Introduction

In the controlled chaos of an emergency room, as the frantic beat of a heart monitor cuts through the air, one figure stands as the epicenter of calm and decisive action: the trauma surgeon. This is a profession not for the faint of heart, but for those who run toward the fire, armed with a scalpel, immense knowledge, and an unwavering commitment to snatching life from the jaws of death. For aspiring medical professionals drawn to the highest stakes in medicine, the career of a trauma surgeon represents the pinnacle of skill, pressure, and impact.
But beyond the profound personal satisfaction, a career of such intensity and dedication comes with significant financial rewards. A trauma surgeon's salary reflects the decade-plus of rigorous training, the life-or-death responsibility, and the round-the-clock demands of the job. Nationally, the average trauma surgeon salary sits comfortably in the high six-figure range, typically between $350,000 and $600,000, with the potential to exceed $750,000 for experienced surgeons in high-demand areas.
I once spoke with a seasoned trauma surgeon who, after a grueling 24-hour shift, told me, “The money is a necessary byproduct of the sacrifice. But the real compensation is handing a life back to a family that thought they’d lost it forever.” This sentiment captures the dual nature of the career: it is both a noble calling and a highly compensated profession. This guide will provide an exhaustive analysis of the trauma surgeon salary, the factors that shape it, and the long road required to earn the title. We will dissect every component of compensation, explore the job outlook, and provide a clear, step-by-step roadmap for those brave enough to answer the call.
### Table of Contents
- [What Does a Trauma Surgeon Do?](#what-does-a-trauma-surgeon-do)
- [Average Trauma Surgeon Salary: A Deep Dive](#average-trauma-surgeon-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Trauma Surgeon Do?

While the term "trauma doctor" is commonly used, the specific role we are analyzing is that of a Trauma Surgeon. These are highly specialized physicians who have completed a full general surgery residency followed by advanced fellowship training in surgical critical care and trauma surgery. Their expertise lies in the operative and medical management of patients with severe, life-threatening injuries, typically resulting from physical trauma such as car accidents, falls, gunshot wounds, or other violent incidents.
A trauma surgeon’s work environment is almost exclusively a hospital, specifically one with a designated Trauma Center. These centers are categorized by level (Level I to Level V), with Level I centers providing the highest level of comprehensive surgical care to trauma patients and often serving as academic hubs for teaching and research.
The core of their responsibility is to lead the trauma team in the "golden hour"—the critical period immediately following a traumatic injury where prompt medical and surgical treatment has the highest likelihood of preventing death.
Core Responsibilities and Daily Tasks:
- Initial Resuscitation and Assessment: When a "trauma alert" is activated, the trauma surgeon leads a team of emergency physicians, nurses, and other specialists. They perform a rapid, systematic evaluation of the patient (the ABCDEs: Airway, Breathing, Circulation, Disability, Exposure) to identify and address immediate life threats.
- Diagnostic Procedures: They are proficient in point-of-care ultrasound (like the FAST exam) to rapidly detect internal bleeding, and they interpret complex imaging like CT scans to diagnose injuries.
- Operative Intervention: This is the heart of the job. Trauma surgeons perform a wide range of emergency procedures, including:
- Damage Control Laparotomy: Opening the abdomen to control bleeding and contamination from organ injuries.
- Thoracotomy: Opening the chest to address injuries to the heart, lungs, or major blood vessels.
- Vascular Repair: Mending severed arteries and veins to restore blood flow.
- Splenectomy/Nephrectomy: Removing a shattered spleen or kidney.
- Critical Care Management: The job doesn't end in the operating room. Trauma surgeons manage their patients in the Surgical Intensive Care Unit (SICU), overseeing ventilators, complex medication regimens, and nutritional support.
- Clinic and Follow-up: They also see patients in an outpatient clinic for post-discharge follow-up, ensuring their long-term recovery is on track.
### A Day in the Life of a Trauma Surgeon (On-Call)
6:00 AM: Arrive at the hospital. Round on existing patients in the SICU and on the surgical floor. Review overnight events, lab results, and imaging with the resident team. Adjust ventilator settings for one patient and plan for a minor follow-up procedure on another.
8:30 AM: "Trauma Alert, Level I, ETA 5 minutes. 24-year-old male, driver in a high-speed motor vehicle collision, hypotensive, GCS 8." The overhead page cuts through the morning calm. The team assembles in the trauma bay.
8:35 AM: The patient arrives. The surgeon leads the primary survey, rapidly assessing for life-threatening injuries. The FAST exam shows fluid in the abdomen. The patient is unstable. The decision is made instantly: "We're going to the OR, now."
9:00 AM - 11:30 AM: In the Operating Room. The surgeon performs an emergency laparotomy, identifying and controlling bleeding from a liver laceration and repairing a mesenteric tear. The patient is stabilized using a "damage control" approach, with the abdomen temporarily left open for a planned second look in 24-48 hours.
12:00 PM: Post-op debrief with the team and a quick, tense conversation with the patient's family. Documentation of the complex procedure begins.
1:30 PM: A second "Trauma Alert" comes in. This time it's a construction worker who fell three stories. The cycle begins again, leading to another complex case involving orthopedic and neurosurgical consultations.
5:00 PM: Evening rounds on all patients. Writing orders, checking on the post-op patients, and teaching a medical student how to properly assess a chest tube.
8:00 PM - 5:00 AM (The Long Night): The "on-call" period is a mix of managing ongoing patient issues, consulting on other patients in the ER, and responding to any new trauma alerts that may arise. Sleep is fragmented, often interrupted by the piercing sound of the trauma pager. This is the reality of being the ultimate safety net for the critically injured.
Average Trauma Surgeon Salary: A Deep Dive
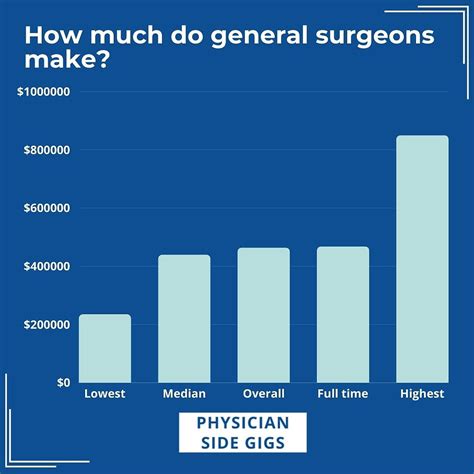
The compensation for trauma surgeons is among the highest in the medical field, a direct reflection of the extensive training, demanding lifestyle, and high-stakes nature of the work. Salary data varies based on the source, but a clear picture emerges when multiple authoritative sources are synthesized.
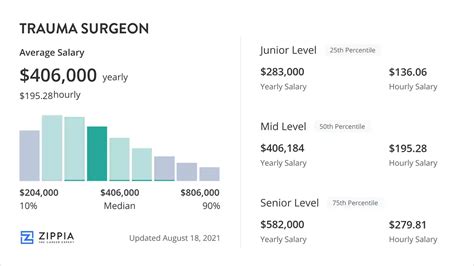
According to the 2023 Medscape Physician Compensation Report, surgeons in general earn an average of $402,000 annually. However, specialized fields like trauma surgery often command higher salaries. More specific data from salary aggregators provides a clearer view:
- Salary.com reports the median salary for a Trauma Surgeon in the United States as $454,031 as of late 2023, with a typical range falling between $395,296 and $537,130.
- Payscale.com lists a similar average base salary of around $396,000, with total pay packages often exceeding $500,000 when bonuses and other compensation are included.
- Doximity's 2023 Physician Compensation Report, a comprehensive analysis based on survey data from over 190,000 U.S. physicians, consistently places surgical specialties in the top-tier of earners. While it doesn't isolate trauma surgery specifically, "Surgical Critical Care" and "General Surgery" fall within a range that aligns with other sources, often between $400,000 and $550,000.
It's crucial to understand that these figures are national averages. A surgeon's actual take-home pay can be significantly higher or lower based on a multitude of factors discussed in the next section.
### Salary Brackets by Experience Level
A trauma surgeon's earning potential grows substantially with experience. The initial post-fellowship years are a period of building skills and reputation, which translates directly into higher compensation over time.
| Experience Level | Typical Years of Experience | Average Annual Salary Range | Key Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 Years | $300,000 - $420,000 | Fresh out of fellowship. Often includes a significant sign-on bonus and student loan repayment assistance. Salary may be lower in prestigious academic centers. |
| Mid-Career | 4-10 Years | $400,000 - $550,000 | Has established a strong clinical reputation. More efficient in the OR and managing patients. May take on leadership roles (e.g., assistant trauma director) and participate in more lucrative call schedules. |
| Senior/Experienced| 11-20+ Years | $500,000 - $750,000+ | At the peak of their career. Often holds a major leadership position like Trauma Medical Director or Chief of Surgery. May have a highly favorable compensation structure based on productivity (RVUs) or a stake in a private practice. |
*Sources: Data compiled and synthesized from Salary.com, Medscape, and industry-specific hiring reports.*
### Deconstructing the Compensation Package
The base salary is only one piece of a trauma surgeon's total compensation. A comprehensive package is designed to attract and retain top talent in this demanding field.
Key Components of a Trauma Surgeon's Compensation:
1. Base Salary: The guaranteed annual income, which forms the foundation of the pay package.
2. Productivity Bonuses (RVU-Based): This is a major component for many surgeons. Compensation is tied to Relative Value Units (RVUs), a measure used by Medicare to value the work involved in a physician's service. The more complex surgeries and the higher volume of patients a surgeon manages, the more RVUs they generate, leading to substantial bonuses.
3. On-Call Pay / Trauma Stipend: Many hospitals provide a per diem stipend for being on call for trauma, which can range from a few hundred to several thousand dollars per 24-hour shift, depending on the trauma center's level and volume.
4. Sign-On Bonus: To attract surgeons to a new position, hospitals often offer a significant one-time bonus, which can range from $25,000 to over $100,000.
5. Relocation Assistance: A stipend provided to cover the costs of moving to a new city for the job.
6. Student Loan Repayment: Given the immense educational debt physicians accrue, many employers, particularly in underserved areas, offer loan repayment programs, sometimes amounting to tens of thousands of dollars per year.
7. Retirement Plans: Robust retirement plans such as 401(k) or 403(b) with generous employer matching contributions are standard.
8. Continuing Medical Education (CME) Allowance: An annual stipend (typically $5,000 - $15,000) to cover costs for attending conferences, buying textbooks, and subscribing to journals to stay current in the field.
9. Malpractice Insurance: Comprehensive "claims-made" or "occurrence-based" malpractice insurance is always covered by the employer. This is a massive, non-taxable benefit, as individual policies can cost tens of thousands of dollars per year.
10. Health and Disability Insurance: Full health, dental, vision, and long-term disability insurance for the surgeon and their family.
When considering a job offer, it's essential to evaluate the entire package, as a lower base salary at an academic institution may be offset by superior benefits and retirement contributions compared to a private practice with a higher base but more personal expenses.
Key Factors That Influence Salary

A national average provides a useful benchmark, but a trauma surgeon's actual salary is a complex equation with many variables. Understanding these factors is crucial for anyone negotiating a contract or planning their career trajectory.
###
Level of Education and Board Certification
In surgery, the educational path is less a variable and more a standardized, non-negotiable requirement. There is no "shortcut" to becoming a trauma surgeon. The minimum pathway includes:
1. A four-year bachelor's degree (pre-med).
2. A four-year medical degree (M.D. or D.O.).
3. A five-to-seven-year General Surgery residency.
4. A one-to-two-year fellowship in Surgical Critical Care and/or Trauma Surgery.
The impact on salary isn't about having *more* education, as this entire 15+ year path is the baseline. Rather, the key differentiators are the board certifications obtained at the end of this training.
- American Board of Surgery (ABS) Certification: Achieving board certification in General Surgery is a prerequisite. It signals a nationally recognized standard of excellence and is required by virtually all hospitals.
- Added Qualifications in Surgical Critical Care (SCC): Earning this subspecialty certification from the ABS is the mark of a true trauma and critical care specialist. It is the single most important credential for this role and is directly tied to securing top-tier positions and salaries.
Holding these certifications is the price of entry. Lacking them would effectively exclude a physician from being hired as a trauma surgeon at any reputable trauma center, thus having an infinitely negative impact on salary potential in this specific field.
###
Years of Experience
As illustrated in the salary table above, experience is one of the most significant drivers of income growth. This is due to several factors:
- Increased Efficiency: An experienced surgeon is faster and more decisive in the operating room and more efficient at managing patient care in the ICU. This allows them to handle a higher volume of patients, directly increasing the RVUs they generate and, consequently, their bonus potential.
- Reputation and Referrals: A seasoned surgeon builds a reputation for excellent outcomes, leading to more complex case referrals and a more prominent role within the hospital and community.
- Leadership Roles: Experience is a prerequisite for leadership. The highest-paying positions, such as Trauma Medical Director or Chief of the Division of Trauma and Acute Care Surgery, are reserved for surgeons with 10+ years of proven clinical and administrative experience. These roles come with a substantial administrative stipend on top of clinical earnings, often pushing total compensation well into the $600,000 - $800,000+ range.
Salary Progression Example:
- Year 1-3: Focus is on clinical work. Salary is primarily base + call pay. (~$380,000)
- Year 5-9: Strong clinical volume, high RVU generation. Taking on mentorship or committee roles. (~$490,000)
- Year 15+: Trauma Medical Director. Mix of clinical and administrative duties. Salary is base + director stipend + productivity bonus. (~$650,000)
###
Geographic Location
Where a trauma surgeon practices has a profound impact on their salary. This is often driven by supply and demand. Major metropolitan areas on the coasts (e.g., New York City, Los Angeles, Boston) are highly desirable places to live and have a high concentration of academic medical centers, leading to a greater supply of surgeons and, consequently, slightly more competitive (i.e., lower) salaries.
Conversely, less populated states or regions in the Midwest and Southeast often struggle to recruit highly specialized surgeons. To attract talent, hospitals in these areas offer significantly higher compensation packages.
High-Paying States/Regions (based on Doximity and Medscape data):
- Wisconsin
- Indiana
- Georgia
- Texas
- Florida
- North Carolina
Lower-Paying States/Regions (often due to saturation or cost-of-living adjustments):
- Maryland
- Massachusetts
- California (though some rural areas pay well)
- New York
City-Level Variation: Even within a state, salaries can vary dramatically. A position in a rural or smaller metropolitan area will almost always pay more than a similar position in a major city center within the same state. For example, a trauma surgeon in Fresno, California, will likely earn more than one in San Francisco.
###
Employer Type & Size
The type of institution a trauma surgeon works for is a critical determinant of their compensation structure and overall earning potential.
- Academic Medical Centers: These are university-affiliated hospitals (e.g., Johns Hopkins, Mayo Clinic).
- Salary: Tend to have slightly *lower* base salaries.
- Pros: Excellent benefits, robust retirement plans, prestige, opportunities for research and teaching, and access to cutting-edge technology. The "pension-like" benefits can have significant long-term value.
- Cons: More bureaucracy, pressure to publish research ("publish or perish"), and lower pure cash compensation compared to private models.
- Hospital-Employed (Private, Non-Profit): This is the most common employment model. The surgeon is a direct employee of a private or non-profit hospital system (e.g., HCA Healthcare, Advocate Aurora Health).
- Salary: Highly variable but generally very competitive. Often features a strong base salary plus a significant productivity bonus structure.
- Pros: Stability, predictable income streams, strong benefits, and relief from the administrative burdens of running a business.
- Cons: Less autonomy compared to private practice; beholden to hospital administration and policies.
- Private Practice Group (Physician-Owned): A group of surgeons form their own business and contract with one or more hospitals to provide trauma coverage.
- Salary: Highest income potential. After an initial "buy-in" period as an employee, a surgeon can become a partner in the practice, sharing in the profits. Senior partners can be among the highest earners in the field.
- Pros: Maximum autonomy, direct control over business decisions, and unlimited income potential.
- Cons: Significant business risk, responsibility for overhead (staffing, billing, malpractice insurance), and less stability. This model is becoming less common in trauma surgery due to the high costs and logistical complexity.
- Locum Tenens ("Traveling Surgeon"): Surgeons work as independent contractors on a temporary basis to fill gaps at understaffed hospitals.
- Salary: Extremely high daily or hourly rates (e.g., $2,000 - $3,500+ per day).
- Pros: High pay, flexibility in scheduling, and the ability to travel and experience different hospital systems.
- Cons: No benefits (health insurance, retirement), no paid time off, constant travel, instability, and the need to manage your own taxes and business licenses.
###
Area of Specialization & Hybrid Roles
While "trauma surgery" is itself a specialization, a surgeon's specific role and any additional skills can further influence pay.
- Trauma/Acute Care Surgery Model: This is the modern standard. Surgeons cover not only trauma but also general surgery emergencies (e.g., appendicitis, perforated ulcers). This broader skill set makes them more valuable to a hospital and can support a higher salary.
- Combined Burn/Trauma Role: Surgeons who are also certified to manage a hospital's burn center possess a rare and valuable skill set, which can command a salary premium.
- Trauma Medical Director: As mentioned, this leadership role carries significant administrative responsibilities for quality improvement, performance reviews, and protocol management. It always comes with a substantial stipend that can add $50,000 to $150,000+ to a surgeon's annual income.
- Combined Research Roles: In academic settings, a surgeon who secures significant external research funding (e.g., from the National Institutes of Health - NIH) may have a portion of their salary "protected" by grant money, making them a major asset to the university and potentially enhancing their overall package.
###
In-Demand Skills
Beyond the standard surgical repertoire, certain advanced procedural and non-technical skills can increase a surgeon's value and earning potential.
- Advanced Endovascular and Laparoscopic Skills: Proficiency in minimally invasive techniques, such as REBOA (Resuscitative Endovascular Balloon Occlusion of the Aorta) or advanced laparoscopic repairs, places a surgeon at the forefront of modern trauma care.
- Robotic Surgery: While less common in initial trauma settings, experience with robotic platforms for elective or delayed reconstructive surgeries is becoming an increasingly valued skill.
- Administrative and Leadership Acumen: Demonstrating an ability to manage budgets, lead quality improvement initiatives, and effectively manage a team is the direct pathway to high-paying directorship roles.
- Public Health and Injury Prevention: Surgeons who engage in outreach, policy development, and community-based injury prevention programs (e.g., "Stop the Bleed") add unique value to their hospital system, which can be recognized in their career advancement and compensation.
Job Outlook and Career Growth

The demand for trauma surgeons is expected to remain strong and stable over the next decade. The U.S. Bureau of Labor Statistics (BLS) projects that employment for all physicians and surgeons will grow by 3 percent from 2022 to 2032. While this is about as fast as the average for all occupations, the specifics for a high-demand specialty like trauma surgery are more nuanced and positive.
Factors Driving Demand for Trauma Surgeons:
1. Aging Population: An older population is more susceptible to falls and other forms of trauma, leading to a sustained need for expert trauma care.
2. Consolidation of Trauma Care: There is a growing trend of concentrating trauma care into designated, high-level trauma centers. This means that while some smaller hospitals may close their trauma services, the larger, verified centers will have a constant and growing need for highly qualified surgeons.
3. Physician Burnout and Attrition: The demanding nature of trauma surgery leads to a higher rate of burnout and earlier retirement compared to some other specialties. This unfortunate reality creates a continuous cycle of job openings as experienced surgeons leave the field.
4. The Acute Care Surgery Model: The expansion of the role to include emergency general surgery has broadened the scope of practice and made trauma-trained surgeons more indispensable to hospitals, ensuring a robust job market.
### Emerging Trends and Future Challenges
The profession is not static. Aspiring and current trauma surgeons must be aware of the trends and challenges shaping the future of the field.
Key Trends:
- Advancements in Technology: The integration of AI for diagnostic imaging, robotics for reconstructive surgery, and new endovascular devices (like REBOA) will continue to evolve the technical aspects of the job. Surgeons who embrace these technologies will be at a competitive advantage.
- Focus on Outcomes and Quality Metrics: Reimbursement and hospital reputation are increasingly tied to publicly reported outcomes (e.g., mortality rates, complication rates). There is immense pressure on trauma departments to demonstrate high-quality, cost-effective care.
- Emphasis on Physician Well-being: Acknowledging the high rates of burnout and PTSD in the field, leading institutions are implementing programs focused on mental health support, more sustainable scheduling (e.g., block schedules instead of 24-hour in-house calls), and peer support networks.
Future Challenges:
- Burnout: This remains the single greatest threat to a long and healthy career in trauma surgery. The combination of sleep deprivation, high emotional stress, and administrative burdens can be overwhelming.
- Healthcare System Pressures: Navigating changes in insurance reimbursement, hospital budget cuts, and increasing documentation requirements adds a layer of non-clinical stress to the job.
- Work-Life Integration: The "always-on" nature of trauma call can make achieving a healthy work-life balance exceptionally difficult, impacting personal relationships and family life.
### How to Stay Relevant and Advance in the Field
A career in trauma surgery is one of lifelong learning and adaptation. To ensure continued growth and career advancement, surgeons should focus on:
- Continuous Learning: Actively participate in CME, attend national conferences hosted by organizations like the American College of Surgeons (ACS), the American Association for the Surgery of Trauma (AAST), and the **Eastern Association for the Surgery of Trauma (