Introduction

In the controlled chaos of an emergency department (ED), where every second counts and decisions carry immense weight, a unique and highly skilled professional stands as a cornerstone of patient care: the Emergency Medicine Physician Assistant (EM PA). For those drawn to high-stakes, fast-paced environments and who possess a deep desire to make a tangible difference in people's lives during their most vulnerable moments, this career is not just a job—it's a calling. But beyond the profound personal fulfillment, a career as an EM PA offers remarkable financial stability and significant growth potential. The conversation around an emergency med pa salary often begins with impressive six-figure numbers, but the reality is far more nuanced and rewarding, with top earners commanding compensation well over $150,000 and even approaching $200,000 with the right combination of experience, skills, and location.
I once spoke with a seasoned EM PA who had just finished a grueling 12-hour overnight shift. Despite her exhaustion, she described her work with a quiet passion, explaining, "One minute I'm suturing a complex laceration, the next I'm coordinating a critical stroke alert. I have the autonomy to manage my own patients, but the support of an incredible team right beside me." This blend of independent practice and collaborative teamwork is the very essence of the role, making it one of the most dynamic and respected specialties for a Physician Assistant.
This comprehensive guide is designed to be your definitive resource, whether you are a student contemplating a future in medicine, a current PA considering a specialty change, or a professional seeking to maximize your earning potential. We will dissect every facet of an Emergency Medicine PA's career, from their daily responsibilities to the intricate factors that shape their salary. By the end, you will have a clear, data-driven understanding of the financial landscape and a strategic roadmap for building a successful and lucrative career on the front lines of medicine.
Table of Contents
- [What Does an Emergency Medicine PA Do?](#what-is-an-em-pa)
- [Average Emergency Medicine PA Salary: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence an Emergency Medicine PA Salary](#salary-factors)
- [Job Outlook and Career Growth for EM PAs](#job-outlook)
- [How to Become an Emergency Medicine PA](#how-to-get-started)
- [Conclusion: Is a Career as an EM PA Right for You?](#conclusion)
What Does an Emergency Medicine PA Do?

An Emergency Medicine Physician Assistant is a nationally certified and state-licensed medical professional who practices medicine on healthcare teams with physicians and other providers. Operating with a significant degree of autonomy under the supervision of an emergency medicine physician, the EM PA is a vital force in the emergency department, responsible for diagnosing and treating a vast spectrum of illnesses and injuries, from minor ailments to life-threatening conditions.
Think of the EM PA as a versatile and indispensable clinician. They are often the first provider a patient sees, tasked with quickly assessing the situation, ordering and interpreting diagnostic tests, and initiating a treatment plan. Their scope of practice is broad and demanding, requiring a comprehensive knowledge base across multiple medical disciplines, including cardiology, pulmonology, orthopedics, neurology, and more. They must be adept at thinking on their feet, multitasking effectively, and communicating clearly with patients, families, and the entire healthcare team.
Core Responsibilities and Daily Tasks:
The day-to-day work of an EM PA is anything but predictable, but a set of core responsibilities forms the foundation of their practice.
- Patient Assessment: Performing comprehensive physical examinations, taking detailed patient histories, and quickly identifying urgent medical issues.
- Diagnosis and Treatment: Developing differential diagnoses for undifferentiated patient complaints, ordering appropriate laboratory tests and imaging studies (X-rays, CT scans, ultrasounds), and creating and implementing evidence-based treatment plans.
- Performing Medical Procedures: EM PAs are trained to perform a wide array of procedures, including:
- Suturing and wound care (laceration repair)
- Incision and drainage of abscesses
- Splinting and fracture reduction
- Foreign body removal
- Joint aspirations and injections
- In some settings, advanced procedures like lumbar punctures, central line placement, and intubation.
- Prescribing Medication: Prescribing a full range of medications to treat infections, manage pain, control symptoms, and address chronic disease exacerbations.
- Patient Counseling and Education: Explaining diagnoses, treatment plans, and follow-up care instructions to patients and their families in a clear and compassionate manner.
- Collaboration and Coordination: Working seamlessly with emergency physicians, nurses, technicians, specialists, and social workers to ensure cohesive and efficient patient care from arrival to discharge or admission.
- Documentation: Meticulously documenting all aspects of patient encounters in the Electronic Health Record (EHR), ensuring accuracy for medical, legal, and billing purposes.
### A Day in the Life of an EM PA
- 7:00 AM - Sign-out: The shift begins. You arrive and receive a detailed "sign-out" from the overnight PA and physicians, getting updates on patients who are still being evaluated, awaiting test results, or pending admission to the hospital.
- 7:30 AM - First Patient: You pick up your first chart. A 45-year-old male with chest pain. You conduct a rapid but thorough history and physical, order an EKG, cardiac enzymes, and a chest X-ray, and administer initial medications while collaborating with the attending physician on the case.
- 9:00 AM - The Triage Board Lights Up: Patients begin to fill the waiting room. Over the next few hours, you see a child with a febrile seizure, a construction worker who fell from a ladder, and an elderly woman with symptoms of a urinary tract infection. You move from room to room, assessing, diagnosing, and treating.
- 11:30 AM - Procedure Time: A patient arrives with a deep 5cm laceration on their forearm from a kitchen knife slip. You expertly anesthetize the area and perform a multi-layer suture repair, providing wound care instructions upon completion.
- 1:00 PM - A Critical Moment: A "code stroke" is announced overhead. You join the team to rapidly assess a 72-year-old woman with sudden-onset facial droop and arm weakness. You help facilitate a STAT head CT and collaborate with the neurologist to determine her eligibility for thrombolytic therapy.
- 3:00 PM - Documentation and Dispositions: You find a moment to catch up on charting. You review labs and imaging results for your patients, discharging those who are stable with clear follow-up plans and coordinating with hospitalists to admit the patient with pneumonia.
- 6:30 PM - Winding Down: The pace begins to slow slightly. You see a few more patients with less acute complaints—a sprained ankle, a sore throat, a rash.
- 7:00 PM - Sign-out: The night shift PA arrives. You provide a thorough sign-out on your remaining patients, ensuring a safe and effective handoff of care before heading home after a demanding but impactful 12-hour shift.
Average Emergency Medicine PA Salary: A Deep Dive
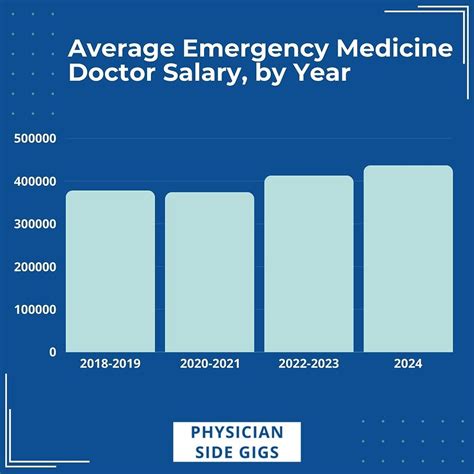
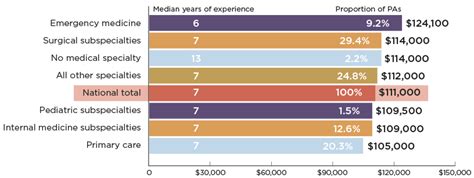
The financial compensation for the high-stakes work of an Emergency Medicine PA is substantial, reflecting the advanced training, high level of responsibility, and demanding nature of the specialty. An emergency med pa salary is consistently one of the highest among all Physician Assistant specialties, making it a financially attractive career path.
It's crucial to understand that "salary" is just one part of the total compensation package. We'll explore the national averages for base salary and then break down the additional components that contribute to an EM PA's overall earnings.
### National Average Salary and Typical Range
Data from multiple authoritative sources provides a clear picture of the earning potential for EM PAs. While figures vary slightly based on methodology and data sets, they consistently point to a strong six-figure income.
- The American Academy of Physician Associates (AAPA): The 2023 AAPA Salary Report is one of the most comprehensive resources available. It reported that the median base salary for PAs specializing in Emergency Medicine was $135,000. The median total compensation, which includes bonuses, was $143,790. This highlights the importance of looking beyond just the base salary.
- U.S. Bureau of Labor Statistics (BLS): The BLS provides data for all Physician Assistants, not just EM specialists. As of May 2022, the median annual wage for Physician Assistants was $126,010. The lowest 10 percent earned less than $87,470, and the highest 10 percent earned more than $170,790. Given that Emergency Medicine is a top-paying specialty, EM PAs can expect their earnings to fall in the upper-middle to high end of this range.
- Salary Aggregators:
- Salary.com: As of late 2023, reports the average Emergency Room Physician Assistant salary in the United States is $135,934, with a typical range falling between $124,545 and $149,438.
- Glassdoor: Reports a total pay average of around $139,000 per year, with a likely range between $121,000 and $160,000, combining base pay and additional compensation.
In summary, a newly graduated PA entering Emergency Medicine can realistically expect a starting salary in the $110,000 to $125,000 range, while experienced PAs can comfortably earn $140,000 to $160,000 or more, especially in high-paying geographic locations.
### Salary by Experience Level
Like any profession, experience is a primary driver of salary growth for an EM PA. As you gain speed, efficiency, procedural confidence, and the ability to manage more complex patients independently, your value to an employer increases significantly.
Here is a typical salary progression based on years of experience, compiled from industry data:
| Experience Level | Typical Years of Experience | Average Base Salary Range (USD) | Key Milestones & Value Proposition |
| --------------------- | --------------------------- | ------------------------------- | -------------------------------------------------------------------------------------------------------------------------------- |
| Entry-Level | 0-2 Years | $110,000 - $125,000 | Focus on foundational skills, building speed, and gaining procedural competency. High learning curve, requires more direct supervision. |
| Mid-Career | 3-9 Years | $125,000 - $145,000 | Highly efficient, autonomous with most common ED presentations. Can mentor new PAs, often manages higher patient volumes. |
| Senior / Experienced | 10+ Years | $145,000 - $165,000+ | A clinical expert, often a "Lead PA" or in an administrative role. May train residents/students, develops protocols, a key team leader. |
### Beyond the Base Salary: Understanding Total Compensation
An EM PA's base salary is only the beginning. A comprehensive compensation package often includes several other lucrative components that can add tens of thousands of dollars to your annual income. When evaluating a job offer, it's critical to look at the "total package."
- Bonuses: This is a significant part of EM PA pay.
- Performance/Productivity Bonuses: Often based on metrics like Relative Value Units (RVUs), which measure the volume and complexity of patient care provided. An efficient PA who sees more patients can earn substantial bonuses.
- Sign-On Bonuses: Commonly offered to attract talent, especially in competitive markets or underserved areas. These can range from $5,000 to $25,000 or more.
- Quality Bonuses: Tied to patient satisfaction scores (HCAHPS) or departmental quality metrics (e.g., door-to-needle time for stroke).
- Shift Differentials and Overtime: Emergency departments operate 24/7/365. Working less desirable shifts comes with financial rewards.
- Night Differential: Typically an extra $5 to $15 per hour for working overnight shifts.
- Weekend/Holiday Differential: Extra pay for working on weekends or major holidays.
- Overtime Pay: For hourly employees, any hours worked over 40 in a week are paid at 1.5 times the base rate. Salaried employees may receive a flat rate for picking up extra shifts.
- Continuing Medical Education (CME) Allowance: To maintain certification and licensure, PAs must complete 100 hours of CME every two years. Employers typically provide an annual allowance ($1,500 to $3,500 is common) and paid time off to attend conferences or complete coursework.
- Retirement Benefits: This is a cornerstone of long-term financial health. Look for employer-sponsored plans like a 401(k) or 403(b), and pay close attention to the employer match. A "100% match up to 6% of your salary" is essentially a 6% bonus that grows tax-deferred.
- Health and Wellness Benefits: Comprehensive health, dental, and vision insurance are standard. Also look for disability insurance (both short-term and long-term) and life insurance.
- Malpractice Insurance: The employer must provide professional liability insurance. It is crucial to understand the type of policy: "claims-made" vs. "occurrence." An occurrence policy is generally superior as it covers any incident that happened during your employment, regardless of when the claim is filed. If it's a claims-made policy, ensure the employer pays for "tail coverage" when you leave.
- Paid Time Off (PTO): This includes vacation, sick leave, and personal days. The amount of PTO generally increases with years of service.
- Other Perks: Some employers may offer loan repayment assistance, relocation packages, or stipends for professional licenses and association dues.
Key Factors That Influence an Emergency Medicine PA Salary
While we've established a strong baseline for the emergency med pa salary, actual earnings can vary dramatically based on a combination of professional and environmental factors. Understanding these variables is the key to maximizing your income potential throughout your career. This section provides an exhaustive breakdown of what truly drives compensation in this field.
### 1. Level of Education & Advanced Certification
For Physician Assistants, the standard entry-level degree is a Master's from an ARC-PA accredited program. While having a doctorate (DMSc) may offer an edge in academia or administration, it doesn't typically translate to a direct, significant increase in clinical pay in the emergency department.
The most impactful credential for an EM PA beyond initial certification is the Certificate of Added Qualifications (CAQ) in Emergency Medicine.
- What is the EM CAQ? Offered by the National Commission on Certification of Physician Assistants (NCCPA), the CAQ is a voluntary credential that demonstrates advanced knowledge and experience in the specialty. It signifies a PA has gone above and beyond the standard for practice.
- Requirements: To earn the CAQ, a PA must have at least 1,500 hours of experience in an emergency department, a physician attestation of their competency, a specialty CME requirement, and must pass a rigorous specialty exam.
- Impact on Salary: Earning the EM CAQ is a powerful negotiating tool. It signals to employers a high level of expertise and dedication, which can translate into a higher base salary, access to more competitive jobs, and eligibility for leadership positions. While exact figures vary, PAs with a CAQ can often command a salary that is 5-10% higher than their non-certified peers. According to the 2023 AAPA report, PAs holding at least one CAQ had a median total compensation of $150,000, significantly higher than the overall median.
### 2. Years of Experience
As detailed in the previous section, experience is arguably the most significant driver of salary growth in the first decade of practice. The salary trajectory is not linear but follows a curve that reflects the development of clinical expertise.
- Years 0-2 (The Learning Phase): New graduates are an investment for an ED group. They are building efficiency, learning departmental flow, and require more supervision. Their compensation reflects this learning curve. The primary focus here is skill acquisition, not salary maximization.
- Years 3-9 (The Efficiency Phase): This is where PAs hit their stride. They can manage high patient volumes, handle complex cases with greater autonomy, and require minimal supervision. Their productivity (often measured in RVUs) is high, directly contributing to the department's bottom line. This is the period of the most rapid salary growth.
- Years 10+ (The Expertise/Leadership Phase): At this stage, salary growth in a purely clinical role may begin to plateau. However, new avenues for increased compensation open up. Senior PAs become mentors, preceptors for PA students, and may take on administrative duties as a "Lead PA" or "Advanced Practice Provider (APP) Director." These leadership roles come with significant salary bumps and stipends, pushing experienced PAs into the highest earning brackets.
### 3. Geographic Location
Where you choose to practice has a monumental impact on your salary. This variation is driven by a combination of local demand for providers, the cost of living, and state-level regulations regarding PA scope of practice.
Highest-Paying States for Physician Assistants:
According to the BLS (May 2022 data for all PAs), the top-paying states are often on the West Coast, where high demand and cost of living drive up wages.
1. Washington: Annual Mean Wage: $145,390
2. California: Annual Mean Wage: $144,520
3. Alaska: Annual Mean Wage: $144,460
4. Hawaii: Annual Mean Wage: $142,310
5. Nevada: Annual Mean Wage: $141,360
Highest-Paying Metropolitan Areas:
City-level data often reveals even higher salaries in specific urban centers.
1. San Jose-Sunnyvale-Santa Clara, CA: $166,930
2. Salinas, CA: $163,890
3. Santa Rosa, CA: $161,280
4. San Francisco-Oakland-Hayward, CA: $159,810
5. Yakima, WA: $159,100
The Rural vs. Urban Factor:
The dynamic between rural and urban salaries is complex. While major metropolitan areas often boast the highest *absolute* salaries, this is frequently offset by a much higher cost of living. Conversely, rural or underserved areas may offer surprisingly competitive salaries, significant sign-on bonuses, and even loan repayment programs (like the National Health Service Corps) to attract desperately needed providers. A $135,000 salary in rural Iowa provides a vastly different quality of life than a $150,000 salary in San Francisco.
### 4. Practice Setting & Employer Type
The type of institution you work for directly influences your compensation structure, benefits, and work environment.
- Academic Medical Centers/University Hospitals: These institutions are often at the forefront of research and medical education.
- Salary: Base salaries may be slightly lower than in the private sector.
- Pros: Excellent benefits packages (pension plans, generous PTO), opportunities for teaching and research, and the prestige of working at a top-tier institution. The work often involves a higher acuity patient population.
- Large Private Hospital Systems (Community Hospitals): This is the most common employment setting for EM PAs. These systems are often run by large national or regional corporations (like HCA, Tenet, AdventHealth) or non-profit health systems.
- Salary: Highly competitive and often driven by productivity metrics (RVUs). This is where many of the highest clinical salaries can be earned.
- Pros: Often feature structured onboarding, clear paths for advancement, and robust compensation packages with significant bonus potential.
- Private, Physician-Owned Democratic Groups: In this model, a smaller group of physicians (and sometimes PAs) contracts with a hospital to staff the ED.
- Salary: Can be extremely lucrative. In addition to a competitive salary and bonus structure, there may be opportunities for profit-sharing or a partnership track after several years of service.
- Pros: More autonomy, a smaller and potentially more collegial group dynamic, and a direct share in the financial success of the group.
- Government (VA Hospitals, Military, Indian Health Service):
- Salary: Governed by the federal General Schedule (GS) pay scale, which is transparent and predictable. While the ceiling may be lower than in the private sector, the starting salaries are competitive.
- Pros: Unmatched job security, an incredible federal benefits package (pension, excellent health insurance, generous leave), and often a better work-life balance with less emphasis on productivity metrics.
- Urgent Care Centers: While related, Urgent Care is a distinct environment from the ED.
- Salary: Typically 10-15% lower than in an emergency department. The work involves lower acuity patients, and the procedural opportunities are less extensive.
- Pros: More predictable hours and a less stressful environment, which can be a major draw for some PAs seeking better work-life balance.
### 5. In-Demand Skills (Hard and Soft)
In the high-pressure environment of the ED, certain skills make a PA exceptionally valuable, which can be leveraged for higher pay.
Critical Hard Skills:
- **Point-of-Care
