Introduction

For the driven and intellectually curious medical resident, the path to becoming a cardiologist represents the pinnacle of a demanding, yet profoundly rewarding, career in medicine. It's a journey fueled by a passion for complex physiology, a desire to perform life-saving interventions, and the promise of a professionally and financially fulfilling future. But before you become an attending cardiologist commanding a six-figure salary, you must first navigate the critical training period known as a fellowship. This raises the pivotal question for every aspiring heart specialist: What is a realistic cardiology fellow salary?
The answer is more nuanced than a single number. During this three-or-more-year period of intensive, specialized training, your compensation isn't a traditional salary but a stipend, typically ranging from $65,000 to $90,000 per year. This figure is designed to support you through a period of immense learning and growth, a final apprenticeship before you achieve full professional autonomy. I once spoke with a recently graduated interventional cardiologist who described his fellowship as "the most challenging and lowest-paid years of my professional life, but also the most transformative." He emphasized that every long night on call and every complex case was a direct investment in a future where he could confidently save a life—an investment that has since paid dividends beyond measure.
This guide is designed to be your definitive resource, moving beyond simple averages to provide a granular, in-depth analysis of every factor that shapes your earnings and career as a cardiology fellow. We will dissect the numbers, explore the influencing variables, and map out the complete journey from medical school to a successful career as a leader in cardiovascular medicine.
### Table of Contents
- [What Does a Cardiology Fellow Do?](#what-does-a-cardiology-fellow-do)
- [Average Cardiology Fellow Salary: A Deep Dive](#average-cardiology-fellow-salary-a-deep-dive)
- [Key Factors That Influence a Cardiology Fellow's Salary (Stipend)](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Cardiologists](#job-outlook-and-career-growth)
- [How to Become a Cardiologist: The Step-by-Step Path](#how-to-get-started-in-this-career)
- [Conclusion: Investing in a Life-Saving Future](#conclusion)
What Does a Cardiology Fellow Do?

A cardiology fellow is not a student, nor are they a fully independent physician. They occupy a unique and critical position in the medical hierarchy: a board-eligible internal medicine doctor undergoing advanced, supervised training to become an expert in cardiovascular diseases. The fellowship is an immersive, hands-on experience where theoretical knowledge from medical school and residency is forged into practical, life-saving skill.
The core of the role is to learn and master the diagnosis and management of a vast spectrum of heart and vascular conditions. This includes everything from common ailments like hypertension and coronary artery disease to complex issues like advanced heart failure, congenital heart defects, and life-threatening arrhythmias. A fellow's responsibilities are a blend of clinical duties, procedural training, and academic pursuits, all performed under the guidance of seasoned attending cardiologists.
Breakdown of Daily Tasks and Responsibilities:
- Inpatient Care: Fellows are often the primary point of contact for patients admitted to the cardiology service or the Cardiac Intensive Care Unit (CICU). They conduct daily rounds, develop treatment plans, manage medications, and respond to acute cardiac events.
- Consultations: They are consulted by other departments (e.g., Emergency, Surgery, Internal Medicine) to provide expert cardiovascular assessment for patients with complex medical histories.
- Outpatient Clinics: Fellows manage their own panel of patients in outpatient clinics, providing long-term care, follow-up, and preventative medicine under supervision. This is where they build lasting relationships with patients and manage chronic conditions.
- Procedural Training: A significant portion of fellowship is dedicated to learning procedures. This can include diagnostic cardiac catheterizations, interpreting echocardiograms (ultrasounds of the heart), conducting stress tests, and placing temporary pacemakers. Fellows in advanced sub-specialties will learn more complex interventions.
- Diagnostic Interpretation: They become experts in reading electrocardiograms (EKGs), ambulatory cardiac monitors, nuclear imaging scans, and cardiac CT/MRIs.
- Research and Academics: Most fellowships, particularly at academic institutions, require fellows to participate in research. This can range from clinical trials to basic science investigation, culminating in presentations at national conferences and publications in peer-reviewed journals.
- Teaching: As senior trainees, fellows are responsible for teaching and mentoring junior residents and medical students, solidifying their own knowledge in the process.
### A Day in the Life of a Cardiology Fellow (Inpatient Rotation)
To make this role more tangible, here is a representative schedule for a fellow on a busy inpatient service:
- 6:00 AM: Arrive at the hospital. Begin "pre-rounding" on the service's patients, reviewing overnight events, new lab results, and imaging studies.
- 7:30 AM: Meet with the junior residents and medical students to discuss patient updates and formulate initial plans for the day.
- 8:30 AM: "Attending Rounds." Present each patient to the supervising attending cardiologist. This is a teaching-heavy session where treatment plans are debated, refined, and finalized.
- 10:30 AM: Time for procedures. This could involve performing a diagnostic heart catheterization in the cath lab, supervising a nuclear stress test, or interpreting a new transesophageal echocardiogram (TEE) for a patient needing surgery.
- 1:00 PM: Grab a quick lunch while catching up on patient messages and following up on consult requests from other services.
- 2:00 PM: "Noon Conference." Attend a daily didactic lecture on a core cardiology topic, such as advanced lipid management or the latest guidelines for atrial fibrillation.
- 3:00 PM: Follow up on morning patients, write progress notes, call consulting services, and discuss care plans with nurses and case managers.
- 5:00 PM: Field new consults. Go see a new patient in the Emergency Department with chest pain, perform an initial assessment, and arrange for their admission to the cardiology service.
- 6:30 PM: "Sign-out." Hand over the patient list and active issues to the fellow on call for the night, ensuring a safe transition of care.
- 7:00 PM (or later): Head home, often with articles to read for the next day's cases or research to work on. If on call, the day has only just begun.
This demanding schedule underscores that a fellowship is far more than a job; it is a period of total immersion designed to forge a competent and confident cardiologist.
Average Cardiology Fellow Salary: A Deep Dive
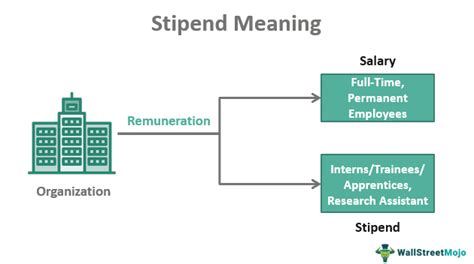
When we discuss the "salary" of a cardiology fellow, it's essential to use the correct terminology: stipend. This compensation is determined by the hospital or institution's Graduate Medical Education (GME) office and is standardized across all specialties for a given training year. The primary determinant of a fellow's stipend is their Post-Graduate Year (PGY) level.
After four years of medical school, a physician enters a 3-year Internal Medicine residency. These are PGY-1, PGY-2, and PGY-3 years. A standard Cardiology fellowship is an additional three years of training. Therefore, a first-year cardiology fellow is a PGY-4, a second-year is a PGY-5, and a third-year is a PGY-6. If a fellow pursues a further sub-specialty like Interventional Cardiology or Electrophysiology, they become a PGY-7 or even PGY-8.
The stipend increases incrementally with each PGY level to reflect the fellow's growing experience and responsibility.
### National Average Stipends and Salary Ranges
While stipends vary by institution and location, we can establish a reliable national picture by looking at authoritative sources.
According to the Medscape Resident Salary & Debt Report 2023, the average salary for all medical residents and fellows across all specialties was $67,400. However, cardiology fellows, being in their PGY-4 to PGY-6 years, earn on the higher end of this trainee spectrum.
Here is a more granular breakdown of typical cardiology fellow stipends based on PGY level, compiled from data from GME websites of major academic institutions and salary aggregators:
- First-Year Fellow (PGY-4): $72,000 - $78,000
- Second-Year Fellow (PGY-5): $75,000 - $82,000
- Third-Year Fellow (PGY-6): $78,000 - $88,000
- Sub-specialty Fellow (PGY-7+): $82,000 - $95,000+
For example, the Stanford Health Care GME office for the 2023-2024 academic year lists the following stipends, which align with these ranges:
- PGY-4: $86,303
- PGY-5: $89,321
- PGY-6: $92,234
It's clear that while this income is sufficient to live on, it is a modest figure, especially considering the level of education, debt accrued (the Association of American Medical Colleges reports the median medical school debt is over $200,000), and the grueling hours required.
### The Light at the End of the Tunnel: Fellow vs. Attending Salary
The true financial value of the fellowship is realized upon its completion. The transition from fellow to attending cardiologist marks one of the most significant salary jumps in any profession.
| Career Stage | Typical Annual Compensation | Primary Role |
| :--- | :--- | :--- |
| Third-Year Cardiology Fellow (PGY-6) | $78,000 - $88,000 | Trainee Physician |
| First-Year Attending General Cardiologist | $300,000 - $450,000+ | Independent Physician |
| Experienced Attending Cardiologist | $400,000 - $700,000+ | Partner, Specialist, Leader |
*Sources: Medscape Cardiologist Compensation Report 2023, Merritt Hawkins, AMGA Medical Group Compensation and Productivity Survey.*
The Medscape Cardiologist Compensation Report 2023 states the average annual salary for a cardiologist is $507,000. This demonstrates that the fellowship period, while financially lean, is a short-term investment for long-term, exceptional earning potential.
### Beyond the Stipend: Other Compensation and Benefits
The total compensation package for a fellow extends beyond the base stipend. GME programs compete for the best candidates by offering attractive benefits packages, which can significantly impact a fellow's financial well-being.
- Health Insurance: Comprehensive medical, dental, and vision insurance for the fellow and their family is standard.
- Disability and Life Insurance: Institutions provide crucial long-term disability and life insurance policies, protecting a fellow's future earning potential.
- Retirement Accounts: Access to 401(k) or 403(b) retirement plans, often with an institutional match. This is a critical benefit that allows fellows to start saving for retirement early.
- Professional Development Funds: An annual allowance (typically $1,500 - $3,000) to cover the cost of textbooks, medical equipment, board exam fees, and travel to national conferences like the American College of Cardiology (ACC) or American Heart Association (AHA) scientific sessions.
- Meal and Housing Stipends: Many programs, especially those in high-cost-of-living areas, provide monthly meal allowances or subsidized hospital housing to ease the financial burden.
- Paid Time Off: Typically 3-4 weeks of vacation per year, in addition to sick leave and professional leave for conferences.
- Malpractice Insurance: Full professional liability coverage is provided by the institution.
When evaluating fellowship programs, it is crucial to look at the entire benefits package, as a program with a slightly lower stipend but a generous housing allowance and retirement match might be the better financial choice.
Key Factors That Influence a Cardiology Fellow's Salary (Stipend)
While the PGY level is the primary driver of a fellow's stipend, several other factors create significant variation in compensation packages and, more importantly, influence future earning potential as an attending physician. Understanding these variables is key to making strategic career decisions.
###
Geographic Location
Location is arguably the most significant factor influencing a fellow's stipend. Hospitals in high-cost-of-living areas must offer higher stipends to attract trainees who can afford to live there. A PGY-4 stipend in New York City or San Francisco will be substantially higher than one in a smaller city in the Midwest or the South.
However, it's crucial to analyze stipend vs. cost of living. A higher salary in an expensive city may result in less disposable income than a lower salary in an affordable one.
Stipend Comparison by Geographic Location (Representative PGY-4 Stipends for 2023-2024):
| Location | Institution (Example) | Representative PGY-4 Stipend | Analysis |
| :--- | :--- | :--- | :--- |
| New York, NY | NewYork-Presbyterian (Columbia/Cornell) | ~$88,000 | High stipend, but offset by extremely high housing and living costs. |
| San Francisco, CA | UCSF | ~$93,000 (includes housing stipend) | Very high stipend with housing support, essential for the Bay Area market. |
| Houston, TX | Baylor College of Medicine | ~$72,000 | Lower stipend, but significantly lower cost of living and no state income tax. |
| Cleveland, OH | Cleveland Clinic | ~$73,500 | Competitive stipend for a city with a very affordable cost of living. |
| Durham, NC | Duke University | ~$72,000 | Moderate stipend in a region with a balanced cost of living and high quality of life. |
*Note: These are illustrative figures pulled from public GME websites and are subject to change. They demonstrate the regional variance.*
For an attending cardiologist, geography remains a powerful salary determinant. However, the trend often inverts. According to Salary.com, a cardiologist in a mid-sized, less saturated market like Milwaukee, WI, may earn a higher average salary ($477,094) than one in a highly competitive, saturated market like Boston, MA ($460,337) due to supply and demand dynamics. Rural areas often offer the highest salaries, coupled with loan repayment programs, to attract specialists.
###
Institution Type & "Company" Size
In the world of medical training, the "company type" is the nature of the sponsoring institution. This has a direct impact on the training environment, academic opportunities, and the stipend itself.
- University-Based Academic Medical Centers (e.g., Johns Hopkins, Mass General): These are the largest and most prestigious programs. They often offer stipends that are at or slightly above the regional average. Their primary draw is not money, but unparalleled research opportunities, exposure to rare pathologies, and connections to world leaders in the field. The "brand name" of a top academic fellowship can significantly boost a graduate's desirability for competitive academic jobs or top-tier private practices.
- Large Community Hospital Programs (e.g., Inova Heart and Vascular, Ochsner Medical Center): These programs often focus more on high-volume clinical training and procedural skills. Their stipends are highly competitive, sometimes even exceeding those of nearby university programs to attract top talent. They can be an excellent choice for fellows who are certain they want to enter private practice, as the training is intensely practical.
- Government/VA Hospitals: Fellowships at Department of Veterans Affairs (VA) hospitals are funded by the federal government. Their stipends are standardized and competitive. These programs offer unique insight into a specific patient population and often have a more structured work environment, but may have more administrative bureaucracy.
The size of the program (the number of fellows per year) also matters. Larger programs may offer more sub-specialty exposure and a wider network of alumni, while smaller programs can provide more one-on-one mentorship with faculty.
###
Level of Education & Path to Fellowship
While all cardiology fellows hold a doctorate (M.D. or D.O.), their educational journey and choices along the way influence their competitiveness for top fellowship programs, which in turn impacts future salary.
- M.D. vs. D.O.: Both Doctor of Medicine (M.D.) and Doctor of Osteopathic Medicine (D.O.) graduates are fully licensed physicians and can apply for cardiology fellowships. Historically, top academic programs have been dominated by M.D.s, but this is changing rapidly as the distinction becomes less important, with emphasis placed on board scores, research, and residency performance.
- Prestigious Medical School/Residency: Graduating from a top-ranked medical school or a highly respected internal medicine residency program can provide a competitive edge in the fellowship application process (known as ERAS - the Electronic Residency Application Service).
- Advanced Degrees (MD/PhD, MD/MPH): Physicians who have completed dual-degree programs, such as an M.D./Ph.D. in a relevant science or an M.D./Master of Public Health (MPH), are extremely attractive candidates for academic fellowship programs. These additional degrees position them for careers as physician-scientists or leaders in public health policy, which can lead to grant funding and high-level academic positions. While it doesn't increase the fellowship stipend, it dramatically shapes the ultimate career path and earning potential.
###
Years of Experience (The PGY System)
As detailed earlier, this is the most direct factor for stipends. The incremental raise from PGY-4 to PGY-6 is a non-negotiable, standardized increase within an institution.
- PGY-4 (First Year): Focus is on building a foundation. Rotations through the CICU, consult service, and echo lab. The learning curve is steep.
- PGY-5 (Second Year): Increased autonomy. Fellows take on more complex cases, lead the team more frequently, and begin to focus their interests toward a potential sub-specialty. They often have dedicated research time.
- PGY-6 (Third Year): Senior/Chief Fellow. This year involves significant leadership roles. The PGY-6 fellow often acts as a junior attending, making high-level decisions (with supervision), managing schedules for other fellows, and taking the lead on the most complex consults. They are preparing for independent practice.
This progression of responsibility is mirrored by the modest but meaningful increase in their stipend, acknowledging their growing value to the hospital system.
###
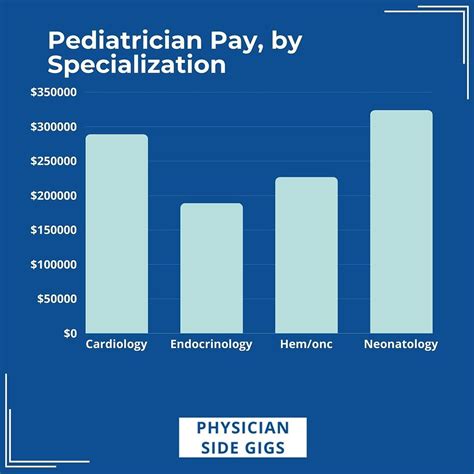
Area of Specialization (Sub-specialty Fellowships)
After completing a 3-year general cardiology fellowship, physicians can choose to specialize further. These sub-specialty fellowships are typically 1-2 additional years (PGY-7, PGY-8) and lead to the highest-paying careers in all of medicine. The stipend during this extra training will be the highest a trainee receives, but the real payoff is the attending salary.
Cardiology Sub-specialties and Their Impact on Attending Salary:
| Sub-specialty | Fellowship Duration (Post-Cardiology) | Description | Average Attending Salary |
| :--- | :--- | :--- | :--- |
| Interventional Cardiology | 1-2 years | Specializes in catheter-based treatments like angioplasty and stenting. | $600,000 - $800,000+ |
| Electrophysiology (EP) | 2 years | Manages heart rhythm disorders; performs ablations and device implantation (pacemakers, defibrillators). | $550,000 - $750,000+ |
| Advanced Heart Failure | 1 year | Manages patients with end-stage heart failure, ventricular assist devices (VADs), and heart transplants. | $450,000 - $600,000 |
| Structural Heart Disease | 1 year | Focuses on non-surgical valve repair/replacement (TAVR, MitraClip) and other structural interventions. | $600,000 - $850,000+ |
| Non-Invasive Cardiology | 0 years | Focuses on imaging (echo, nuclear, CT/MRI) and clinical/preventative care. | $400,000 - $550,000 |
*Source: Data synthesized from MedAxiom, AMGA, and Merritt Hawkins reports.*
Choosing to pursue one of these fields requires a significant time commitment, but the financial and professional rewards are immense. The procedural-based specialties like Interventional and EP command the highest incomes due to the high reimbursement rates for the procedures they perform.
###
In-Demand Skills for Fellows
While a fellow cannot negotiate their stipend based on skills, developing specific high-value skills during training makes them a more competitive candidate for the best jobs after graduation. A fellow who masters these skills will receive more lucrative job offers.
- Advanced Imaging Proficiency: Expertise in reading Cardiac MRI and Cardiac CT is becoming essential. Programs that offer strong training in these modalities produce highly sought-after graduates.
- Structural Heart Imaging: The ability to perform and interpret transesophageal echocardiography (TEE) for guiding structural interventions like TAVR is a golden ticket to a job in a high-volume structural heart program.
- Clinical Research: A strong portfolio of publications and presentations at national meetings demonstrates productivity and intellectual curiosity, which is highly valued by both academic centers and forward-thinking private practices.
- Leadership and Teaching: Serving as a Chief Fellow or being recognized for excellence in teaching residents and students signals leadership potential, a quality that is highly desirable for future partnership tracks or department leadership roles.
- Business Acumen: Understanding billing, coding, and the basics of healthcare finance can make a fellow a more attractive hire for a private practice, as it shows they can contribute to the business's bottom line.
Job Outlook and Career Growth for Cardiologists

The demand for cardiologists is robust and projected to grow significantly in the coming years. This strong outlook provides a secure foundation for anyone undertaking the long journey of a fellowship.
According to the U.S. Bureau of Labor Statistics (BLS) Occupational Outlook Handbook, the overall employment for "Physicians and Surgeons" is projected to grow by 3% from 2022 to 2032. However, this general number masks the much higher demand within specific specialties. Cardiology is poised for much faster growth due to several key demographic and public health trends.
Key Drivers of Demand for Cardiologists:
1. The Aging Population: The primary driver is the aging of the Baby Boomer generation. As this massive demographic cohort enters its 70s and 80s, the incidence and prevalence of cardiovascular diseases—including coronary artery disease, heart failure, and atrial fibrillation—are skyrocketing. This creates a sustained and growing need for cardiovascular care.
2. Increased Survival Rates: Advances in medical and interventional cardiology mean that patients are living longer *with* heart disease. A patient who survives a heart attack today requires decades of follow-up care from a cardiologist, creating a long-term demand for clinical management.
3. Prevalence of Risk Factors: Despite public health efforts, rates of obesity, type 2 diabetes, and hypertension remain stubbornly high in the United States. These are major risk factors for heart disease, ensuring a steady stream of new patients for decades to come.
4. Technological Advancement: The rapid development of new technologies, particularly in minimally invasive structural heart interventions (like TAVR) and advanced electrophysiology procedures, creates new service lines and expands the number of patients who can be treated, further fueling demand.
A 2021 report from the Association of American Medical Colleges (AAMC) projected a significant physician shortage by 2034, with a particularly acute shortfall in medical specialists like cardiologists. This supply-and-demand imbalance ensures strong job security and high compensation for graduating fellows.
### Emerging Trends and Future Challenges
The field of cardiology is not static. Fellows entering the profession today must be prepared to adapt to a changing landscape.
Emerging Trends:
- Artificial Intelligence (AI): AI is beginning to revolutionize cardiology, particularly in the interpretation of EKGs and medical imaging. Cardiologists who embrace AI as a diagnostic aid will be more efficient and effective.
- Telehealth and Remote Monitoring: The COVID-19 pandemic accelerated the adoption of virtual visits. Remote monitoring of pacemakers, defibrillators, and heart failure patients using wearable technology is becoming standard practice.
- A "Team-Based" Approach: Care is increasingly delivered by a team that includes the cardiologist, advanced practice providers (NPs/PAs), pharmacists, and nurses. Future cardiologists must be skilled leaders of these teams.
- Focus on Prevention: There is a growing emphasis on "primordial" and primary prevention—addressing risk factors before any disease develops. This includes advanced lipidology and cardiometabolic health.
Future Challenges:
- Physician Burnout: Cardiology is a high-stakes, high-stress field. The long hours, administrative burden of electronic health records, and pressures of patient outcomes contribute to high rates of burnout. Work-life balance will be an ongoing struggle and a key consideration for job seekers.
- Reimbursement Changes: Changes in how Medicare and private insurers reimburse for consultations and procedures can directly impact practice revenue and