The piercing wail of an ambulance siren, the controlled chaos of a trauma bay, the quiet, reassuring voice cutting through a patient's fear—this is the world of the Emergency Medicine Physician. It's a career defined by high stakes, immense pressure, and the profound ability to make a difference at life's most critical junctures. For those drawn to this intense and rewarding field, the question of compensation is not just a practical consideration but a reflection of the extensive training, specialized skills, and immense responsibility the role entails. While the motivation is rarely just about money, understanding the financial landscape of an er doc salary is a crucial step in planning for this demanding career. The earning potential is substantial, with national averages often exceeding $350,000 annually, but this figure is just the beginning of a much more complex story.
As a career analyst who has spent years dissecting professional trajectories, I once spoke with a seasoned ER physician who shared a poignant insight. "You don't get paid for the 99 routine cases," she told me, "you get paid for your ability to handle the one catastrophic case that walks through the door at 3 AM without a moment's notice. You're paid for your readiness." This sentiment perfectly encapsulates the value placed on this profession. It's a career that demands you be at your best when others are at their worst, and the compensation structure reflects that unique burden and privilege.
This comprehensive guide will illuminate every facet of an Emergency Room (ER) doctor's salary, career path, and future outlook. We will dissect national data, explore the myriad factors that influence your paycheck, and provide a clear, step-by-step roadmap for aspiring physicians.
### Table of Contents
- [What Does an ER Doctor Do?](#what-er-doc-do)
- [Average ER Doc Salary: A Deep Dive](#average-salary)
- [Key Factors That Influence an ER Doc's Salary](#key-factors)
- [Job Outlook and Career Growth in Emergency Medicine](#job-outlook)
- [How to Become an ER Doctor: A Step-by-Step Guide](#how-to-become)
- [Conclusion: Is a Career in Emergency Medicine Right for You?](#conclusion)
What Does an ER Doctor Do?

An Emergency Medicine Physician, commonly known as an ER doctor, is a medical specialist on the front lines of healthcare. They are experts in diagnosing and treating a vast spectrum of acute illnesses and injuries, many of which can be life-threatening. Unlike other specialists who may focus on a single organ system, an ER doctor must be a master of rapid assessment and stabilization for patients of all ages, from newborns to the elderly, with any conceivable condition. Their workplace—the Emergency Department—is a dynamic, unpredictable, and often high-stress environment that operates 24/7.
The core responsibility of an ER doctor is to provide immediate medical care to undifferentiated patients. This involves a rapid-fire process of evaluation, diagnosis, intervention, and disposition. They are the ultimate medical multitaskers, often simultaneously managing a patient in cardiac arrest, a child with a broken arm, and an elderly person suffering from a stroke.
Core Roles and Responsibilities Include:
- Triage and Assessment: Working with nurses to quickly assess the severity of a patient's condition to prioritize care for the most critical cases.
- Diagnosis: Employing a combination of physical examinations, patient history, and diagnostic tests (like X-rays, CT scans, ultrasounds, and lab work) to arrive at a provisional or definitive diagnosis under extreme time pressure.
- Stabilization: Performing immediate, life-saving interventions. This can include anything from administering medications to stop a seizure, performing CPR, inserting a breathing tube (intubation), or controlling severe bleeding.
- Performing Procedures: Executing a wide range of medical procedures, such as suturing complex lacerations, setting broken bones, draining abscesses, inserting central venous catheters, and performing lumbar punctures.
- Treatment and Management: Prescribing medications, managing pain, and initiating treatment for acute conditions like heart attacks, strokes, sepsis, and severe infections.
- Disposition Planning: Making the critical decision about a patient's next step in their care journey. This can be admitting them to the hospital for further treatment, discharging them with follow-up instructions, or transferring them to a specialized facility.
- Communication and Collaboration: Effectively communicating with patients and their families, often during times of intense emotional distress. They also work in constant collaboration with nurses, physician assistants, specialists, surgeons, and other hospital staff.
---
### A Day in the Life of an ER Doctor
To make this tangible, let's walk through a hypothetical shift for Dr. Anya Sharma, an attending physician in a busy urban hospital.
- 6:45 AM: Dr. Sharma arrives for her 7:00 AM shift, grabbing a quick coffee. She changes into her scrubs and prepares for "sign-out," the critical handoff from the overnight physician.
- 7:00 AM: The night-shift doctor provides a rapid, detailed overview of the current patients in the department: a patient with chest pain awaiting cardiology, a trauma patient stabilizing in the bay, several patients in the waiting room, and lab results pending for others.
- 7:30 AM: Her first new patient is a 65-year-old male with sudden, severe abdominal pain. Dr. Sharma quickly assesses him, orders bloodwork and a CT scan, suspects a possible aortic aneurysm, and gets the vascular surgery team on alert.
- 9:00 AM: While awaiting the scan results, she moves to the next room to see a 5-year-old with a high fever and cough. She reassures the anxious parents, performs a thorough exam, and orders a flu and RSV swab.
- 10:15 AM: A "Code Blue" is called overhead. A patient has gone into cardiac arrest. Dr. Sharma leads the resuscitation team, calling for medications, performing chest compressions, and ultimately using a defibrillator to restore a normal heart rhythm. The patient is stabilized and moved to the Intensive Care Unit (ICU).
- 11:30 AM: She returns to her desk to rapidly document the code, review incoming lab results, and check on her abdominal pain patient. The CT scan confirms a leaking aneurysm; the patient is rushed to the operating room.
- 1:00 PM: She finally has a moment to eat a protein bar while simultaneously reviewing an X-ray of a teenager's wrist—a clear fracture. She heads to the patient's room to perform a reduction (setting the bone) and apply a splint.
- 2:30 PM: The afternoon brings a steady stream of cases: a patient with a severe allergic reaction, a person experiencing a psychiatric crisis, and a complex laceration from a kitchen accident that requires meticulous suturing.
- 4:45 PM: Dr. Sharma begins preparing her own sign-out for the incoming evening physician, ensuring all critical information, pending tests, and follow-up plans are clearly communicated.
- 5:15 PM: After a grueling 10-hour shift, she leaves the hospital, mentally replaying the critical cases and knowing she made a direct impact on more than a dozen lives.
This snapshot illustrates the incredible breadth of knowledge, technical skill, and emotional resilience required. It's this unique combination of capabilities that commands the substantial salary associated with the profession.
Average ER Doc Salary: A Deep Dive
The compensation for an Emergency Medicine Physician is among the highest in the medical field, a direct reflection of the grueling training, high-stress environment, and critical nature of the work. However, the term "average salary" can be misleading, as actual earnings are influenced by a multitude of factors. Let's break down the numbers from authoritative sources to paint a clear and accurate picture.
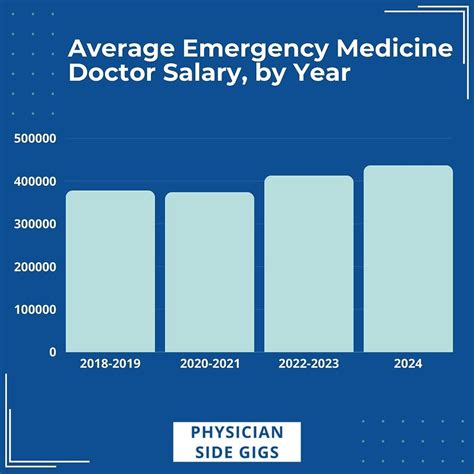
According to the Medscape Physician Compensation Report 2023, one of the most respected annual surveys in the industry, the average annual salary for an Emergency Medicine Physician is $373,000. This places them squarely in the middle to upper-middle tier of all physician specialties.
Other reputable sources provide a similar range, though methodologies can differ:
- Salary.com reports a median ER doctor salary of $335,463 as of late 2023, with a typical range falling between $283,780 and $398,730.
- Doximity's 2023 Physician Compensation Report places the average annual compensation for Emergency Medicine even higher, at $385,000.
- Payscale.com, which often includes a wider range of experience levels and practice types, shows an average base salary around $299,700, with a total pay range (including bonuses) extending from $123k to over $420k.
The consensus from these top-tier sources is clear: a typical, full-time ER doctor in the United States can expect to earn somewhere in the $330,000 to $390,000 range.
### Salary by Experience Level
Like any profession, experience is a primary driver of salary growth. An ER doctor's value increases as they become more efficient, more skilled in complex procedures, and more adept at managing patient flow, all of which can translate to higher productivity and compensation.
Here is a breakdown of the typical salary progression for an Emergency Medicine Physician:
| Career Stage | Years of Experience | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level (Post-Residency) | 0-2 Years | $250,000 - $320,000 | Recently completed residency. Focused on building speed, confidence, and clinical acumen. May work more nights/weekends. |
| Mid-Career | 3-9 Years | $320,000 - $390,000 | Highly proficient and efficient. Comfortable with a wide range of critical procedures and complex cases. Often the workhorses of the department. |
| Senior/Experienced | 10-19 Years | $370,000 - $450,000+ | Peak earning years. May take on leadership roles (Medical Director, Department Chair), which come with additional stipends. High level of efficiency. |
| Late Career | 20+ Years | $350,000 - $430,000+ | Salary may plateau or slightly decrease as some physicians choose to reduce hours or step back from high-intensity roles. Deep expertise is highly valued. |
*Sources: Data synthesized from Salary.com, Payscale, and Medscape industry analysis.*
It's important to note that the jump from residency to attending physician is the most significant financial leap in a doctor's life. A final-year resident may earn between $65,000 and $75,000, so their first attending salary represents a 400-500% increase in income overnight.
### Beyond the Base Salary: Understanding Total Compensation
An ER doctor's base salary is only one piece of the puzzle. Total compensation is a much more comprehensive measure of their earnings and benefits, which are often substantial.
Key Components of an ER Doctor's Compensation Package:
1. Base Salary vs. Hourly Rate: Many ER doctors, especially those working for physician groups or hospital systems, are paid an hourly rate. A typical full-time schedule is often between 120 and 144 hours per month (e.g., twelve 12-hour shifts).
- Example: An hourly rate of $200 x 130 hours/month x 12 months = $312,000 base salary.
- Rates can range from $150/hour in lower-paying academic settings to over $300/hour for experienced physicians in high-demand rural areas or through *locum tenens* (temporary) agencies.
2. Productivity Bonuses (RVUs): This is a huge component of many compensation models. RVU stands for "Relative Value Unit," a measure used by Medicare to value the work involved in a physician's service. Doctors are often paid a base salary and then earn a bonus for every RVU they generate above a certain threshold. This directly rewards physicians who are more efficient and see more complex (higher RVU-generating) patients. This can add $20,000 to $100,000+ to their annual income.
3. Quality Bonuses: As healthcare shifts towards value-based care, hospitals are increasingly tying bonuses to quality metrics. This can include patient satisfaction scores, door-to-doctor time, and adherence to clinical protocols (e.g., sepsis or stroke care). These bonuses are typically smaller, perhaps $5,000 to $25,000 annually.
4. Profit Sharing & Partnership: Physicians working for private, democratic physician groups often have the opportunity for partnership after a few years. As a partner, they share in the profits of the group, which can significantly boost their total compensation. This is often where the highest earning potential lies.
5. Sign-On Bonuses and Relocation Assistance: To attract talent, especially in less desirable or underserved areas, hospitals and groups offer significant sign-on bonuses, which can range from $20,000 to $75,000 or more. They also often cover the costs of moving.
6. Comprehensive Benefits: The value of an ER doctor's benefits package is substantial and should be considered part of their total compensation. This almost always includes:
- Health, Dental, and Vision Insurance: For the physician and their family.
- Malpractice Insurance: This is a critical and expensive benefit. "Occurrence-based" policies are generally superior to "claims-made" policies with a "tail" coverage requirement.
- Retirement Savings Plans: Such as a 401(k) or 403(b), often with a generous employer match.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $3,000 - $5,000) to pay for conferences, courses, and materials needed to maintain their license and skills.
- Paid Time Off (PTO): While often calculated in hours rather than days, it's a key part of the package.
- Disability and Life Insurance: Protecting their high income is crucial.
When evaluating a job offer, it is essential to look beyond the headline salary and analyze the entire compensation structure, as these additional components can add tens of thousands of dollars in value each year.
Key Factors That Influence an ER Doc's Salary

The $373,000 average salary is a useful benchmark, but an individual ER doctor's earnings can swing dramatically based on a combination of personal and professional variables. This section provides an exhaustive breakdown of the factors that have the biggest impact on the bottom line. Understanding these levers is critical for maximizing earning potential throughout one's career.
---
### 1. Geographic Location
Where you practice is arguably the single most significant factor determining your salary. The supply and demand for ER physicians vary immensely across the country, creating large pay disparities that do not always align with the cost of living.
- High-Paying States and Regions: Often, the highest salaries are found not in the major coastal hubs, but in the Midwest, Southeast, and rural areas where recruiting physicians is more challenging. States known for high ER physician compensation include:
- Wisconsin
- Indiana
- North Carolina
- Alabama
- Florida
- Texas
- Arizona
According to Doximity's report, metro areas like Charlotte, NC ($433k), and San Antonio, TX ($421k) offer some of the highest average salaries. The principle is simple: less desirable locations must offer higher compensation to attract top talent.
- Lower-Paying States and Regions: Conversely, areas with a high density of medical schools, residency programs, and desirable amenities tend to have a greater supply of physicians, which drives down salaries. These often include:
- Maryland
- Massachusetts
- Colorado
- The Northeast corridor (e.g., Boston, New York City, Washington D.C.)
While the salaries in these areas are still very high by any standard (often over $300,000), they are lower relative to the national average and come with a much higher cost of living. For example, the BLS notes that physician salaries in the D.C. area are often lower than in less populated regions.
- Rural vs. Urban: The rural/urban divide is a powerful force. A physician in a rural, critical-access hospital in Wyoming might earn $450,000 or more due to extreme demand, while a physician in a prestigious academic center in downtown Chicago might earn $310,000. The rural physician has fewer local amenities but a much lower cost of living, leading to immense wealth-building potential.
---
### 2. Practice Model and Employer Type
The type of organization you work for has a profound impact on your pay structure, autonomy, and overall earning potential.
- Private Democratic Physician Groups: Historically, this has been the most lucrative model. In these groups, physicians are the owners. After a 1-3 year partnership track, they become partners and share directly in the group's profits. This model provides high autonomy and the highest ceiling for earnings, often exceeding $450,000 - $500,000 for senior partners in successful groups. However, it also comes with administrative responsibilities and business risk.
- Hospital/Health System Employee: This is the most rapidly growing model of employment. The physician is a direct employee of the hospital or a large corporate health system.
- Pros: High stability, predictable salary, excellent benefits, no administrative burden, and often a better work-life balance.
- Cons: Lower top-end earning potential (generally capped under $400,000), less autonomy, and more corporate bureaucracy. This model is ideal for those who want to "just practice medicine" without the headaches of running a business.
- Academic Medical Centers: Physicians at university hospitals are typically paid the least. Their compensation might range from $280,000 to $340,000. The lower salary is offset by other benefits: the prestige of working at a major academic institution, involvement in teaching residents and medical students, and opportunities for research. The work environment is often more intellectually stimulating, but patient volume and acuity can be extremely high.
- *Locum Tenens* (Temporary Work): This involves working as an independent contractor on a temporary basis to fill staffing gaps. *Locum tenens* physicians command the highest hourly rates, often $250 - $400+ per hour. This translates to massive earning potential for those willing to work full-time.
- Pros: Unmatched flexibility, high hourly pay, and the ability to travel and experience different practice environments.
- Cons: No benefits (health insurance, retirement, disability must be self-funded), job instability, constant travel, and the challenges of adapting to new hospital systems and EMRs.
---
### 3. Years of Experience and Reputation
As detailed in the previous section, salary grows with experience. This isn't just about longevity; it's about the development of skills that directly impact revenue and departmental efficiency.
- Efficiency and Throughput: An experienced physician can see, diagnose, treat, and disposition patients more quickly and safely than a new graduate. In a productivity-based (RVU) model, this directly translates to higher pay. A doctor who can comfortably manage 2.5 patients per hour will earn significantly more than one who manages 1.8.
- Procedural Competence: Senior physicians are often the go-to experts for difficult procedures like complex airway management or central line placement, which are valued highly.
- Leadership Roles: Experienced physicians often advance into leadership positions that come with additional compensation (a "stipend").
- Medical Director / Department Chair: This role involves administrative oversight, quality control, scheduling, and representing the department. It can add $50,000 to $150,000+ to a physician's annual income.
- Ultrasound Director, Stroke Coordinator, etc.: Leading specific programs within the department can also come with smaller stipends.
---
### 4. Sub-Specialization and Fellowships
While Emergency Medicine is itself a specialty, physicians can pursue further training via fellowships (typically 1-2 years) to become sub-specialists. This doesn't always lead to a higher salary within the ER, but it opens up different career paths and can increase marketability.
- Pediatric Emergency Medicine (PEM): A 2-3 year fellowship. PEM physicians can work in dedicated children's hospital ERs. According to Medscape, their average salary is often slightly higher than general EM.
- Critical Care Medicine: This 2-year fellowship allows a physician to become dual board-certified in EM and Critical Care. They can split their time between the ER and the ICU. Critical Care physicians (Intensivists) have a higher average salary (Medscape reports $406,000), so this path can increase overall earnings.
- Toxicology: Experts in poisonings and overdoses. This often leads to a hybrid career of clinical shifts and work with a poison control center or in a consulting role.
- Ultrasound: This is a highly valuable fellowship. An Ultrasound Director can improve department billing, quality, and resident education, making them a highly sought-after and well-compensated leader.
- EMS (Emergency Medical Services): This fellowship leads to roles as medical directors for ambulance services, fire departments, or event medicine, providing a different career avenue.
While a fellowship means delayed entry into peak earning years, the unique skills acquired can provide long-term career stability and open doors to leadership and niche roles.
---
### 5. In-Demand Skills and Certifications
Beyond the standard board certification (ABEM or AOBEM), certain skills can enhance a physician's value.
- Advanced Procedural Skills: Mastery of ultrasound-guided procedures (nerve blocks, difficult IV access), advanced airway techniques, and other complex interventions makes a physician more valuable, especially in high-acuity centers.
- Administrative and Business Acumen: Understanding billing, coding, and hospital finances is crucial for those in private groups or leadership roles. This knowledge directly impacts the financial health of the group and, therefore, individual partner pay.
- Tech Proficiency: In the age of Electronic Medical Records (EMRs), being a fast and efficient charter is a superpower. It allows a physician to see more patients and reduce time spent on administrative tasks, which is critical for both RVU-based pay and personal well-being.
- Communication and "Soft Skills": Excellent bedside manner and communication skills improve patient satisfaction scores. As these scores become increasingly tied to hospital reimbursement and physician bonuses, these "soft skills" have a tangible financial impact.
Job Outlook and Career Growth in Emergency Medicine

For anyone considering the decade-long journey to become an ER doctor, understanding the long
