Introduction

Imagine being the highest level of medical authority in a chaotic, high-stakes environment outside the hospital walls. You're in the back of an ambulance, a helicopter, or a fixed-wing aircraft, managing a critically ill patient on a ventilator, titrating multiple life-saving medications, and making autonomous decisions that would typically be reserved for an ICU physician. This is the reality for a Critical Care Paramedic (CCP), an elite prehospital provider at the apex of emergency medical services. This career is not just a job; it's a calling defined by immense responsibility, unparalleled clinical skill, and the profound reward of saving lives at their most vulnerable moments.
For those with the dedication and nerve to pursue this path, the financial compensation reflects the advanced expertise required. While a standard paramedic salary provides a stable living, the critical care paramedic salary represents a significant step up, often ranging from $55,000 to over $90,000 per year, with top earners in specialized roles or high-demand locations exceeding six figures. This comprehensive guide will illuminate every facet of that salary, explore the factors that drive it, and provide you with a definitive roadmap to achieving your career and earning potential in this exceptional field.
I've spent years analyzing career trajectories in healthcare, and I once had the privilege of interviewing a flight paramedic for an industry report. He told me, "Every transport is an ICU with wings. There's no doctor to ask, no code team to call—it's just you, your partner, and your patient. The trust they place in you is absolute." That conversation solidified my understanding that the value of a CCP goes far beyond a paycheck; it's about being the ultimate safety net when one is needed most. This article is for anyone who hears that calling and wants to understand the professional and financial rewards that await.
### Table of Contents
- [What Does a Critical Care Paramedic Do?](#what-does-a-critical-care-paramedic-do)
- [Average Critical Care Paramedic Salary: A Deep Dive](#average-critical-care-paramedic-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Critical Care Paramedic Do?

A Critical Care Paramedic is not simply an experienced paramedic; they are a specialized clinician trained to manage and transport the most severely ill and injured patients between healthcare facilities. This role bridges the gap between prehospital emergency care and in-hospital intensive care. While a traditional 911 paramedic excels at stabilizing patients in the field for rapid transport to an emergency department, a CCP's primary function is to maintain or elevate a patient's level of care during transport, effectively operating a mobile Intensive Care Unit (ICU).
Their scope of practice is significantly broader and more advanced than that of a standard paramedic. They are entrusted with managing complex medical equipment and performing procedures that are otherwise confined to the hospital setting. This elevated responsibility is the cornerstone of the profession and the primary justification for the enhanced compensation structure.
### Core Responsibilities and Daily Tasks
The duties of a CCP are dictated by the patient's condition and the nature of the transport, which is typically an interfacility transfer—moving a patient from a smaller community hospital to a larger tertiary care center with specialized services.
Key responsibilities include:
- Advanced Patient Assessment: Performing comprehensive head-to-toe assessments to manage complex multi-system trauma, septic shock, acute respiratory distress syndrome (ARDS), or post-cardiac arrest care.
- Mechanical Ventilation Management: Initiating and managing mechanical ventilators, including adjusting settings for tidal volume, rate, PEEP (Positive End-Expiratory Pressure), and FiO2 (Fraction of Inspired Oxygen) based on blood gas analysis and patient response.
- Advanced Pharmacological Intervention: Administering and titrating a wide array of critical care medications, such as vasopressors (e.g., Norepinephrine, Dopamine) to manage blood pressure, sedatives (e.g., Propofol, Midazolam) for ventilated patients, and paralytics for advanced airway procedures.
- Invasive Line Monitoring: Managing and interpreting data from arterial lines for continuous blood pressure monitoring and central venous catheters for measuring central venous pressure.
- Specialized Equipment Operation: Operating advanced medical devices like intra-aortic balloon pumps (IABP), ventricular assist devices (VADs), and extracorporeal membrane oxygenation (ECMO) circuits during transport—a highly specialized and in-demand skill.
- Comprehensive Documentation: Creating detailed and meticulous patient care reports that document every assessment, intervention, and change in patient status for a seamless handover to the receiving facility's ICU team.
### A "Day in the Life" of a Critical Care Paramedic
To make this role more tangible, let's walk through a hypothetical shift for a hospital-based CCP named Alex, who works 12-hour shifts.
- 07:00: Alex arrives for her shift, receives a handover from the off-going crew, and performs a thorough check of the critical care ambulance. This isn't just counting bandages; it involves running diagnostics on the ventilator, ensuring the IV pumps are calibrated, and confirming that all critical care medications are stocked and not expired.
- 09:30: The first call comes in. A small rural hospital 90 minutes away needs to transfer a 65-year-old male patient in septic shock to Alex's tertiary care center. The patient is on a ventilator and multiple IV infusions.
- 11:00: Alex and her partner arrive at the rural hospital. They receive a detailed report from the sending physician and nurse. Alex performs her own assessment, reviews the patient's labs and imaging, and formulates a transport plan. She adjusts the ventilator settings for the long transport and ensures all IV lines are secure.
- 11:30: The transfer begins. En route, the patient's blood pressure begins to drop. Alex calmly analyzes the data from the arterial line, increases the rate of the Norepinephrine infusion according to her protocol, and communicates with her partner. The patient stabilizes.
- 13:00: They arrive at the receiving hospital's ICU. Alex provides a comprehensive, structured handover to the ICU nurse and resident, detailing the patient's history, her interventions, and the patient's response during transport.
- 14:00 - 18:00: The afternoon involves cleaning and restocking the unit, completing the extensive patient care report, and engaging in mandatory training on a new VAD protocol.
- 18:30: The second call of the day. A pediatric patient with severe respiratory distress at another community hospital needs to be brought to their children's hospital. This requires a different mindset, different equipment, and different drug calculations. The high-stress, high-skill nature of the job is on full display.
- 19:00: Alex and her partner complete the second transport and hand off their radios, concluding a mentally and emotionally demanding but professionally fulfilling day.
This example illustrates that the role is less about the "sirens and lights" of 911 and more about meticulous planning, advanced clinical decision-making, and functioning as a critical care practitioner in a mobile environment.
Average Critical Care Paramedic Salary: A Deep Dive

Understanding the financial landscape of a career is a critical component of professional planning. For Critical Care Paramedics, the salary is a reflection of their advanced training, expanded scope of practice, and the high-stakes nature of their work. It's important to distinguish this specialized role's earnings from that of a general paramedic.
The U.S. Bureau of Labor Statistics (BLS) groups all "EMTs and Paramedics" together, reporting a median annual wage of $39,410 as of May 2022. While this is a crucial benchmark for the EMS field as a whole, it does not accurately represent the earning potential of a CCP. The CCP certification and associated responsibilities place these professionals in a significantly higher compensation bracket.
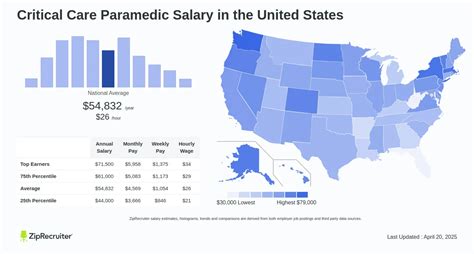
Authoritative salary aggregators that allow for more granular job title searches provide a clearer picture:
- Salary.com reports the average Critical Care Paramedic salary in the United States is $61,167 as of late 2023, with a typical range falling between $55,103 and $67,738.
- Payscale data indicates a similar average base salary of around $62,000 per year, with the total pay range (including overtime and bonuses) stretching from $48,000 to $93,000.
- Glassdoor lists an average total pay (including tips, bonuses, and overtime) for a "Critical Care Paramedic" at approximately $74,500 per year, reflecting the significant impact of supplemental pay in this field.
Taking these sources into account, a realistic national average base salary for a Critical Care Paramedic is between $60,000 and $65,000, with total compensation, after including overtime and other factors, frequently pushing into the $70,000 to $85,000 range.
### Salary by Experience Level
Like any profession, experience is a primary driver of salary growth. A paramedic who has just earned their CCP certification will earn less than a 15-year veteran with a flight background. Below is a breakdown of typical salary progression.
| Experience Level | Years in Field | Typical Annual Base Salary Range | Typical Total Compensation Range (with Overtime) | Key Characteristics |
| :--- | :--- | :--- | :--- | :--- |
| Entry-Level CCP | 0-3 Years | $52,000 - $60,000 | $60,000 - $70,000 | Recently certified; likely working in ground-based CCT. Focused on consolidating skills and gaining transport experience. |
| Mid-Career CCP | 4-9 Years | $60,000 - $70,000 | $70,000 - $85,000 | Experienced and proficient in CCT. May be working in a flight program or a high-volume service. Might take on precepting or FTO roles. |
| Senior/Veteran CCP| 10+ Years | $68,000 - $80,000+ | $85,000 - $100,000+ | A leader in the field. Often holds dual certifications (FP-C, CCP-C). May be in a management, education, or quality assurance role. Highly sought after. |
*Note: These are national averages and can vary significantly based on the factors discussed in the next section.*
### Deconstructing Total Compensation: More Than Just a Base Salary
A Critical Care Paramedic's W-2 is rarely limited to their base salary. The 24/7 nature of emergency services creates numerous opportunities for additional earnings, which can increase total annual pay by 20-40% or more. Aspiring CCPs must understand these components when evaluating a job offer.
- Overtime (OT): This is the single most significant contributor to higher earnings. EMS is notorious for staffing shortages and unpredictable call volumes, leading to frequent opportunities to work extra shifts or hold over at the end of a shift. Most services pay OT at 1.5 times the base hourly rate. A CCP earning a base of $30/hour would earn $45/hour for overtime work. Working just one extra 12-hour shift per week can add over $28,000 to one's annual income.
- Shift Differentials: To incentivize employees to work less desirable hours, many services offer a pay differential. This might be an extra $2-$5 per hour for working evenings, nights, or weekends. Over a year, this can add thousands of dollars to one's salary.
- Holiday Pay: Working on federal holidays (Thanksgiving, Christmas, etc.) often comes with premium pay, typically at 1.5x or 2x the normal hourly rate.
- Bonuses: While less common than in corporate roles, some private services and hospital systems offer performance-based bonuses, sign-on bonuses to attract talent in competitive markets, or retention bonuses for staying with the company for a set period.
- On-Call / Stand-By Pay: Flight programs, in particular, often use an on-call model. A flight paramedic might be paid a lower on-call rate (e.g., $5-$10/hour) to stay within a certain response radius of the base. When a call comes in, their pay switches to their full hourly rate, often with a guaranteed minimum number of hours paid per activation.
- Education & Certification Stipends: Many employers offer annual stipends or pay increases for maintaining required certifications or obtaining new ones. For example, a service might offer an extra $1.00/hour for holding both the FP-C and CCP-C certifications.
- Benefits Package (The Hidden Salary): The value of the benefits package cannot be overstated. A robust package is a form of compensation. When comparing offers, look at:
- Health Insurance: The quality of the plan and the percentage of the premium covered by the employer. A generous employer contribution can be worth over $10,000 per year for a family plan.
- Retirement Plans: The presence of a 401(k) or 403(b) with an employer match. A "100% match up to 6% of your salary" is essentially a 6% raise that is invested for your future.
- Paid Time Off (PTO): A generous PTO policy is essential for work-life balance and preventing burnout in this high-stress field.
- Tuition Reimbursement: An employer willing to pay for your bachelor's or master's degree is making a massive investment in your future earning potential.
When assessing the critical care paramedic salary, it is imperative to look at the total compensation package. A job with a slightly lower base salary but excellent overtime opportunities, strong differentials, and a top-tier benefits package can be far more lucrative and professionally rewarding in the long run.
Key Factors That Influence Salary

The national average salary provides a useful benchmark, but an individual's actual earnings are determined by a complex interplay of several key factors. A CCP with the right combination of experience, location, and specialization can earn double that of a colleague in a less favorable situation. Understanding these variables is crucial for maximizing your career earnings. This section, the most detailed in our guide, will break down each of these influential factors.
###
Level of Education and Certification
In the world of critical care transport, education and certification are the primary currency of value. They are direct proof of your specialized knowledge and clinical capability, and employers compensate accordingly.
- Paramedic Certification: This is the non-negotiable foundation. You cannot become a CCP without first being a certified and experienced paramedic.
- Associate's vs. Bachelor's Degree: While an associate's degree is the most common entry point for paramedics, a Bachelor of Science (BS) in Paramedicine, Emergency Health Sciences, or a related field is increasingly becoming a differentiator. A BS degree often signals a deeper understanding of research, leadership, and healthcare systems. Employers, especially hospital-based programs and those looking for future leaders, may offer a higher starting salary to candidates with a four-year degree. More importantly, a bachelor's degree is often a prerequisite for moving into management, education, or administrative roles, which carry the highest salaries in the field.
- The Critical Care Certifications (CCP-C and FP-C): This is the most significant educational factor for salary. The gold standard certifications are administered by the International Board of Specialty Certification (IBSC):
- Certified Critical Care Paramedic (CCP-C): This certification validates a paramedic's knowledge and judgment in managing critical care patients in a ground transport environment. Passing the rigorous exam demonstrates mastery of topics like ventilator management, pharmacology, and invasive monitoring. Holding a CCP-C is often a minimum requirement for a CCT job and is directly tied to the higher pay scale.
- Certified Flight Paramedic (FP-C): This is arguably the most prestigious certification in prehospital medicine. It covers all the material of the CCP-C but adds flight physiology, aviation safety, and advanced trauma care relevant to the air medical environment. Paramedics with an FP-C almost always work in flight programs, which are among the highest-paying employers in the industry. Many flight paramedics hold both certifications. Simply obtaining your FP-C can result in an immediate pay increase of 10-20% compared to a ground-based CCP role.
###
Years of Experience
Experience is a powerful determinant of salary, but its impact is tiered. The growth is not always linear but often occurs in significant jumps as you cross certain experience thresholds.
- The Foundational Years (1-3 years as a Paramedic): Before even qualifying for a CCP course, most programs require 2-3 years of experience as a paramedic in a high-volume 911 system. This period is about building a strong clinical foundation. Your salary will be that of a standard paramedic during this time.
- The Transition to CCP (0-3 years as a CCP): Once you become certified and land your first CCP job, you'll see a significant salary bump over your previous 911 paramedic role. In these early years, your focus is on mastering the CCT-specific skills. Salary growth is steady but modest as you prove your competency.
- *Example Salary Progression:* A paramedic earning $45,000 in a 911 role might jump to $58,000 upon starting their first CCP job.
- The Proficient Years (4-9 years as a CCP): This is where earning potential truly begins to accelerate. At this stage, you are a reliable, seasoned provider. You may have transitioned to a flight program, taken on field training officer (FTO) responsibilities, or become a preceptor for new CCPs. Your experience makes you a valuable asset, and your salary reflects that. You are trusted with the most complex patients and may be involved in quality improvement or protocol development.
- *Example Salary Progression:* The CCP who started at $58,000 could now be earning a base salary of $72,000, with total compensation reaching the high $80s or low $90s due to a flight role or significant overtime.
- The Veteran/Leadership Years (10+ years as a CCP): After a decade or more, CCPs are at the top of their clinical game. Many transition into formal leadership roles that leverage their extensive experience. These roles often come with higher, more stable salaries that are less reliant on overtime.
- Clinical Educator/Instructor: Teaching at a college or for an employer's education department.
- Clinical Manager/Base Manager: Overseeing daily operations, staffing, and budgeting for a transport base.
- Director of Clinical Services/Quality Assurance: A senior leadership role responsible for protocols, compliance, and clinical excellence across an entire organization.
- *Example Salary Progression:* A veteran CCP moving into a Clinical Manager role could see their base salary increase to $85,000 - $110,000+.
###
Geographic Location
Where you work is one of the most significant factors influencing your paycheck. Salary variations exist due to differences in cost of living, state and local government funding, union presence, and competition for talent.
- High-Paying States and Metropolitan Areas: States with a high cost of living, strong unions, and/or large, well-funded hospital systems tend to offer the highest salaries.
- Top 5 Highest-Paying States (for Paramedics, extrapolated for CCPs):
1. California: Major metropolitan areas like San Francisco and Los Angeles offer top-tier salaries to offset the extremely high cost of living. A CCP here could see base salaries well into the $80,000s or $90,000s.
2. Washington: Seattle's booming economy and strong public service unions contribute to high wages.
3. Hawaii: High cost of living necessitates higher pay scales.
4. Maryland: Proximity to Washington D.C. and major medical institutions like Johns Hopkins creates a competitive market for top talent.
5. Alaska: Remote locations and harsh conditions often command premium pay to attract qualified professionals.
- Lower-Paying States and Rural Areas: Conversely, states with a lower cost of living and less unionization typically have lower salary ranges.
- Example of Lower-Paying States: Southern and some Midwestern states like Mississippi, Alabama, and Arkansas tend to have lower average salaries, though the reduced cost of living can partially offset this. A CCP in a rural part of a lower-paying state might earn a salary closer to $50,000.
- Urban vs. Rural Divide: Even within a single state, there can be a vast difference between urban and rural pay. A CCP working for a major university hospital in a city will almost always earn more than one working for a small county service in a rural area. The urban roles typically involve higher acuity patients and a more competitive hiring environment, driving wages up.
###
Company Type & Size
The type of organization you work for has a profound impact on your salary, benefits, and work environment.
- Hospital-Based Programs (Often the Gold Standard): These programs, whether ground or air, are operated as a department of a hospital or health system. They typically offer the best combination of salary, benefits, and professional development. Because they are part of a larger healthcare institution, they often have better retirement plans, excellent health insurance, and access to tuition reimbursement. They are also more likely to be involved in cutting-edge medicine (like ECMO transport) and research.
- Private, For-Profit Companies: These range from large national corporations (e.g., AMR, GMR) to smaller regional services. Compensation can be highly competitive, especially for flight divisions. They may offer attractive sign-on bonuses but might have less generous benefits or retirement plans compared to hospital systems. The work environment can be very fast-paced and business-oriented.
- Municipal/Government Services (Fire Departments, Third-Services): Many fire departments operate paramedic services, and some have dedicated CCT units. These roles often come with excellent job security, strong union representation, and defined-benefit pension plans, which are rare in the private sector. The base salary might be structured differently, often with scheduled step increases, but the long-term financial security of a government pension can be immense.
- Non-Profit & University-Based Services: Similar to hospital-based programs, these employers often prioritize clinical excellence and education. A university-based flight program, for example, is a highly prestigious and competitive place to work, with salaries and benefits to match.
###
Area of Specialization
Within the CCP role itself, specialization can lead to higher pay and more opportunities.
- Flight Paramedic (Aeromedical): This is the most well-known and often highest-paid specialization. The added risks of aviation, the extreme autonomy, and the specialized knowledge of flight physiology command a premium salary. Flight paramedics (FP-C) consistently earn more than their ground-based (CCP-C) counterparts.
- Neonatal/Pediatric Critical Care Transport: Transporting critically ill infants and children is a highly specialized niche. It requires unique skills, equipment, and emotional resilience. CCPs who specialize in this area and work for dedicated pediatric transport teams are in high demand and are compensated accordingly.
- ECMO/VAD/IABP Specialist: The ability to manage highly complex cardiac support devices like ECMO (Extracorporeal Membrane Oxygenation), VADs (Ventricular Assist Devices), or IABPs (Intra-Aortic Balloon Pumps) during transport is an elite skill. Paramedics on dedicated ECMO transport teams are among the highest earners in the entire profession, often with total compensation packages exceeding $100,000. This specialization typically requires years of experience and extensive, ongoing hospital-based training.
###
In-Demand Skills
Beyond formal certifications, possessing specific, high-value clinical skills can make you a more attractive candidate and justify a higher salary.
- Advanced Ventilator Management: The ability to not just operate a ventilator, but to troubleshoot it, interpret its data, and make complex changes based on Arterial Blood Gas (ABG) results.
- Point-of-Care Ultrasound (POCUS): Using ultrasound at the bedside (or stretcher-side) to quickly assess for things like cardiac activity, fluid in the lungs, or internal bleeding is a rapidly emerging skill in prehospital medicine.
- Advanced Pharmacology Knowledge: A deep, intuitive understanding of how critical care drugs interact and how to titrate multiple infusions simultaneously to achieve a specific physiological goal.
- Bilingualism: In many parts of the country, being fluent in a second language (especially Spanish) is a highly valuable skill that can improve patient care and may come with a pay differential.
- Leadership and Precepting Skills: A demonstrated ability to teach and mentor others is highly valued. Experienced CCPs who are effective preceptors or field training officers are essential for the long-term health of any service and are often compensated for this extra responsibility.
By strategically focusing on these factors—pursuing advanced certifications, gaining experience in high-acuity systems, choosing your location and employer wisely, and developing specialized skills—you can actively steer your career towards the highest possible critical care paramedic salary.
Job Outlook and Career Growth

Choosing a career path requires not only understanding the current salary but also evaluating its long-term viability and potential for advancement. For Critical Care Paramedics, the future is bright, driven by demographic shifts, changes in the healthcare landscape, and an increasing recognition of the value of high-quality mobile critical care.
### Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) projects that employment for "EMTs and Paramedics" as a whole will grow by 5 percent from 2022 to 2032. This rate is faster than the average for all occupations. The BLS anticipates about 20,800 openings for EMTs and paramedics each year over the decade, on average, with many of those openings resulting from the need to replace workers who transfer to different occupations or exit the labor force.
While the BLS doesn't provide a separate projection for the CCP subspecialty, the growth drivers for the overall field have an amplified effect on this advanced role:
- Aging Population: As the large baby-boomer generation ages, the incidence of medical emergencies like heart attacks, strokes, and respiratory failure increases. This demographic shift directly increases the demand for all emergency medical services, but especially for the critical care transport needed to move these complex patients between facilities.
- Hospital Specialization and Consolidation: Modern healthcare is trending towards centralization. Smaller, rural, and community hospitals are often not equipped to handle highly acute or specialized cases (e.g., severe trauma, complex cardiac surgery, specialized neurological interventions). This "hub and spoke" model of healthcare necessitates a robust network of CCT teams to move patients from outlying facilities ("spokes") to comprehensive tertiary care centers ("hubs"). This is the core function of a CCP and a primary driver of job growth in the specialty.
- Increased Use of Aeromedical Services: The speed and accessibility of helicopters and fixed-wing aircraft have made them an indispensable tool in modern emergency medicine, particularly in rural areas or for time-sensitive conditions. The expansion of flight programs directly creates high-paying jobs for flight paramedics.
- Expansion of Community Paramedicine (Mobile Integrated Healthcare): While distinct from CCT, the rise of community paramedicine—where paramedics provide preventative care and manage chronic conditions in patients' homes—is raising the overall profile and scope of the paramedic profession. This push towards more advanced, out-of-hospital care creates a culture where high-level providers like CCPs are increasingly valued.
### Emerging Trends and Future Challenges
The role of the Critical Care Paramedic is not static; it is constantly evolving. Staying ahead of these trends is key to long-term career success.
Emerging Trends:
- Technology Integration: The