Introduction

Imagine a career at the very heart of healthcare—a profession where you are not just a clinician, but a trusted guide, a confidant, and a constant presence in the lives of your patients. This is the reality of a family medicine doctor. It's a role that demands immense knowledge, compassion, and dedication, but in return, offers a unique opportunity to build lasting relationships and make a tangible impact on the health of a community. Beyond the profound personal rewards, it is also a financially stable and highly sought-after profession, with the average salary for a family medicine doctor reflecting their crucial role in the healthcare ecosystem, often ranging from $200,000 to over $300,000 annually.
I once spoke with a veteran family doctor in a rural community who described her role not as a job, but as being the "trusted keeper of a community's stories." She cared for three generations of the same family, from delivering babies to managing the chronic conditions of their grandparents. It's this profound human connection, coupled with a rewarding financial outlook, that draws so many dedicated individuals to this demanding yet deeply fulfilling field.
This comprehensive guide is designed to be your definitive resource, whether you're a pre-med student exploring specialties, a medical resident weighing your options, or a practicing physician considering a career change. We will delve deep into the financial realities, career opportunities, and the step-by-step journey to becoming a cornerstone of primary care.
### Table of Contents
- [What Does a Family Medicine Doctor Do?](#what-does-a-family-medicine-doctor-do)
- [Average Family Medicine Doctor Salary: A Deep Dive](#average-family-medicine-doctor-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Family Medicine Doctor Do?

A family medicine doctor, often called a family physician, is a primary care physician (PCP) who provides comprehensive, continuous healthcare for individuals and families across all ages, genders, diseases, and parts of the body. They are the quintessential generalists of the medical world, equipped with a broad base of knowledge that allows them to treat a wide spectrum of health issues. Their scope is unique in its breadth, covering pediatrics, adolescent medicine, adult medicine, and geriatrics.
Unlike specialists who focus on a specific organ or disease (like a cardiologist or an oncologist), a family physician's focus is on the patient as a whole person within the context of their family and community. They are the first point of contact for patients in the healthcare system and play a critical role in preventative care, health maintenance, and the diagnosis and treatment of acute and chronic illnesses.
Core Responsibilities and Daily Tasks:
The work of a family medicine doctor is incredibly varied. On any given day, their responsibilities may include:
- Diagnosing and Treating Acute Illnesses: Addressing common conditions like infections (strep throat, influenza, pneumonia), minor injuries, and skin rashes.
- Managing Chronic Conditions: Providing long-term care for patients with diseases such as diabetes, hypertension (high blood pressure), asthma, heart disease, and depression.
- Providing Preventative Care: Conducting routine check-ups, health-risk assessments, and cancer screenings (e.g., Pap smears, mammogram referrals).
- Administering Immunizations: Ensuring both children and adults are up-to-date on their vaccinations to prevent infectious diseases.
- Patient Counseling: Advising on lifestyle modifications, including diet, exercise, stress management, and smoking cessation.
- Coordinating Care: Acting as the central hub for a patient's health. This involves referring patients to specialists when necessary and interpreting their reports to maintain a holistic view of the patient's health.
- Performing In-Office Procedures: Depending on their training and clinic setup, this can include joint injections, skin biopsies, cryotherapy (freezing warts), IUD placement, and suturing minor lacerations.
- Maintaining Medical Records: Meticulously documenting patient encounters, diagnoses, treatments, and follow-up plans in Electronic Health Records (EHRs).
### A Day in the Life of a Family Medicine Doctor
To make this role more tangible, here is a glimpse into a typical day for a family physician working in a hospital-owned outpatient clinic:
- 7:30 AM - 8:30 AM: Arrive at the clinic. Grab a coffee and log into the EHR system. Review the day's patient schedule, check lab results and specialist reports that came in overnight, and triage any urgent patient messages.
- 8:30 AM - 12:00 PM: Morning patient appointments. The schedule is packed and diverse:
- 8:30 AM: A 6-month-old well-child check and vaccinations.
- 8:50 AM: A 45-year-old male for a follow-up on his high blood pressure medication.
- 9:10 AM: A 28-year-old female with symptoms of a urinary tract infection.
- 9:30 AM: An annual physical for a 65-year-old female, including a discussion about Medicare wellness benefits and cancer screenings.
- 10:00 AM: A 19-year-old college student struggling with anxiety.
- 10:30 AM: A 58-year-old male with type 2 diabetes, reviewing his blood sugar logs and A1c levels.
- 11:00 AM: A "squeeze-in" appointment for a 10-year-old with a persistent cough and fever.
- 12:00 PM - 1:00 PM: "Admin Hour" (often a working lunch). Catch up on charting from the morning, sign prescription refills, make referral calls to specialists, and review prior authorization requests from insurance companies.
- 1:00 PM - 4:30 PM: Afternoon patient appointments. The variety continues:
- 1:00 PM: A procedure slot for a patient needing a skin tag removed.
- 1:30 PM: A new patient visit for a 50-year-old who just moved to the area and needs to establish care.
- 2:10 PM: A 75-year-old male follow-up after a recent hospitalization for heart failure, coordinating with his cardiologist.
- 2:40 PM: A Telehealth visit with a patient to discuss recent lab results.
- 3:00 PM - 4:30 PM: More follow-ups and acute visits.
- 4:30 PM - 5:30 PM (or later): The "end" of the patient day. This hour is dedicated to finishing all clinical documentation (a crucial task), responding to non-urgent patient messages, and reviewing the schedule for the next day. This administrative work often extends well beyond the last appointment.
This schedule highlights the fast-paced, intellectually stimulating, and deeply personal nature of family medicine.
Average Family Medicine Doctor Salary: A Deep Dive
One of the most significant considerations for any aspiring physician is compensation. The path to becoming a doctor is long and expensive, so understanding the financial return on that investment is crucial. Fortunately, family medicine is a financially rewarding specialty, offering a robust salary that supports a comfortable lifestyle and allows for aggressive repayment of student loan debt.
It's important to note that salary data can vary slightly between sources due to different methodologies, sample sizes, and the components included in "total compensation." Therefore, we will synthesize data from several authoritative industry reports to provide a comprehensive and reliable picture.
### National Average Salary and Typical Range
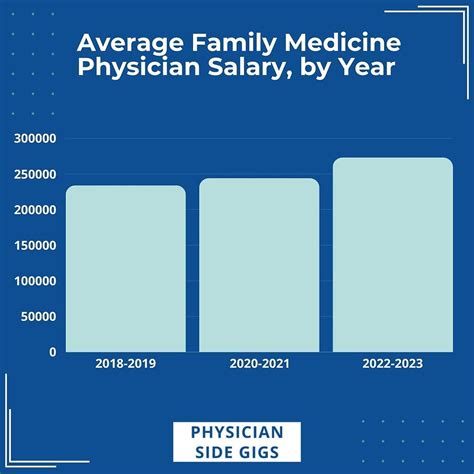
According to the most recent physician compensation reports, the average salary for a family medicine doctor in the United States typically falls between $240,000 and $275,000 per year.
- Medscape's 2023 Physician Compensation Report, a widely cited industry benchmark, reports an average annual salary for family physicians of $255,000.
- Doximity's 2023 Physician Compensation Report places the average compensation slightly higher at $273,000 for family medicine.
- The U.S. Bureau of Labor Statistics (BLS), in its May 2022 data, provides a median annual wage for "Family Medicine Physicians" of $224,460. The BLS notes that the top 10% of earners in this category made more than $239,000, though their cap on the highest wage bracket often underrepresents the top-end potential seen in other surveys.
This data paints a clear picture: a family physician can expect to earn a salary in the mid-$200,000s, but this is just an average. The full salary spectrum is wide, influenced by experience, location, and practice type. A more realistic range spans from around $180,000 for a new graduate in a lower-paying area to well over $350,000 for an experienced physician with high productivity in a lucrative market.
### Salary by Experience Level
Like any profession, compensation in family medicine grows significantly with experience. As physicians become more efficient, build a larger patient base, and potentially take on leadership responsibilities, their earning potential increases.
Here is a typical salary progression, synthesized from data from sources like Salary.com and Payscale, which provide granular experience-based data:
| Experience Level | Typical Years of Experience | Average Annual Base Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 years (Post-Residency) | $190,000 - $230,000 | Focus is on building a patient panel and gaining clinical speed. Often includes a signing bonus and may have a guaranteed salary for the first 1-2 years. |
| Mid-Career | 4-9 years | $230,000 - $275,000 | Peak clinical efficiency. Compensation often shifts to a productivity model (e.g., RVU-based). Highest period of salary growth. |
| Experienced | 10-19 years | $260,000 - $300,000+ | Established reputation and large patient base. May take on leadership roles (Medical Director) or become a partner in a private practice, boosting income. |
| Late-Career | 20+ years | $250,000 - $290,000+ | Salary may plateau or slightly decrease if the physician chooses to reduce clinical hours. Some transition to part-time, administrative, or teaching roles. |
*(Note: These figures represent base salary and do not include the significant value of bonuses and benefits.)*
### Beyond the Base Salary: Understanding Total Compensation
A physician's offer letter is much more than just a base salary. Total compensation is a package that includes performance-based incentives and valuable benefits that can add tens of thousands of dollars to the overall value.
- Production Bonuses: This is the most common form of incentive pay. Many family doctors are paid a base salary plus a bonus based on productivity, which is often measured in Work Relative Value Units (wRVUs). An wRVU is a standardized measure of the value of a physician's work, factoring in the time, skill, and intensity required for a patient visit or procedure. The more patients a doctor sees and the more complex the care, the more wRVUs they generate, leading to a larger bonus.
- Quality Bonuses: With the shift towards value-based care, health systems increasingly offer bonuses tied to quality metrics. This could include achieving certain targets for patient outcomes (e.g., A1c control in diabetic patients), patient satisfaction scores, or adherence to preventative care guidelines. These bonuses can range from $5,000 to $30,000+ annually.
- Signing Bonus: To attract talent, especially in high-demand areas, employers often offer a one-time signing bonus. For primary care physicians, this can range from $10,000 to $50,000 or more.
- Profit Sharing / Partnership Track: In private practices, physicians may be offered a partnership track. After a few years as an employee, they can "buy-in" to the practice, entitling them to a share of the profits. This offers the highest long-term earning potential but also comes with the financial risks and administrative responsibilities of business ownership.
- Comprehensive Benefits Package: The value of an employee benefits package is substantial. Key components include:
- Health, Dental, and Vision Insurance: For the physician and their family.
- Malpractice Insurance: This is a critical and expensive form of insurance that is almost always covered by the employer.
- Retirement Plans: Generous 401(k) or 403(b) plans, often with a significant employer match (e.g., 3-6% of salary).
- Paid Time Off (PTO): Typically 4-6 weeks for vacation and sick leave.
- Continuing Medical Education (CME) Stipend: An annual allowance (e.g., $3,000 - $5,000) and extra paid time off to attend conferences and maintain medical knowledge and board certification.
- Relocation Assistance: A stipend to cover moving costs for physicians relocating for a job.
- Loan Repayment Programs: Some employers, particularly in underserved areas, offer student loan repayment assistance, which can be worth tens or even hundreds of thousands of dollars over several years.
When evaluating a job offer, it is essential to look beyond the base salary and calculate the total value of the entire compensation package.
Key Factors That Influence Salary

The national average salary for a family medicine doctor provides a useful benchmark, but an individual physician's actual earnings are determined by a complex interplay of several key factors. Understanding these variables is crucial for maximizing your earning potential throughout your career. This section provides an in-depth analysis of the elements that have the most significant impact on compensation.
###
Geographic Location: The Power of Place
Where you choose to practice is arguably the single most influential factor in determining your salary. The demand for primary care physicians, the cost of living, and the concentration of healthcare systems create vast salary discrepancies between different states, cities, and even between urban and rural settings within the same state.
State-by-State and Regional Variations
Physician compensation reports consistently show that the highest salaries are often found in the Midwest and Southeast, where the demand for primary care is high, and the cost of living is often lower than on the coasts. Conversely, states in the Northeast tend to have a higher concentration of physicians and academic medical centers, which can lead to lower average salaries.
Based on an aggregation of recent data from Doximity and Medscape, here’s a representative look at high-paying and lower-paying states for family medicine:
- Top 5 Highest-Paying States (Average Annual Salary):
1. Alabama: ~$308,000
2. Kentucky: ~$305,000
3. Oklahoma: ~$300,000
4. Indiana: ~$294,000
5. Missouri: ~$290,000
- 5 Lower-Paying States (Average Annual Salary):
1. Maryland: ~$210,000
2. Massachusetts: ~$218,000
3. Rhode Island: ~$220,000
4. New York: ~$225,000
5. Connecticut: ~$230,000
The Rural vs. Urban Divide
Perhaps counterintuitively, physicians practicing in rural and underserved areas often command significantly higher salaries than their urban counterparts. This is a simple matter of supply and demand. Rural communities face chronic physician shortages, and healthcare organizations must offer aggressive compensation packages, signing bonuses, and generous loan repayment programs to attract and retain talent.
- Rural Practice: A family physician in a rural town might be offered a starting salary of $275,000, a $40,000 signing bonus, and access to the National Health Service Corps (NHSC) Loan Repayment Program, which can provide up to $50,000 in tax-free loan repayment for a two-year service commitment.
- Urban Practice: A similar physician starting in a competitive metropolitan area like Boston or San Francisco might be offered a salary closer to $210,000 with a smaller signing bonus. While the city offers more lifestyle amenities, the salary-to-cost-of-living ratio is often much less favorable.
###
Practice Setting and Employment Type
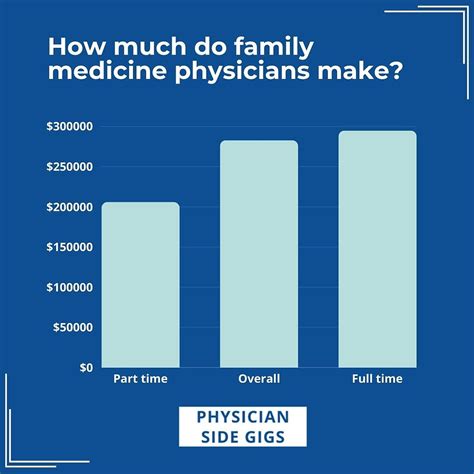
The type of organization you work for has a profound impact on your compensation structure, work-life balance, and long-term earning potential.
- Private Practice (Physician-Owned): This model offers the highest ceiling for income. As a partner or owner, you are not just an employee; you are a business owner entitled to a share of the practice's profits. After several years, top-earning partners in successful group practices can earn well over $400,000. However, this comes with significant responsibilities: managing staff, handling billing and overhead, and assuming the financial risks of the business.
- Hospital-Owned or Health System-Employed: This is now the most common employment model. Physicians are employees of a large health network. This offers stability, a predictable salary (often with wRVU-based bonuses), excellent benefits, and freedom from administrative burdens. Compensation is strong, typically aligning with the national averages discussed previously ($240,000 - $280,000), but the ceiling is generally lower than in private practice ownership.
- Academic Medical Centers: Physicians in academia split their time between clinical duties, teaching medical students and residents, and conducting research. This path is incredibly rewarding for those passionate about education and discovery. However, compensation is typically 10-20% lower than in private or hospital-owned settings, as a portion of the physician's effort is non-revenue-generating.
- Urgent Care Centers: These centers offer a different model, often with hourly pay or a salary plus productivity incentives. The work is fast-paced and focused on acute, episodic care. Experienced urgent care physicians can earn very competitive salaries, sometimes exceeding $250,000, especially if they work additional shifts.
- Direct Primary Care (DPC): An emerging model where physicians opt out of the insurance system. Patients pay a flat monthly membership fee (e.g., $75-$150) for comprehensive primary care services. This model offers incredible autonomy and a reduced administrative burden. Income is directly tied to the number of patients in the physician's panel. A successful DPC practice with a full panel of 500-600 patients can generate a very comfortable income, but it involves the entrepreneurial risk of building the business from scratch.
- Government/VA (Veterans Affairs): Working for the federal government, such as in the VA health system, offers predictable hours, excellent job security, and a robust federal benefits package. Salaries are often on a set scale and may be slightly lower than in the private sector, but the work-life balance and pension benefits are highly attractive.
###
Fellowships, Specializations, and Certifications
While family medicine is itself a specialty, physicians can pursue additional fellowship training (typically one year) to gain a Certificate of Added Qualification (CAQ) in a specific area. This can open doors to niche roles and increase earning potential.
- Sports Medicine: A popular fellowship that trains physicians in non-operative musculoskeletal care. A family doctor with a sports medicine CAQ can work in an orthopedic group or a dedicated sports medicine clinic, often earning $20,000 - $50,000 more per year than a general family physician.
- Geriatrics: With the aging population, geriatricians are in high demand. This fellowship focuses on the complex care of the elderly. While it may not always lead to a higher salary in a fee-for-service model (due to the time-intensive nature of visits), it can secure leadership positions in geriatric centers or value-based care models that reward comprehensive care.
- Obstetrics (OB): Some family physicians, particularly those planning to work in rural areas, complete an OB fellowship to gain proficiency in performing deliveries, including C-sections. This "full-scope" family medicine is highly valued and compensated accordingly due to the added skill set, call schedule, and higher malpractice insurance costs. This can add $50,000+ to their annual salary.
- Hospice and Palliative Medicine: This fellowship focuses on providing care and improving the quality of life for patients with life-limiting illnesses.
- Addiction Medicine: A rapidly growing and critically important field. A CAQ in addiction medicine can lead to roles in specialized treatment centers and a higher salary due to the high demand for experts in this area.
###
In-Demand Skills and Their Salary Impact
Beyond formal certifications, developing a specific set of clinical and professional skills can directly translate to higher compensation, primarily through increased productivity and value to an employer.
- Procedural Competency: Being skilled in a variety of in-office procedures is a significant revenue generator for a clinic. Physicians who can perform services like joint injections, vasectomies, colposcopy, skin biopsies, and IUD insertions are highly valuable and often see a direct impact on their wRVU-based bonuses.
- Leadership and Administrative Acumen: Physicians who demonstrate leadership potential can advance into roles like Clinic Medical Director or Chief Medical Officer (CMO). These roles combine clinical practice with administrative oversight and come with a significant salary increase, often pushing compensation well into the **$30