Introduction

Imagine being the first person to guide a patient through a process that could restore their sight, the calm and knowledgeable professional who prepares them to see the world clearly again. This is the profound reality for a Certified Ophthalmic Assistant (COA). In a healthcare landscape filled with complex and demanding roles, the career of a COA stands out as a uniquely rewarding blend of technical skill, patient compassion, and critical importance. It's a profession that not only offers the deep satisfaction of helping others but also provides a stable, in-demand career with significant financial potential. For those drawn to both science and service, understanding the certified ophthalmic assistant salary and career trajectory is the first step toward a fulfilling future.
The financial landscape for a COA is promising and dynamic. Nationally, the average salary for a Certified Ophthalmic Assistant typically falls between $45,000 and $58,000 per year, but this is merely a starting point. With advanced certifications, specialized skills, and strategic career moves, top earners in the field can command salaries well over $70,000 annually.
I remember a time my grandmother was anxiously preparing for cataract surgery. It wasn't the ophthalmologist who eased her initial fears, but the ophthalmic assistant. With remarkable patience, he explained each diagnostic test, answered her barrage of questions, and treated her not as another case file, but as a person. His expertise and empathy transformed her anxiety into confidence, a small but powerful act that underscored the vital, human-centric nature of this profession.
This comprehensive guide is designed to be your definitive resource for navigating the world of a Certified Ophthalmic Assistant. We will dissect every component of a COA's salary, explore the factors that can dramatically increase your earning potential, and provide a step-by-step roadmap to launch and advance your career. Whether you are a student exploring healthcare options, a professional considering a career change, or a current COA aiming for the next level, this article will equip you with the knowledge and strategy to succeed.
### Table of Contents
- [What Does a Certified Ophthalmic Assistant Do?](#what-does-a-certified-ophthalmic-assistant-do)
- [Average Certified Ophthalmic Assistant Salary: A Deep Dive](#average-certified-ophthalmic-assistant-salary-a-deep-dive)
- [Key Factors That Influence a COA Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for COAs](#job-outlook-and-career-growth)
- [How to Become a Certified Ophthalmic Assistant](#how-to-get-started-in-this-career)
- [Conclusion: Is a Career as a COA Right for You?](#conclusion)
What Does a Certified Ophthalmic Assistant Do?

A Certified Ophthalmic Assistant is the skilled right hand of an ophthalmologist (a medical doctor specializing in eye and vision care). They are multi-talented allied health professionals who perform a wide array of clinical and administrative tasks, ensuring that patient encounters are efficient, accurate, and compassionate. A COA's work is foundational to the diagnosis and treatment of eye diseases and conditions, from simple refractive errors to complex issues like glaucoma, cataracts, and diabetic retinopathy.
Their responsibilities are diverse and require a unique combination of technical proficiency, scientific knowledge, and interpersonal skills. They are the bridge between the patient and the doctor, gathering critical data that informs the ophthalmologist's medical decisions.
Core Responsibilities and Daily Tasks:
A COA's duties can be broken down into three main categories:
1. Clinical and Patient History: This is the heart of the role.
- Patient Work-up: Taking a detailed patient history, including chief complaint, past ocular history, medical history, medications, and allergies.
- Visual Acuity Testing: Measuring and recording the patient's vision using eye charts (e.g., Snellen charts) at various distances.
- Refractometry: Performing preliminary measurements for glasses prescriptions, often using an auto-refractor and then refining with a phoropter.
- Tonometry: Measuring intraocular pressure (IOP), a critical screening test for glaucoma, using tools like the Tono-Pen, Goldmann applanation tonometer, or non-contact tonometers.
- Pupil Assessment: Evaluating pupil size, shape, and reaction to light.
- Lensometry: Measuring the power of a patient's current eyeglasses using a lensometer.
2. Diagnostic Testing and Procedures:
- Visual Field Testing: Administering tests (e.g., Humphrey Visual Field) to map a patient's peripheral vision, crucial for diagnosing and monitoring glaucoma and neurological conditions.
- Ocular Motility Testing: Assessing eye muscle alignment and coordination.
- Color Vision Testing: Screening for color blindness using Ishihara plates or similar tests.
- Keratometry: Measuring the curvature of the cornea, essential for contact lens fitting and cataract surgery calculations.
- Biometry (A-scans): Using ultrasound to measure the length of the eye to calculate the power of the intraocular lens (IOL) implant for cataract surgery.
- Optical Coherence Tomography (OCT): Operating advanced imaging equipment to create cross-sectional images of the retina, optic nerve, and cornea.
- Administering Eye Drops: Instilling dilating drops, anesthetic drops, and other topical medications as directed by the ophthalmologist.
3. Administrative and Surgical Support:
- Scribing: Accompanying the ophthalmologist during patient exams and accurately documenting findings and treatment plans in the Electronic Health Record (EHR).
- Patient Education: Explaining conditions, procedures, and post-operative care instructions to patients and their families.
- Minor Surgical Assisting: Assisting in minor in-office surgical procedures, such as chalazion removal or laser treatments.
- Instrument Maintenance: Sterilizing and maintaining ophthalmic instruments and equipment.
- Contact Lens Instruction: Teaching patients how to insert, remove, and care for contact lenses.
### A Day in the Life of a COA
To make this tangible, let's follow a COA named David through a typical day at a busy multi-specialty ophthalmology practice.
- 8:00 AM: David arrives, clocks in, and huddles with the other technicians and ophthalmologists to review the day's schedule. He sees they have a mix of post-op cataract patients, annual glaucoma checks, and several new patient consultations.
- 8:15 AM: His first patient is a 68-year-old male for a one-month post-op check on his right eye. David greets him warmly, takes his visual acuity, checks his intraocular pressure, and performs a quick auto-refraction to see what his new uncorrected vision is. He documents all findings meticulously in the EHR before handing the patient off to the doctor.
- 9:30 AM: Next is a new patient, a 45-year-old diabetic woman referred for blurry vision. This is a full work-up. David takes a comprehensive history, focusing on her diabetes control. He performs a full battery of tests: visual acuity, pupils, motility, confrontation fields, tonometry, and then instills dilating drops. While the patient dilates, he sets up the OCT machine for the retinal scan the doctor will need.
- 11:00 AM: A patient with advanced glaucoma arrives for her biannual check-up. David escorts her to the visual field testing room. He calmly explains the test, gets her positioned comfortably, and monitors her progress, offering encouragement as she clicks the button in response to the light stimuli.
- 1:00 PM: After a quick lunch, David's afternoon is focused on scribing for the practice's retina specialist. He follows the doctor from room to room, his fingers flying across the keyboard as he documents complex findings related to macular degeneration and diabetic retinopathy, ensuring every detail of the exam and treatment plan is captured accurately.
- 3:30 PM: David assists with an in-office laser procedure (a YAG capsulotomy) for a patient with a secondary cataract. He prepares the patient, sets up the laser, and provides the ophthalmologist with the necessary lenses, ensuring a smooth and sterile process.
- 4:45 PM: As the last patient leaves, David helps clean and restock the exam rooms, sterilizes instruments used during the day, and triages patient phone calls, answering questions about medications and scheduling urgent appointments. He checks his notes one last time before heading home, feeling tired but fulfilled.
This snapshot reveals that the role is far more than just "assisting." A COA is an active, essential participant in the delivery of high-quality eye care.
Average Certified Ophthalmic Assistant Salary: A Deep Dive
Understanding the financial landscape of a COA career requires looking beyond a single number. While national averages provide a useful benchmark, the true earning potential is revealed by examining the salary range, the influence of experience, and the complete compensation package. All data presented here is based on the most recent information from leading authorities like the U.S. Bureau of Labor Statistics (BLS), Salary.com, Payscale, and Glassdoor.
### National Averages and Salary Ranges
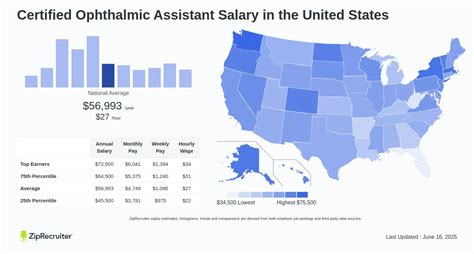
As of late 2023 and early 2024, the data points to a solid and growing salary for Certified Ophthalmic Assistants.
- The U.S. Bureau of Labor Statistics (BLS) groups Ophthalmic Assistants under the broader category of "Ophthalmic Medical Technicians." The BLS reports a median annual wage of $42,090 as of May 2022. It's crucial to note that this BLS category includes both certified and non-certified personnel, as well as those with varying levels of training, which can pull the median figure down compared to certified-only data.
- Salary.com, which provides more granular data specifically for *Certified* Ophthalmic Assistants, reports a much more representative median salary. As of November 2023, the median salary for a COA in the United States is $49,006. The typical salary range falls between $43,303 and $56,193.
- Payscale reports a similar average base salary of $47,212 per year, with a common range of $36,000 to $60,000.
- Glassdoor places the average total pay (including base and additional pay like bonuses) at $51,699 per year, with a likely range between $43,000 and $62,000.
Synthesizing this data, a realistic expectation for a newly certified or early-career COA is a starting salary in the low-to-mid $40,000s, with the national median hovering around $49,000. The most significant finding is the top end of the range. The top 10% of earners, as reported by Salary.com, can make $62,243 or more. This highlights that with experience, advanced skills, and strategic career choices, a COA can build a career with substantial earning power.
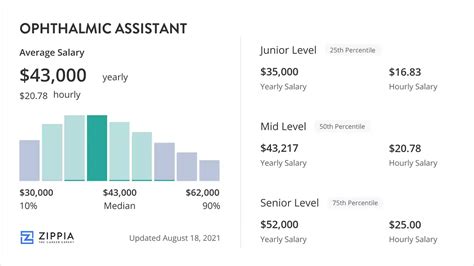
### Salary Progression by Experience Level
Experience is arguably the single most powerful driver of salary growth for a COA. As you gain hands-on skills, master new technologies, and demonstrate reliability and expertise, your value to an employer increases exponentially.
Here is a detailed breakdown of expected salary brackets based on years of experience, compiled from data from Payscale and Salary.com:
| Experience Level | Years of Experience | Typical Salary Range | Key Responsibilities & Skills at this Stage |
| :--- | :--- | :--- | :--- |
| Entry-Level COA | 0-1 Year | $38,000 - $45,000 | Mastering core competencies: patient history, visual acuity, tonometry, lensometry. Learning the practice's workflow and EHR system. Focus on accuracy and efficiency. |
| Early-Career COA | 1-4 Years | $44,000 - $52,000 | Proficient in all basic skills. Begins training on more advanced diagnostics like visual fields and OCTs. May start scribing for general ophthalmologists. Increased speed and autonomy. |
| Mid-Career COA | 5-9 Years | $49,000 - $58,000 | Mastered a wide range of diagnostic equipment. Often specializes in a sub-field (e.g., glaucoma, retina). May be a primary scribe for a specialist. Potentially trains new assistants. May pursue COT certification. |
| Experienced/Senior COA | 10-19 Years | $55,000 - $65,000+ | Expert-level technician, often holding advanced certification (COT or COMT). May act as a Lead Technician or Clinical Supervisor. Manages clinic flow, troubleshoots complex equipment, and handles the most challenging patient cases. |
| Late-Career/Expert COA | 20+ Years | $60,000 - $75,000+ | Often in a leadership role (Practice Manager, Clinical Director). Deep institutional knowledge. Involved in practice management, compliance, and staff development. Highest level of technical and administrative expertise. |
*(Note: These salary ranges are national averages and can be significantly higher in high-cost-of-living areas or specialized roles.)*
### Beyond the Base Salary: Understanding Your Full Compensation Package
Your annual salary is only one piece of the puzzle. A comprehensive compensation package can add thousands of dollars in value and significantly impact your financial well-being. When evaluating a job offer, consider these critical components:
- Bonuses: Some private practices offer annual or quarterly performance-based bonuses tied to clinic efficiency, patient volume, or practice profitability. These can range from a few hundred to several thousand dollars per year.
- Overtime Pay: As an hourly employee in most settings, COAs are eligible for overtime pay (1.5x their hourly rate) for any hours worked over 40 per week. In a busy practice, this can be a regular and substantial income boost.
- Certification & Continuing Education (CE) Stipend: Many employers recognize the value of certification and will pay for your initial exam fees and the annual CE credits required to maintain your credentials. This is a valuable, non-taxable benefit.
- Health Insurance: This is a major factor. A good employer plan with low premiums and deductibles can save you thousands per year in out-of-pocket healthcare costs compared to a high-deductible plan or purchasing insurance on the open market.
- Retirement Savings Plans: Look for employers who offer a 401(k) or 403(b) (for non-profits) plan with a matching contribution. An employer match is essentially free money. For example, a 100% match on the first 4% of your contributions means if you save 4% of your salary, your employer adds another 4%, instantly doubling your savings.
- Paid Time Off (PTO): A generous PTO policy (including vacation, sick leave, and holidays) is a crucial component of work-life balance and overall compensation.
- Profit Sharing: While less common, some private practices offer profit-sharing plans, allowing employees to receive a portion of the company's profits at the end of the year.
When comparing offers, it's essential to calculate the total value. An offer with a $48,000 salary but excellent health benefits and a 5% 401(k) match may be far superior to a $50,000 salary with a high-deductible health plan and no retirement match.
Key Factors That Influence Salary

While experience provides a predictable upward trajectory for a COA's salary, several other key factors create significant variation in earning potential. By understanding and strategically leveraging these factors, you can actively steer your career toward higher compensation. This section delves into the most impactful variables that determine how much a Certified Ophthalmic Assistant can earn.
###
Level of Certification and Education
Certification is the cornerstone of professional legitimacy and higher pay in the ophthalmic technical field. The Joint Commission on Allied Health Personnel in Ophthalmology (JCAHPO) offers a three-tiered core certification ladder, and each step up corresponds with a significant jump in responsibility and salary.
1. Certified Ophthalmic Assistant (COA®): This is the entry-level certification and the focus of this guide. It validates your competency in 19 core skill areas. Achieving this certification is the single most important step to move beyond a "trainee" or "non-certified technician" salary, often resulting in an immediate pay increase of 10-20% compared to non-certified peers.
- Average Salary: ~$49,000
2. Certified Ophthalmic Technician (COT®): This is the intermediate level of certification. The COT exam is more rigorous, requiring a deeper understanding of ophthalmic concepts and proficiency in more advanced skills like advanced tonometry, visual field analysis, and intermediate-level biometry. Technicians at this level can often work more independently.
- Estimated Salary Impact: COTs typically earn $5,000 to $10,000 more per year than COAs in the same market. Salary.com places the median salary for a COT at around $59,021.
3. Certified Ophthalmic Medical Technologist (COMT®): This is the highest level of core certification. COMTs possess an advanced, technologist-level understanding of ophthalmology. They are capable of performing all diagnostic tests, including the most complex and specialized ones (e.g., advanced electrophysiology, fundus photography interpretation). They often serve in leadership, training, and supervisory roles.
- Estimated Salary Impact: COMTs represent the top tier of technical earners. Their salaries are often $15,000 to $25,000+ higher than a COA's. The median salary for a COMT can easily exceed $70,000, with senior COMTs in high-demand areas earning well into the $80,000s.
Formal Education: While a high school diploma is the minimum educational requirement, pursuing a formal academic program can accelerate your career. Graduates of a CAAHEP (Commission on Accreditation of Allied Health Education Programs) accredited ophthalmic technology program (typically a 1-year certificate or 2-year Associate's Degree) are often preferred by top employers. They can command higher starting salaries because they enter the workforce with a strong theoretical foundation and pre-qualified clinical hours, ready to take the COA exam immediately.
###
Geographic Location
Where you work has a massive impact on your paycheck. Salaries are closely tied to the local cost of living and the regional demand for healthcare services. A COA working in a major metropolitan area with high living costs will almost always earn more than one in a rural area.
According to BLS data and salary aggregators, here are examples of high-paying and lower-paying regions for ophthalmic medical technicians:
Top-Paying States for Ophthalmic Technicians:
| State | Average Annual Salary | Why It Pays More |
| :--- | :--- | :--- |
| California | $55,000 - $65,000+ | High cost of living, large population, numerous large hospital systems and specialty practices. |
| Washington | $54,000 - $62,000+ | Strong healthcare sector, high cost of living in the Seattle metro area. |
| Alaska | $53,000 - $60,000+ | High cost of living and a need to offer competitive wages to attract skilled workers to a remote state. |
| Massachusetts | $52,000 - $60,000+ | Hub for medicine and research (Boston), high density of academic medical centers and specialty clinics. |
| New York | $51,000 - $59,000+ | Very high cost of living, particularly in the NYC metropolitan area, driving up wages across all sectors. |
Top-Paying Metropolitan Areas:
Cities like San Francisco, CA; San Jose, CA; New York, NY; Boston, MA; and Seattle, WA, will consistently offer the highest salaries, often exceeding national averages by 15-30% or more. However, it is crucial to weigh this against the dramatically higher cost of housing, transportation, and daily expenses.
States with Lower-Than-Average Salaries:
States in the Southeast and parts of the Midwest, such as Alabama, Arkansas, Mississippi, and West Virginia, typically have salaries that fall below the national average. While the dollar amount is lower, the reduced cost of living can sometimes make the real take-home pay feel comparable.
###
Work Setting (Practice Type & Size)
The type of facility you work for plays a significant role in determining your salary, benefits, and work environment.
- Private Ophthalmology Practice (Small to Medium): This is the most common employer for COAs. Salaries are generally competitive and can be flexible. In a smaller practice, you may have a wider range of responsibilities but potentially fewer opportunities for formal advancement. Bonuses and profit-sharing are more common in this setting.
- Large Multi-Specialty Ophthalmology Group: These larger practices often have a more corporate structure. Salaries may be more standardized but can be higher due to the volume of patients and specialized services offered. There are often more defined career ladders (e.g., Technician I, II, III, Lead).
- University/Academic Medical Center: These institutions often offer excellent benefits packages, including robust health insurance, generous retirement plans (like pensions or 403(b)s), and tuition assistance for further education. Base salaries might start slightly lower than in top private practices, but the total compensation package is often superior. The work environment is focused on teaching and research, offering exposure to rare cases and cutting-edge technology.
- Hospital-Based Clinics: Similar to academic centers, hospitals typically offer strong benefits and standardized pay scales. The work may be more integrated with other hospital departments. These roles are often unionized, which can lead to predictable, scheduled wage increases.
- Ophthalmic Surgery Centers: These highly specialized facilities focus on outpatient surgical procedures like cataract and LASIK surgery. The work is fast-paced and procedure-oriented. COAs with strong surgical assisting and pre/post-operative care skills can command higher salaries in this environment.
###
Area of Specialization
While a COA is a generalist, the subspecialty of the ophthalmologist(s) you support can influence your value and earning potential. Assisting in a high-volume, procedure-heavy, or technologically advanced subspecialty often correlates with higher pay because your specialized skill set is more difficult to replace.
- Retina: This is one of the highest-demand subspecialties. Retina technicians become experts in OCT imaging, fundus photography, fluorescein angiography, and assisting with intravitreal injections. This technical expertise is highly valued.
- Glaucoma: Requires mastery of various tonometry methods, advanced visual field testing, and gonioscopy setup. A deep understanding of the disease process is crucial for patient education.
- Cornea: Involves skills in corneal topography, pachymetry, and specialized contact lens fitting (e.g., for keratoconus).
- Oculoplastics: Involves assisting with in-office surgical procedures on the eyelids, orbit, and lacrimal system, requiring knowledge of sterile technique and surgical instruments.
- Pediatrics: Requires a unique skill set involving patience and creative techniques to perform accurate examinations on young children who may be uncooperative.
Developing expertise in one of these areas makes you a more valuable asset and can be a strong point of leverage during salary negotiations.
###
In-Demand Skills
Beyond core competencies, certain high-value skills can set you apart and justify a higher salary. Proactively developing these skills is a direct investment in your earning potential.
- Advanced Diagnostic Equipment Proficiency: Simply knowing how to perform an OCT is standard. Becoming a "super-user" who can troubleshoot the machine, perform advanced scan protocols, and understand the nuances of image acquisition is a high-value skill.
- Scribing: The ability to scribe accurately and efficiently is one of the most sought-after skills. It dramatically improves the doctor's efficiency, allowing them to see more patients. Expert scribes are invaluable and often compensated accordingly.
- Surgical Assisting: Formal training or experience in assisting with minor or major ophthalmic surgeries (including sterile technique) opens doors to roles in surgery centers and can command a premium salary.
- Ophthalmic Biometry/IOL Calculations: Expertise in performing precise A-scans and using tools like the IOLMaster or Lenstar for cataract surgery calculations