For the aspiring physician, the moment the words "Congratulations, you have matched!" appear on the screen is a life-altering culmination of a decade of relentless effort. It signifies the transition from student to doctor, the beginning of a new, intense chapter: residency. If you are on this path, aiming for a career in Internal Medicine—the backbone of adult medical care—one of the most pressing, practical questions you face is about compensation. What is an internal medicine residency salary, and what does it truly mean for your finances and lifestyle during these demanding training years?
This guide is designed to be your definitive resource. We will move beyond simple numbers to provide a comprehensive analysis of a resident's stipend, the factors that shape it, and the long-term financial trajectory of an internist. The average internal medicine resident in the United States earns a stipend between $60,000 and $75,000 per year, a figure that often surprises those outside the medical field given the immense responsibility and grueling hours. I once had a conversation with a PGY-2 (second-year) resident in a hospital cafeteria at 3 AM; despite her exhaustion, she spoke with immense passion about diagnosing a complex autoimmune disease. She also spoke candidly about her student loan statements, which were a constant, looming presence. Her story encapsulates the reality of residency: a period of profound professional growth, personal sacrifice, and careful financial navigation.
This article will equip you with the knowledge to understand your worth, plan your finances, and look ahead to the rewarding career that awaits.
### Table of Contents
- [What Does an Internal Medicine Resident Do?](#what-does-an-internal-medicine-resident-do)
- [Average Internal Medicine Residency Salary: A Deep Dive](#average-internal-medicine-residency-salary-a-deep-dive)
- [Key Factors That Influence a Resident's Salary](#key-factors-that-influence-a-residents-salary)
- [Job Outlook and Career Growth for Internists](#job-outlook-and-career-growth-for-internists)
- [How to Become an Internal Medicine Resident](#how-to-become-an-internal-medicine-resident)
- [Conclusion: Is the Journey Worth the Reward?](#conclusion-is-the-journey-worth-the-reward)
What Does an Internal Medicine Resident Do?

An Internal Medicine resident is a physician who has graduated from medical school (with an M.D. or D.O. degree) and is now undergoing a supervised training program in a hospital or clinic. This three-year residency is the essential, hands-on apprenticeship required to become a board-certified specialist in Internal Medicine, a field focused on the diagnosis, treatment, and prevention of diseases in adults. Residents are often called "internists," and they are the frontline doctors for most adult patients in a hospital setting.
Their role is a unique blend of learning and practice. Under the supervision of senior residents and fully licensed "attending" physicians, residents are the primary caregivers for their patients. They are responsible for a staggering breadth of tasks that form the core of patient care.
Core Responsibilities and Daily Tasks:
- Patient Admissions: When a patient is admitted to the hospital through the emergency department or as a direct transfer, a resident conducts the initial, comprehensive evaluation. This includes taking a detailed medical history, performing a physical exam, developing a preliminary diagnosis (a "differential diagnosis"), and ordering the initial set of tests and treatments.
- Daily Rounds: Each morning, the resident team—typically composed of an attending physician, a senior resident, junior residents, and interns (first-year residents)—"rounds" on each patient. The intern presents the patient's overnight progress, new lab results, and imaging studies, and proposes a plan for the day's care. This is a critical learning experience where the attending physician provides guidance, asks probing questions, and finalizes the treatment plan.
- Executing Medical Plans: Following rounds, residents spend their day implementing the care plan. This involves writing orders for medications, scheduling consultations with specialists (like cardiologists or nephrologists), ordering diagnostic tests, and performing procedures.
- Procedures: Internal Medicine residents are trained to perform a variety of essential medical procedures, such as central line placement (inserting a large IV into a major vein), thoracentesis (draining fluid from around the lungs), paracentesis (draining fluid from the abdomen), and lumbar punctures (spinal taps).
- Documentation: A significant portion of a resident's day is spent on documentation. They must meticulously record every patient encounter, physical exam finding, and change in clinical status in the electronic health record (EHR). This is vital for patient safety, legal reasons, and billing.
- Didactic Learning: Residency is still a training program. Residents attend daily or weekly academic sessions, including "morning report" (discussing interesting cases), Grand Rounds (lectures from experts), and journal clubs (critically reviewing new research).
- On-Call Responsibilities: Residents work long hours, including nights and weekends. When "on call," a resident is responsible for handling any new admissions or urgent patient issues that arise overnight for the entire service.
### A Day in the Life of a PGY-1 Internal Medicine Intern
To make this tangible, here is a typical, grueling day for a first-year resident ("intern") on an inpatient medicine rotation:
| Time | Activity | Description |
| :--- | :--- | :--- |
| 5:30 AM | Wake Up & Arrive | Arrive at the hospital, grab a quick coffee, and head to the team room. |
| 6:00 AM | Pre-Rounding | Log into the EHR to check overnight events, new lab results, and vitals for your 8-10 patients. You physically see each patient to perform a quick check-in and targeted physical exam. |
| 8:00 AM | Attending Rounds | The entire team meets. You present each of your patients to the attending physician, detailing their status and proposing the plan for the day. This can last 2-4 hours. |
| 12:00 PM| Putting in Orders | Rounds are over. You rush to put in all the new orders for medications, imaging (X-rays, CT scans), and specialist consults discussed during rounds. |
| 1:00 PM | Noon Conference | You try to grab a free lunch provided by the hospital while attending a mandatory educational lecture on a topic like "Management of Acute Kidney Injury." |
| 2:00 PM | "The Work" | This is a blur of activity: calling consults, following up on test results, talking to families, writing progress notes, and responding to pages from nurses about patient issues (e.g., pain, fever). |
| 4:00 PM | Admissions | The "on-call" resident for the day starts getting pages from the Emergency Department about new patients who need to be admitted to your service. You go down to the ED to perform a full workup. |
| 6:00 PM | Sign-Out | You meticulously "sign out" your patient list to the night float resident who will cover them overnight. This transfer of information must be perfect to ensure patient safety. |
| 7:00 PM | Finish Notes | You stay another hour to finish your detailed admission notes and progress notes from the day. |
| 8:00 PM | Go Home | Exhausted, you head home to eat, study for a bit, and get a few hours of sleep before it starts all over again. |
This schedule illustrates why residency is more than a job—it's a total immersion experience where practical skills are forged under immense pressure.
Average Internal Medicine Residency Salary: A Deep Dive
While the work is professionally priceless, the financial compensation during residency is a frequent point of discussion and concern. It is crucial to understand that a resident's pay is not a "salary" in the traditional corporate sense but a "stipend"—a fixed payment intended to cover living expenses during a period of training. This distinction is important because it is not negotiated based on past performance or skill but is determined by the institution and the resident's post-graduate year (PGY) level.
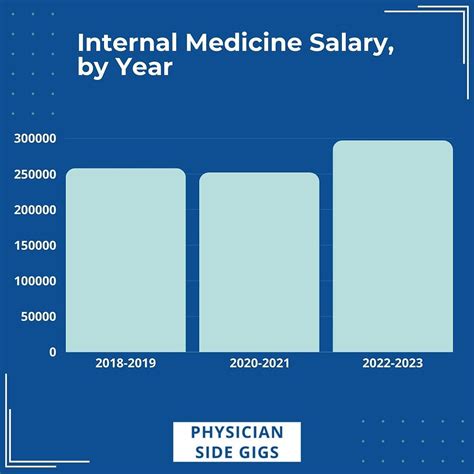
According to the 2023 Medscape Resident Salary & Debt Report, one of the most comprehensive sources in the field, the average salary for all medical residents in the U.S. was $67,400. This figure represents a modest but steady increase from previous years, driven by a greater awareness of resident wellness and rising inflation.
For Internal Medicine specifically, the compensation follows this national average very closely. The salary progresses in lockstep with the year of training, as residents gain more skills, autonomy, and responsibility.
### Internal Medicine Resident Salary by Experience Level (PGY Year)
A resident's primary "experience level" is their PGY year. Each year brings a pre-determined, non-negotiable pay increase.
| Post-Graduate Year (PGY) | Typical Salary Range | Description of Role |
| :--- | :--- | :--- |
| PGY-1 (Intern Year) | $60,000 - $66,000 | The first year of residency. Interns are closely supervised, perform initial patient workups, and carry out the bulk of the daily tasks. |
| PGY-2 (Junior Resident) | $62,000 - $69,000 | Residents take on more of a leadership and teaching role, supervising interns and medical students. They manage more complex patients and make more independent decisions. |
| PGY-3 (Senior Resident) | $65,000 - $75,000 | The final year. Seniors lead the medical team on most rotations, make high-level clinical decisions, and are responsible for the overall functioning of the service under the attending's guidance. |
| PGY-4 (Chief Resident) | $75,000 - $85,000 | An optional, selective year after residency completion. Chief Residents have significant administrative, teaching, and leadership responsibilities within the residency program. |
*Source: Data compiled and averaged from the 2023 Medscape Resident Salary & Debt Report, AAMC (Association of American Medical Colleges) residency stipend data, and individual program listings on FREIDA (the AMA Residency & Fellowship Database).*
If you were to calculate this stipend on an hourly basis, the numbers would be sobering. A resident who works the legally capped maximum of 80 hours per week at a $65,000 salary is earning approximately $15.63 per hour. This is before taxes and without any overtime pay, a rate that is often lower than many skilled hourly positions and highlights the financial sacrifice involved.
### Beyond the Stipend: The Full Compensation Package
While the base stipend is the headline number, residency programs offer a benefits package that adds significant value. This is a critical part of the overall compensation that should not be overlooked.
- Health and Disability Insurance: Programs universally provide health insurance for the resident and often offer subsidized plans for their families. Crucially, they also provide long-term disability and life insurance. This is a vital safety net for a profession with immense stress and risk.
- Malpractice Insurance: The institution provides professional liability (malpractice) insurance that covers all work done within the scope of the training program.
- Educational Funds: Most programs offer an annual stipend, typically ranging from $500 to $2,000, to be used for educational expenses. This can cover the cost of medical textbooks, question banks for board exams, conference travel, or medical equipment like stethoscopes.
- Meal Allowances: Given the long hours spent in the hospital, many programs provide meal cards or stipends for use in the hospital cafeteria. This can amount to a value of several thousand dollars per year.
- Paid Time Off (PTO): Residents typically receive 3-4 weeks of paid vacation per year. However, due to the rigid rotational schedule, taking this time can be challenging and must be planned far in advance.
- Retirement Savings Plans: Most teaching hospitals are non-profit organizations and offer access to a 403(b) retirement plan, the non-profit equivalent of a 401(k). Many programs also offer a matching contribution (e.g., matching 50% of contributions up to 6% of salary). Starting to save for retirement, even with small amounts during residency, can have a massive impact due to the power of compounding.
- Licensing and Exam Fees: Programs often cover the cost of obtaining a state training license and may reimburse for the final board certification exam (the ABIM exam), which can cost over $2,000.
- Other Perks: Depending on the institution, other benefits can include free parking, gym access, and wellness resources.
### The Elephant in the Room: Student Loan Debt
No discussion of resident salary is complete without addressing the context of medical student loan debt. According to the AAMC, the median debt for a graduating medical student in the Class of 2023 was $200,000 (not including undergraduate debt).
A ~$65,000 stipend must therefore cover not only living expenses but also significant student loan payments. Many residents opt for income-driven repayment (IDR) plans like Pay As You Earn (PAYE) or Saving on a Valuable Education (SAVE), which cap monthly payments as a percentage of their discretionary income. While this makes payments manageable during training, interest often continues to accrue, causing loan balances to grow—a phenomenon known as negative amortization. Understanding and managing this debt is a core financial challenge for every resident.
Key Factors That Influence a Resident's Salary
While the PGY-level dictates the primary salary steps, several other factors create significant variation in compensation—both during residency and, more importantly, for your future career as an attending physician. Understanding these levers is key to making strategic career decisions.
###
Post-Graduate Year (PGY) Level
As detailed in the previous section, the PGY level is the single most direct and predictable factor determining a resident's stipend. The progression from PGY-1 to PGY-3 reflects a clear path of increasing expertise and responsibility.
- PGY-1 (Intern): At the bottom of the pay scale, interns are in their most intensive learning phase. The stipend reflects their status as trainees who require constant supervision.
- PGY-2 (Junior Resident): A modest but meaningful pay bump accompanies the transition to a supervisory role. A PGY-2 is expected to lead medical students and interns, demonstrating a higher level of clinical judgment.
- PGY-3 (Senior Resident): The final year brings the highest base salary of the core residency. The PGY-3 is often the team leader, making critical decisions and requiring less direct oversight from the attending physician. The stipend reflects this near-autonomy.
- Chief Resident (PGY-4): Securing a chief resident position offers another salary increase. This role is a prestigious bridge between residency and an attending or fellowship position, focused heavily on medical education and administration. The salary for a Chief Resident often approaches or exceeds $80,000, according to data from individual program websites.
###
Geographic Location
Location is arguably the most significant variable in resident stipends. Hospitals in different regions and cities adjust their pay scales to account for the local cost of living (COL). However, these adjustments are rarely perfect, leading to substantial differences in a resident's real, take-home purchasing power.
The 2023 Medscape Resident Salary & Debt Report provides a clear regional breakdown of average resident salaries:
- Northeast: ~$71,700 (Highest)
- West: ~$69,700
- Midwest: ~$65,900
- South: ~$64,100 (Lowest)
At first glance, it seems that training in the Northeast is the most lucrative. However, this is offset by an extremely high cost of living. A resident earning $72,000 in New York City or Boston may have less disposable income than a resident earning $64,000 in a city like Houston, Texas, or Birmingham, Alabama.
High-Paying vs. High-Value Locations:
- High-Cost, High-Stipend Cities (e.g., New York, NY; San Francisco, CA; Boston, MA): These locations offer the highest nominal stipends, often including specific housing stipends to attract residents. For example, a program in Manhattan might offer a PGY-1 stipend of $75,000 plus a $5,000 housing allowance. While attractive, this often barely covers the cost of a small apartment.
- Low-Cost, Average-Stipend Cities (e.g., Kansas City, MO; Indianapolis, IN; San Antonio, TX): In these areas, a standard PGY-1 stipend of $62,000 can go much further. Residents may be able to afford to buy a home, save more aggressively, and live more comfortably during their training years.
When evaluating residency programs, it is critical to look beyond the raw salary number and research the local cost of living, particularly housing costs, to understand the true financial picture.
###
Type of Residency Program
The character and funding of the sponsoring institution also play a role in compensation and benefits. This is the closest equivalent to "company type" in the medical world.
- Major University-Affiliated Academic Medical Centers (e.g., Johns Hopkins, Mass General, UCSF): These prestigious institutions are often located in high-cost urban areas and tend to offer higher-than-average stipends. They also provide unparalleled research opportunities and networking, which can be invaluable for residents aiming for competitive fellowships or careers in academic medicine. The "brand name" on a CV can open doors for a lifetime.
- Community Hospitals (University-Affiliated or Independent): These programs are the workhorses of medical education. Located in a wider variety of geographic settings, their stipends are often closer to the national average. They may offer a more hands-on, less research-focused experience with a greater degree of autonomy, which can be excellent training for a future hospitalist or general internist.
- For-Profit/Corporate-Owned Hospitals (e.g., HCA Healthcare): A growing number of residency programs are sponsored by large, for-profit hospital systems. Stipends in these programs are competitive and often at or above the regional average. However, prospective residents should research the educational culture, patient population, and ancillary support within these systems.
###
Impact of Future Fellowship Choice on Earning Potential
While your chosen subspecialty does not affect your salary *during* your three-year Internal Medicine residency, it is the single most important factor determining your lifetime earning potential *after* residency. Internal Medicine is a gateway to a vast array of lucrative and intellectually stimulating subspecialties. The decision to pursue a fellowship (an additional 1-3+ years of training) versus becoming a general internist has massive financial implications.
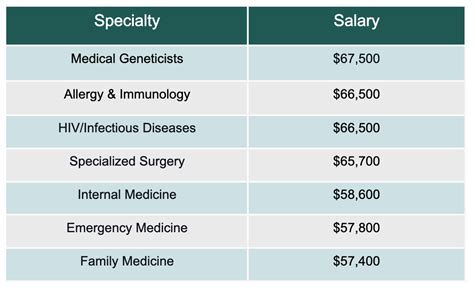
Here is a comparison of average annual attending physician salaries for General Internal Medicine versus several popular subspecialties.
| Specialty | Length of Fellowship (Post-Residency) | Average Annual Salary |
| :--- | :--- | :--- |
| General Internal Medicine (Hospitalist) | 0 years | $260,000 - $320,000 |
| Endocrinology | 2 years | $260,000 - $300,000 |
| Infectious Disease | 2 years | $250,000 - $290,000 |
| Nephrology | 2 years | $310,000 - $360,000 |
| Rheumatology | 2 years | $280,000 - $330,000 |
| Pulmonary/Critical Care | 3 years | $370,000 - $450,000 |
| Gastroenterology | 3 years | $480,000 - $570,000 |
| Cardiology (Non-Invasive) | 3 years | $450,000 - $550,000 |
| Cardiology (Invasive/Interventional) | 4-5 years | $600,000 - $750,000+ |
*Source: Data compiled and averaged from the 2023 Medscape Physician Compensation Report, Doximity Physician Compensation Report, and Salary.com.*
As the table clearly shows, procedural subspecialties like Gastroenterology and Cardiology offer significantly higher earning potential. This is due to the ability to bill for high-reimbursement procedures (like endoscopies and cardiac catheterizations). A medical student choosing an Internal Medicine residency is not just choosing a three-year path; they are opening a door to these divergent financial futures.
###
In-Demand Skills and Credentials for Future Success
During residency, your stipend is fixed. However, the skills you build and the credentials you acquire directly influence your competitiveness for top fellowships and high-paying attending jobs. These are the "skills" that boost your future salary:
- Research and Publications: Having your name on peer-reviewed publications, especially as a first author, is a massive advantage when applying for competitive fellowships at academic centers. It signals a commitment to advancing the field.
- Procedural Competence: Becoming highly skilled in the procedures common to Internal Medicine (central lines, thoracentesis, etc.) makes you a more capable and valuable resident and a more attractive candidate for hospitalist jobs or critical care fellowships.
- Leadership and Teaching: Actively teaching medical students, presenting at conferences, and ultimately earning a Chief Resident position demonstrates leadership qualities that are highly valued in both academic and private practice settings.
- Board Scores: While their importance is debated, high scores on the USMLE exams (taken in medical school) and the Internal Medicine In-Training Exam (ITE) can help you stand out. A high score on the final ABIM board certification exam is essential for practice.
Job Outlook and Career Growth for Internists

After navigating the demanding years of residency, the career outlook for a board-certified internist is exceptionally strong. The field of medicine offers a level of job security that is rare in most other industries, and internists are at the center of this demand.
The U.S. Bureau of Labor Statistics (BLS) projects that employment for physicians and surgeons will grow by **3