to handle more complex cases efficiently. This translates directly into higher productivity and, therefore, higher income in most compensation models. Reputation is an intangible but critical asset; the "go-to" spine surgeon or breast cancer surgeon in a region will have a full schedule and the negotiating leverage that comes with it.
### 5. In-Demand Skills and Sub-Subspecialization
Within a given specialty, possessing a niche skill set can significantly boost income.
- Robotic Surgery Proficiency: Surgeons proficient with surgical robots (like the da Vinci system) are in high demand. Hospitals invest millions in these systems and need surgeons who can use them effectively to market their "advanced surgical care." This skill can be a major negotiating point for a higher starting salary.
- Minimally Invasive Techniques: Expertise in laparoscopic, arthroscopic, or endovascular techniques is highly valued. These procedures often lead to faster patient recovery, lower complication rates, and are preferred by patients, making surgeons who master them more valuable.
- Complex Niche Procedures: An orthopedic surgeon who sub-specializes in complex hip revisions, a neurosurgeon who focuses on skull base tumors, or a general surgeon who is an expert in advanced hernia repairs will command higher salaries and attract referrals from a wider geographic area. These fellowship-trained skills set them apart from their peers.
- Leadership and Administrative Skills: Surgeons who take on roles like Chief of Surgery, Medical Director of the OR, or Trauma Medical Director receive an administrative stipend on top of their clinical income. These roles also position them for executive leadership positions (like Chief Medical Officer) later in their careers.
Job Outlook and Career Growth for Surgeons
For those embarking on the long journey to become a surgeon, the future of the profession is a critical consideration. The good news is that the demand for skilled surgeons is projected to remain strong and even grow, driven by demographic shifts, technological advancements, and the ever-present need for medical care.
### Job Growth Projections
The U.S.
