Table of Contents

- [Introduction](#introduction)
- [What Does a Cardiologist Do?](#what-does-a-cardiologist-do)
- [Average Cardiologist Salary: A Deep Dive](#average-cardiologist-salary-a-deep-dive)
- [Key Factors That Influence a Cardiologist's Salary](#key-factors-that-influence-a-cardiologists-salary)
- [Job Outlook and Career Growth for Cardiologists](#job-outlook-and-career-growth-for-cardiologists)
- [How to Become a Cardiologist: The 14+ Year Journey](#how-to-become-a-cardiologist-the-14-year-journey)
- [Conclusion: Is a Career in Cardiology Worth It?](#conclusion-is-a-career-in-cardiology-worth-it)
Introduction

Have you ever felt a profound calling to be at the forefront of life-saving medicine? Do you possess an intricate fascination with the human body's most vital organ—the heart? A career as a cardiologist is not merely a job; it is a commitment to one of the most challenging, rewarding, and critically important specialties in medicine. It's a path for those who are driven by intellectual curiosity, a desire for high-stakes problem-solving, and a deep-seated compassion for others.
This dedication comes with significant rewards, both intrinsic and financial. While the satisfaction of restoring a patient's health is immeasurable, the financial compensation is also substantial, reflecting the immense skill, extended training, and high-pressure nature of the work. The average cardiologist specialist salary in the United States is one of the highest among all professions, typically ranging from $350,000 to over $750,000 per year, with top earners in specialized fields surpassing the million-dollar mark.
I'll never forget the day my grandfather, a man who seemed invincible, was rushed to the hospital with chest pains. The calm, confident demeanor of the interventional cardiologist who explained the blocked artery and the plan to place a stent was a beacon of hope in a moment of panic. That physician didn't just fix a blood vessel; they restored our family's cornerstone, giving us many more years of memories. It was a powerful, firsthand lesson in the profound impact these specialists have on lives every single day.
This comprehensive guide is designed to be your definitive resource for understanding the complete landscape of a career in cardiology. We will move far beyond a simple salary figure, exploring the day-to-day realities of the job, the intricate factors that dictate your earning potential, the long-term career outlook, and a detailed, step-by-step roadmap to get you started on this remarkable journey. Whether you are a student mapping out your future, a medical resident considering specialties, or a professional curious about this elite field, this article will provide the expert insights you need to make an informed decision.
What Does a Cardiologist Do?
A cardiologist is a physician who specializes in the diagnosis, treatment, and prevention of diseases and conditions of the cardiovascular system, which includes the heart and blood vessels. They are the experts patients turn to for issues ranging from high blood pressure and cholesterol management to complex arrhythmias and life-threatening heart attacks. Their work is a blend of long-term patient relationship management and acute, high-pressure interventions.
A cardiologist's responsibilities are vast and varied, encompassing detective work, patient education, and highly technical procedures. They are, in essence, the master mechanics and electricians of the human body's most critical pump.
Core Responsibilities and Daily Tasks:
- Diagnosis: Cardiologists use a variety of tools to diagnose heart conditions. This includes interpreting electrocardiograms (ECGs or EKGs), conducting stress tests, analyzing echocardiograms (ultrasounds of the heart), and reading images from cardiac CT scans and MRIs.
- Patient Consultation: They spend a significant portion of their time in clinics, meeting with patients. During these consultations, they review medical histories, discuss symptoms, order and interpret tests, and develop comprehensive treatment plans.
- Treatment Planning: Treatment can range from prescribing medications (like beta-blockers, statins, or blood thinners) to recommending lifestyle changes (diet, exercise, smoking cessation) and scheduling advanced procedures.
- Performing Procedures: Depending on their sub-specialty, cardiologists perform a wide array of procedures.
- Non-invasive cardiologists focus on testing and medical management.
- Invasive, non-interventional cardiologists may perform diagnostic procedures like cardiac catheterization to visualize the heart's arteries.
- Interventional cardiologists perform procedures to open blocked arteries, such as angioplasty and stenting.
- Electrophysiologists focus on the heart's electrical system, implanting pacemakers and defibrillators and performing ablations to correct abnormal heart rhythms.
- Collaboration: Cardiologists work closely with a large team of healthcare professionals, including primary care physicians, cardiothoracic surgeons, nurses, physician assistants, and technicians.
- Continuing Education: Medicine is constantly evolving. A cardiologist must dedicate significant time to staying abreast of the latest research, guidelines, and technologies.
### A Day in the Life: Dr. Evelyn Reed, Interventional Cardiologist
To make this tangible, let's walk through a hypothetical but realistic day for an interventional cardiologist employed by a large hospital.
- 6:30 AM: Dr. Reed arrives at the hospital. Her first task is to round on her inpatients—those recovering from heart attacks, stent procedures, or severe heart failure. She reviews overnight events, lab results, and vitals with the resident physicians and nurses, adjusting medication and care plans for each of the 10-15 patients on her service.
- 8:00 AM: Morning conference. Dr. Reed joins other cardiologists and cardiothoracic surgeons to review complex cases, discussing potential candidates for surgery, transcatheter valve replacement (TAVR), or other advanced therapies.
- 9:00 AM: Cath Lab. This is the procedural part of her day. Her first case is a scheduled outpatient, a 68-year-old man with worsening chest pain. Dr. Reed performs a cardiac catheterization, identifies a 90% blockage in a major coronary artery, and successfully places a drug-eluting stent.
- 11:00 AM: Emergency Call. The emergency department (ED) pages her with a "STEMI alert"—a patient is having a major heart attack. Dr. Reed's team springs into action. The patient is rushed to the cath lab, and within 45 minutes of arriving at the hospital, Dr. Reed has opened the completely blocked artery, restoring blood flow and saving heart muscle. This "door-to-balloon" time is a critical measure of quality.
- 1:00 PM: A quick lunch while catching up on patient charts and signing orders in the electronic health record (EHR).
- 2:00 PM - 5:00 PM: Outpatient Clinic. Dr. Reed now transitions to her office role. She sees a mix of new consultations and follow-up appointments. She discusses cholesterol management with one patient, adjusts blood pressure medication for another, and explains the results of a recent stress test to a third, all while documenting her findings and communicating with their primary care doctors.
- 5:30 PM: Finishing up charting, returning calls to referring physicians, and checking in on the post-procedure patients from the morning.
- 6:30 PM: Dr. Reed heads home, but she's still on call for the hospital tonight. She knows that a phone call in the middle of the night could send her rushing back in to save another life.
This blend of scheduled work, emergency intervention, intellectual challenge, and human interaction defines the life of a cardiologist.
Average Cardiologist Salary: A Deep Dive
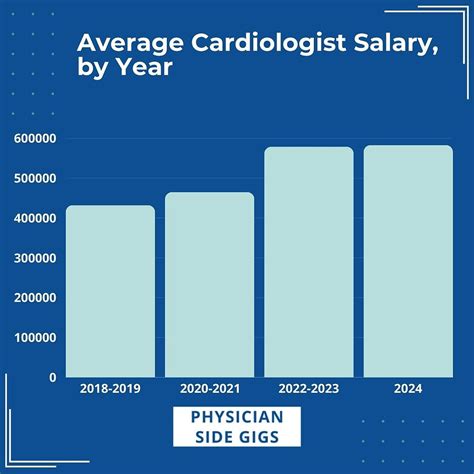
The compensation for cardiologists stands as one of the highest across all medical specialties, a direct reflection of the extensive 14+ years of education and training, the high-stakes nature of the work, and the significant revenue they generate for healthcare systems. While headlines often quote a single number, the reality of a cardiologist specialist salary is a complex package composed of base salary, productivity bonuses, and other benefits.
According to the 2023 Medscape Physician Compensation Report, one of the most authoritative sources in the industry, the average annual compensation for cardiologists is $507,000. This figure represents a combination of all cardiology sub-specialties, practice types, and experience levels.
However, a single average doesn't tell the whole story. Salary aggregators provide a more granular view of the typical salary range.
- Salary.com reports the median salary for a Cardiologist (Non-Invasive) at $459,101 as of late 2023, with a typical range falling between $372,213 and $585,076. For an Invasive Cardiologist, the median jumps to $501,404, with a range of $416,134 to $627,725.
- Doximity's 2023 Physician Compensation Report places Cardiology as the 6th highest-paid specialty, with an average annual compensation of $548,201.
It's crucial to understand that these figures are not just a base salary. A cardiologist's total compensation is often a blend of several components.
### Breakdown of a Cardiologist's Compensation Package
1. Base Salary: This is the guaranteed portion of a cardiologist's income. In a hospital-employed model, this is a fixed annual amount. In private practice, it might be a "guaranteed draw" for the first 1-2 years before a physician becomes a partner.
2. Productivity Bonuses (wRVUs): This is the most significant variable component for most cardiologists. Compensation is often tied to work Relative Value Units (wRVUs). The Centers for Medicare & Medicaid Services (CMS) assigns an RVU value to nearly every task a physician performs, from a simple office visit to a complex heart procedure. A physician's total wRVUs are multiplied by a negotiated conversion factor (e.g., $55 per wRVU) to determine their productivity-based pay. This model directly rewards cardiologists who perform more procedures or see more patients.
3. Performance & Quality Bonuses: Many health systems are moving towards value-based care. Cardiologists can earn additional bonuses for meeting specific quality metrics, such as patient satisfaction scores, adherence to treatment guidelines (e.g., prescribing appropriate medications post-heart attack), and positive patient outcomes.
4. Sign-On Bonus: To attract top talent, especially in underserved areas, hospitals and large groups offer substantial sign-on bonuses. These can range from $25,000 to over $100,000.
5. Retirement Contributions: Employers typically offer robust retirement plans, such as a 401(k) or 403(b), often with generous matching contributions.
6. Benefits Package: This includes comprehensive health, dental, and vision insurance, as well as life and disability insurance—the latter being particularly important in such a high-income profession.
7. CME & Professional Dues: Employers almost always provide an annual stipend (e.g., $5,000 - $15,000) to cover the costs of Continuing Medical Education (CME), conferences, medical licenses, and board certification fees.
8. Malpractice Insurance: Also known as professional liability insurance, this is always covered by the employer and is a significant expense, often tens of thousands of dollars per year.
9. Relocation Assistance: For physicians moving to a new city for a job, employers often provide a relocation package to cover moving expenses.
### Cardiologist Salary by Experience Level
Salary growth in cardiology is steep, especially in the first decade of practice as a physician builds their reputation, referral base, and procedural efficiency.
| Experience Level | Typical Years in Practice | Typical Annual Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years (Post-Fellowship) | $300,000 - $450,000 | Often includes a 1-2 year salary guarantee before transitioning to a productivity model. Lower end for academic or non-invasive roles. |
| Mid-Career | 3-9 Years | $450,000 - $650,000 | Physicians are at peak productivity. In private practice, this is when they may become a partner, sharing in the group's profits. |
| Senior/Experienced | 10-19 Years | $500,000 - $750,000+ | Highly efficient, established referral network. May take on leadership roles (e.g., Cath Lab Director, Chief of Cardiology). |
| Late Career | 20+ Years | $450,000 - $700,000+ | May see a slight decline if they choose to reduce call obligations or clinical hours, but earning potential remains very high. |
*Sources: Data synthesized from Medscape, Doximity, Salary.com, and industry recruitment reports.*
As this data shows, a career in cardiology offers a path to exceptionally high and sustained earning potential. However, this potential is not uniform; it is heavily influenced by a specific set of factors we will explore in the next section.
Key Factors That Influence a Cardiologist's Salary

While the national averages provide a useful benchmark, a cardiologist's actual take-home pay can vary by hundreds of thousands of dollars based on a combination of personal choices, geographic location, and market forces. Understanding these factors is crucial for any aspiring or practicing cardiologist aiming to maximize their earning potential and career satisfaction.
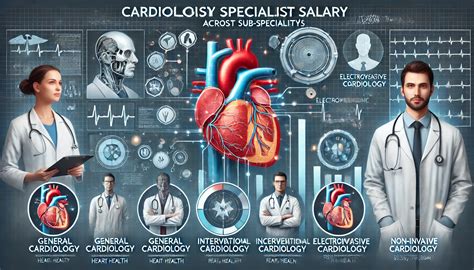
### 1. Area of Specialization within Cardiology
This is arguably the single most important factor determining a cardiologist's salary. "Cardiology" is an umbrella term, and the sub-specialties within it have vastly different compensation profiles, largely driven by the volume and complexity of procedures performed.
- Interventional Cardiology: These are the proceduralists who perform angioplasty and stenting. Because these procedures are numerous and highly reimbursed, interventional cardiologists are consistently among the highest earners. The Medscape 2023 report shows their average compensation at $575,000, with many in high-volume private practices earning well over $800,000.
- Cardiac Electrophysiology (EP): Electrophysiologists specialize in the heart's electrical system. They perform complex ablations to treat arrhythmias like atrial fibrillation and implant high-value devices like pacemakers and implantable cardioverter-defibrillators (ICDs). Their compensation is on par with, and sometimes exceeds, that of interventional cardiologists, with averages around $550,000 - $650,000.
- General/Non-Invasive Cardiology: These cardiologists focus on diagnosis, prevention, and medical management. While they perform and interpret diagnostic tests like echocardiograms and stress tests, they do not perform invasive catheter-based procedures. Their work is more clinic-based and cognitive, leading to lower (though still very high) compensation. The average salary is typically in the $400,000 to $500,000 range.
- Heart Failure & Transplant Cardiology: This is a highly specialized, cognitive-focused field dealing with the sickest patients. While their work is critically important, it is less procedure-heavy, and their compensation is similar to that of non-invasive cardiologists.
- Pediatric Cardiology: This sub-specialty focuses on congenital heart defects and cardiovascular issues in children. It is primarily based in academic medical centers and children's hospitals. Due to the nature of academic compensation and different reimbursement structures, pediatric cardiologists earn less than their adult-focused counterparts, with an average salary closer to $300,000 - $375,000, according to Salary.com and other sources.
### 2. Practice Model and Employment Type
Where a cardiologist works has a profound impact on their compensation structure and earning ceiling.
- Physician-Owned Private Practice: Historically, this was the most lucrative model. Cardiologists are partners in a business, sharing both the expenses and the profits. This model offers the highest earning potential, especially for proceduralists in a busy group, as they capture revenue from both professional fees and ancillary services (like in-office nuclear stress testing). Top-earning private practice interventional cardiologists can exceed $1,000,000 per year. However, it also comes with administrative burdens, business risks, and high overhead costs.
- Hospital or Health System Employment: This is now the most common employment model. The hospital handles all administrative tasks, overhead, and billing, providing the cardiologist with a base salary plus a productivity bonus tied to wRVUs. This model offers more stability, predictable income, and better work-life balance, but with a lower ceiling on potential earnings compared to private practice. The average salaries cited earlier ($500k-$600k) are most representative of this model.
- Academic Medical Centers: Cardiologists in academia are faculty at a university medical school. Their roles are a mix of clinical care, teaching medical students and residents, and conducting research. Compensation is almost always lower than in private or hospital-employed settings, often by 20-30%. The tradeoff is the prestige, intellectual stimulation of research and teaching, and access to cutting-edge technology. An academic cardiologist might earn $300,000 - $450,000.
- Government/VA: Cardiologists working for the Department of Veterans Affairs (VA) or other government entities are federal employees. They have a structured, transparent pay scale, excellent benefits, and a strong pension. The salary is generally lower than in the private sector, but the work-life balance is often considered the best, with minimal call and no pressure of productivity metrics like wRVUs.
### 3. Geographic Location
Compensation for physicians varies dramatically by state and region, often in ways that defy cost-of-living assumptions. Doximity's compensation report consistently shows that the highest-paying states are often in the Midwest and Southeast, where there is a greater need to attract specialists.
- Highest Paying States/Regions: States like Alabama, Kentucky, Oklahoma, and Wisconsin often report the highest average compensation for cardiologists. This is driven by supply and demand; there are fewer cardiologists per capita, and health systems must offer more competitive packages to recruit them. It's not uncommon for salaries in these regions to be 10-20% higher than the national average.
- Lowest Paying States/Regions: Conversely, states in the Northeast (like Massachusetts, Maryland) and some on the West Coast (like California) tend to have lower average salaries. These areas have a high density of physicians, numerous prestigious academic centers, and are considered highly desirable places to live, which suppresses compensation. Salaries here can be 10-15% lower than the national average.
- Rural vs. Urban: Cardiologists in rural or underserved areas often command higher salaries than their urban counterparts. A "rural premium" is common, as hospitals struggle to recruit specialists. A cardiologist might be the only one for a hundred miles, making their services incredibly valuable. They may be offered stipends for student loan repayment on top of a higher base salary.
### 4. Years of Experience and Reputation
As detailed in the previous section, experience is a powerful driver of salary growth. An early-career cardiologist is still building their speed, efficiency, and referral base. A mid-career cardiologist, with 10+ years of experience, is a well-oiled machine.
- Efficiency: An experienced interventionalist can perform a standard stenting procedure faster and more efficiently than a recent graduate, allowing them to complete more cases in a day. This directly translates to higher wRVU generation and, therefore, higher pay.
- Reputation and Referrals: A senior cardiologist with a great reputation receives a steady stream of referrals from primary care physicians and other specialists in the community. A strong referral network is the lifeblood of a busy practice and directly fuels earning potential.
- Leadership Roles: Experienced cardiologists often take on paid administrative and leadership roles, such as Chief of Cardiology, Medical Director of the Catheterization Lab, or Director of the Echocardiography Lab. These positions come with an additional stipend or salary increase, often adding $50,000 - $150,000 to their annual compensation.
### 5. In-Demand Skills and Advanced Procedural Capabilities
Cardiology is a technology-driven field. Physicians who are trained in the latest, most complex procedures can command a salary premium.
- Structural Heart Procedures: This is a rapidly growing area of interventional cardiology. Skills in procedures like Transcatheter Aortic Valve Replacement (TAVR), MitraClip for mitral regurgitation, and WATCHMAN device implantation for stroke prevention in atrial fibrillation are in extremely high demand. Cardiologists with a dedicated structural heart fellowship can often negotiate salaries at the very top end of the interventional cardiology scale.
- Complex Coronary Intervention: This includes skills in treating chronic total occlusions (CTOs)—arteries that have been 100% blocked for a long time. These are technically demanding, lengthy procedures that few cardiologists are trained to perform.
- Advanced Electrophysiology: For EPs, expertise in complex ablations for persistent atrial fibrillation or ventricular tachycardia, as well as lead extractions (removing old pacemaker/defibrillator wires), are high-value skills.
By understanding and strategically navigating these five key factors, a cardiologist can significantly influence their career trajectory and financial success.
Job Outlook and Career Growth for Cardiologists

For those considering the long and arduous path to becoming a cardiologist, the future professional landscape is a critical consideration. Fortunately, the career outlook for cardiologists is exceptionally strong and is projected to remain so for the foreseeable future, driven by powerful demographic and healthcare trends.
The U.S. Bureau of Labor Statistics (BLS) projects employment for all physicians and surgeons to grow by 3% from 2022 to 2032, which is about as fast as the average for all occupations. However, this overall figure masks the much stronger demand within specific specialties like cardiology. Several key factors contribute to a robust and growing demand for cardiovascular specialists.
1. The Aging Population: The primary driver of demand is demographics. The large Baby Boomer generation is aging into the years where cardiovascular disease is most prevalent. As this population segment grows, the incidence of heart attacks, heart failure, arrhythmias, and valvular heart disease will inevitably increase, creating a sustained need for cardiologists to manage these conditions. The Centers for Disease Control and Prevention (CDC) consistently lists heart disease as the leading cause of death in the United States, a statistic that underscores the specialty's critical importance.
2. Increasing Prevalence of Risk Factors: Modern lifestyles have led to a rising prevalence of key risk factors for heart disease, even in younger populations. Epidemics of obesity, type 2 diabetes, and hypertension are creating a larger pool of patients who require cardiovascular monitoring and care long-term, fueling the need for non-invasive and preventative cardiology services.
3. Advances in Treatment and Technology: The field of cardiology is a hotbed of innovation. New technologies and procedures are constantly being developed, which not only improve patient outcomes but also expand the scope of what cardiologists can treat.
- The Rise of Structural Heart Interventions: Procedures like TAVR have revolutionized the treatment of aortic stenosis, offering a less invasive option for older, sicker patients who were previously considered inoperable. This has created an entirely new service line for cardiology departments.
- Expansion of Electrophysiology: Advances in mapping and ablation technology have made procedures for conditions like atrial fibrillation safer and more effective, leading more patients to seek definitive treatment rather than just medical management.
- Improved Survival Rates: Paradoxically, the success of cardiology in treating acute events like heart attacks means more people are surviving and living longer with chronic heart conditions. These survivors require lifelong follow-up care from a cardiologist, further increasing demand.
4. A Looming Physician Shortage: Many analyses, including those by the Association of American Medical Colleges (AAMC), project a significant overall physician shortage in the coming decade. This shortage is expected to be particularly acute in specialties like cardiology, as a substantial portion of the current cardiologist workforce is nearing retirement age. This impending "retirement cliff" will create numerous job openings and give new cardiologists significant leverage in the job market.
### Future Challenges and How to Stay Relevant
While the outlook is bright, the profession is not without its challenges. To thrive, cardiologists must adapt to an evolving healthcare environment.
- The Shift to Value-Based Care: The traditional fee-for-service model (where payment is based on volume) is slowly giving way to a value-based model (where payment is tied to quality and outcomes). Future cardiologists will need to be adept at managing population health, focusing on prevention, and demonstrating positive patient outcomes to maximize their compensation.
- The Impact of Artificial Intelligence (AI): AI is poised to transform cardiology, particularly in diagnostics. AI algorithms are already becoming proficient at interpreting ECGs and echocardiograms, potentially faster and more accurately than humans. The cardiologist of the future will not be replaced by AI, but will instead leverage it as a powerful tool to augment their own diagnostic capabilities and streamline workflows. Staying technologically literate will be non-negotiable.
- Burnout: Cardiology is a demanding and high-stress field. The long hours, on-call responsibilities, and emotional weight of dealing with life-and-death situations contribute to high rates of physician burnout. Successful cardiologists will need to proactively seek practice environments and personal strategies that promote work-life balance and long-term career sustainability.
To advance in the field, a cardiologist can pursue several paths: sub-specialize in a high-demand area like structural heart, take on administrative leadership roles, engage in clinical research to become a thought leader, or build a thriving private practice. The key is continuous learning and adaptation to the ever-changing landscape of medicine.
How to Become a Cardiologist: The 14+ Year Journey
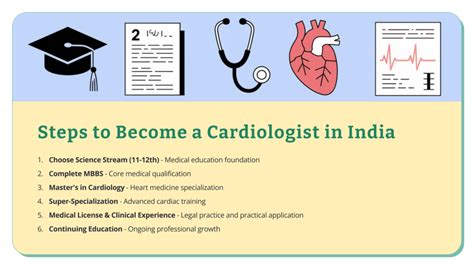
The path to becoming a board-certified cardiologist is one of the longest and most demanding in all of medicine. It requires an immense investment of time, finances, and personal sacrifice. From the first day of college to the first day as an attending cardiologist, the journey typically takes a minimum of 14 years. Here is the step-by-step guide for aspiring heart specialists.
Step 1: Bachelor's Degree (4 Years)
The journey begins with a four-year undergraduate degree from an accredited college or university. While you can major in any subject, you must complete a specific set of prerequisite courses required by medical schools. These typically include:
- One year of General Biology with lab
- One year of General Chemistry with lab
- One year of Organic Chemistry with lab
- One year of Physics with lab
- Biochemistry, English, and Mathematics (Calculus and/or Statistics)
Aspiring physicians should focus on achieving a very high Grade Point Average (GPA), especially in science courses. They should also engage in extracurricular activities that demonstrate a commitment to service and medicine, such as volunteering at a hospital, shadowing physicians