Table of Contents

- [Introduction](#introduction)
- [What Does a Life Flight Nurse Do?](#what-does-a-life-flight-nurse-do)
- [Average Life Flight Nurse Salary: A Deep Dive](#average-life-flight-nurse-salary-a-deep-dive)
- [Key Factors That Influence a Life Flight Nurse's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Life Flight Nurses](#job-outlook-and-career-growth)
- [How to Become a Life Flight Nurse: A Step-by-Step Guide](#how-to-get-started-in-this-career)
- [Conclusion: Is a Career as a Life Flight Nurse Right for You?](#conclusion)
---
Introduction

The rhythmic thrum of helicopter blades cutting through the air is more than just a sound; for many, it's the sound of hope. It signals the arrival of an elite team of medical professionals capable of delivering intensive care unit (ICU)-level treatment in the most extreme and unforgiving environments. At the heart of this team is the Life Flight Nurse, a clinician who combines the knowledge of critical care with the courage of a first responder. This is not just a job; it's a calling for those who run toward emergencies, equipped with the skills to turn a patient's worst day into a story of survival.
For those drawn to this high-stakes, high-reward profession, the question of compensation is a practical and important one. A life flight nurse salary reflects the immense responsibility, advanced skill set, and inherent risks of the role. Nationally, flight nurses can expect to earn an average salary ranging from approximately $85,000 to over $120,000 annually, with top earners in high-demand locations exceeding $150,000 when considering overtime, differentials, and stipends.
I once stood on a highway shut down by a multi-car accident, watching a medevac helicopter land with breathtaking precision in a makeshift zone. The calm, focused demeanor of the flight nurse who emerged, immediately taking command of the critical patient's care, was a masterclass in grace under pressure. It was a stark reminder that these professionals are the critical link between catastrophic injury and the definitive care of a trauma center.
This guide is designed to be your definitive resource for understanding every facet of a career as a life flight nurse. We will explore the responsibilities of the role, provide a comprehensive breakdown of salary expectations, dissect the factors that influence your earning potential, and lay out a clear, step-by-step roadmap to launching your own career in the sky. Whether you are a nursing student dreaming of flight suits, an experienced ICU nurse seeking your next challenge, or a paramedic considering a new path, this article will provide the expert insights you need to make an informed decision.
---
What Does a Life Flight Nurse Do?

A life flight nurse, also known as a flight nurse or critical care transport nurse, is a highly specialized registered nurse (RN) who provides comprehensive, ICU-level medical care to critically ill or injured patients during transport via helicopter (rotor-wing) or airplane (fixed-wing). They operate with a significant degree of autonomy, making high-stakes clinical decisions far from the resources of a traditional hospital setting. Their "office" is the cramped, noisy, and often turbulent cabin of an aircraft, and their patients are those in the most fragile condition.
The core of their responsibility is to stabilize and treat patients during transport from a scene of an accident or from one medical facility to another for a higher level of care. This requires a broad and deep knowledge base that spans emergency medicine, critical care, and trauma.
Core Responsibilities and Daily Tasks Include:
- Advanced Patient Assessment: Performing rapid, yet thorough, physical and neurological assessments to identify life-threatening conditions and establish a treatment plan.
- Airway Management: This is a cornerstone skill. Flight nurses are proficient in advanced airway interventions, including rapid sequence intubation (RSI), managing endotracheal tubes, and operating transport ventilators.
- Hemodynamic Monitoring: Interpreting advanced monitoring data, including arterial lines, central venous pressures, and cardiac monitors, to guide treatment with vasopressors and other life-sustaining medications.
- Medication Administration: Administering a wide array of potent medications, including sedatives, paralytics, cardiac drips, and pain management drugs, often titrating them based on real-time patient response.
- Trauma and Medical Care: Managing everything from severe traumatic injuries (e.g., chest tubes for collapsed lungs, pelvic binders, massive transfusion protocols) to complex medical emergencies like septic shock, heart attacks, or strokes.
- Specialized Care: Many flight nurses are trained to care for specific populations, such as neonatal, pediatric, or cardiac patients, which may involve managing intra-aortic balloon pumps (IABP) or extracorporeal membrane oxygenation (ECMO) circuits during transport.
- Communication and Coordination: Serving as the central communication link between the referring facility or ground crew, the receiving hospital, medical direction physicians, and the pilot. Clear, concise communication is paramount to safety and patient outcomes.
- Equipment Management: Being an expert on every piece of equipment in the aircraft, from the ventilator to the infusion pumps to the patient monitor. This includes daily checks, troubleshooting, and ensuring all gear is flight-ready.
### A Day in the Life of a Flight Nurse
07:00: The shift begins. You arrive at the base, grab a coffee, and connect with the off-going crew for a handover report. They brief you on their flights, any equipment issues, and the status of the aircraft.
07:30: You and your partner (typically another flight nurse or a flight paramedic) conduct a thorough check of all medical equipment. You run diagnostic tests on the ventilator and monitor, count every vial of medication, and ensure the drug bags are perfectly stocked. You check the oxygen levels in the aircraft and confirm all batteries are charged. Your life and your patient's life depend on this meticulous preparation.
09:00: The "hotline" rings. The dispatch center relays the mission: a scene flight for a motorcycle collision on a rural highway, one critical patient. Adrenaline sharpens your focus. You, your partner, and the pilot quickly head to the aircraft.
09:05: Liftoff. En route, the pilot receives coordinates while you and your partner review the dispatch information. You mentally run through potential injuries: head trauma, chest injuries, pelvic fractures. You assign roles—one of you will manage the airway, the other will gain IV access and assess for other injuries.
09:20: You land in a field adjacent to the highway. You exit the helicopter, grabbing your primary gear, and are met by the ground EMS crew. They give you a quick, direct report: the patient is unconscious with labored breathing.
09:25 - 09:45: You and your partner take over care. You perform a rapid assessment, confirming a critical head injury. You decide to intubate. In less than a minute, you have secured the patient's airway. An IV is established, medications are given to stabilize blood pressure, and the patient is expertly packaged onto a backboard and loaded into the helicopter.
09:50: Liftoff again, this time with a patient. The cabin is loud. You communicate with hand signals and shouts. You place the patient on the transport ventilator, continuously monitor vital signs, administer medications, and document everything meticulously on a tablet. You radio a report to the receiving trauma center, giving them a clear picture of the patient's status and your interventions.
10:10: You land at the trauma center. You transfer the patient to the trauma team, providing a detailed bedside report. The emergency department physician commends your team on the excellent pre-hospital care.
11:00: Back at the base. You thoroughly clean and decontaminate the aircraft and all equipment. You restock every item used. You and your partner debrief the mission, discussing what went well and what could be improved. The rest of the day may bring more flights or be spent on training, public relations events, or station duties, always ready for the next call.
---
Average Life Flight Nurse Salary: A Deep Dive
The salary of a life flight nurse is a reflection of their advanced education, extensive critical care experience, specialized certifications, and the high-stakes nature of their work. While compensation varies significantly based on several factors we will explore in the next section, we can establish a solid baseline by analyzing data from authoritative sources.
It's important to note that the U.S. Bureau of Labor Statistics (BLS) does not track "Flight Nurse" as a distinct profession. Instead, it groups them under the broader category of "Registered Nurses." The BLS reported the median annual wage for all Registered Nurses was $86,070 in May 2023. However, due to the specialized nature of the role, flight nurses earn considerably more than the general RN median.
To gain a more accurate picture, we must turn to salary aggregators that collect data specifically for this specialty.
### National Salary Averages and Ranges
Based on an analysis of recent data from leading salary platforms, the financial landscape for a life flight nurse in the United States looks like this:
- Payscale.com reports an average base salary for a Flight Nurse of approximately $88,670 per year. The typical range falls between $67,000 and $119,000.
- Salary.com provides a slightly higher range, indicating the average Flight Nurse salary is $96,373 per year, with a common salary bracket falling between $86,014 and $108,126.
- Glassdoor estimates a total pay average of $104,260 per year, which includes base salary and additional compensation like bonuses and profit sharing. Their likely range spans from $85,000 to $129,000 annually.
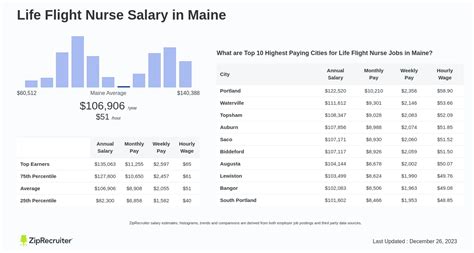
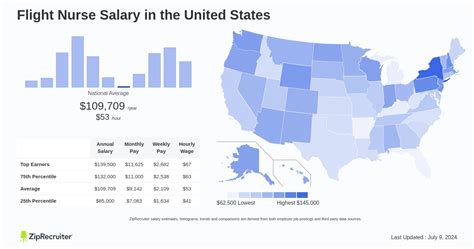
- ZipRecruiter shows an even more robust national average of $107,329 per year, with a significant number of positions paying between $94,500 and $119,000.
Synthesizing this data, we can confidently state that the average national salary for a life flight nurse is between $90,000 and $110,000 per year.
### Salary by Experience Level
Like any profession, experience is a primary driver of earning potential. A newly certified flight nurse will earn less than a seasoned veteran who has taken on leadership or educational responsibilities. Here is a breakdown of what you can expect at different stages of your flight nursing career:
| Experience Level | Typical Years of Experience | Estimated Annual Salary Range (Base) | Key Characteristics |
| ----------------------- | --------------------------- | ------------------------------------- | ---------------------------------------------------------------------------------------- |
| Entry-Level | 0-2 years (as Flight Nurse) | $80,000 - $95,000 | Has met the minimum 3-5 years of ICU/ER experience. New to the flight environment. |
| Mid-Career | 2-8 years (as Flight Nurse) | $95,000 - $115,000 | Proficient in all aspects of the job. May act as a preceptor for new hires. |
| Senior / Lead | 8+ years (as Flight Nurse) | $110,000 - $135,000+ | Often holds leadership roles (Lead Nurse, Base Manager) or specialized education roles. |
*Note: These ranges are estimates and can be significantly influenced by the factors discussed in the next section.*
### Beyond the Base Salary: A Look at Total Compensation
The annual salary figure is only part of the story. A flight nurse's total compensation package is often substantially higher due to a variety of additional pay structures and benefits. Understanding these components is crucial for evaluating a job offer.
- Overtime Pay: Due to the 12-hour or 24-hour shift models and the unpredictable nature of emergency calls, overtime is common and can significantly boost annual earnings.
- Shift Differentials: Companies almost universally offer higher pay rates for working nights, weekends, and holidays. This can add several dollars per hour to the base rate.
- On-Call Pay / Call-Back Pay: Some programs require nurses to be "on-call." They receive a small hourly stipend just for being available and are then paid a premium rate (often time-and-a-half or double-time) if they are called in to work.
- Critical Care & Certification Stipends: Many employers offer annual or hourly stipends for holding advanced certifications, particularly the Certified Flight Registered Nurse (CFRN) credential. Additional stipends may be available for holding other relevant certifications like the CCRN (Critical Care), CEN (Emergency), or specialty transport certifications.
- Charge Nurse / Preceptor Pay: Taking on the responsibility of leading a shift or training a new employee often comes with an additional hourly differential.
- Bonuses: Some for-profit companies may offer performance-based bonuses or sign-on bonuses, especially in areas with high demand for flight nurses.
- Comprehensive Benefits Package: This is a significant part of total compensation.
- Health Insurance: Medical, dental, and vision insurance.
- Retirement Plans: 401(k) or 403(b) plans, often with a generous employer match.
- Paid Time Off (PTO): Vacation, sick leave, and holidays.
- Tuition Reimbursement: Financial assistance for nurses pursuing higher education (e.g., a Master of Science in Nursing).
- Life Insurance and Disability: Employer-paid policies are standard, given the risks of the job.
- Uniform Allowance: An annual stipend to purchase flight suits and other required gear.
When all these factors are combined, it is not uncommon for a mid-career flight nurse in a competitive market to have a total annual compensation package that approaches or exceeds $150,000.
---
Key Factors That Influence a Life Flight Nurse's Salary
While the national averages provide a useful benchmark, a flight nurse's actual salary is a complex equation with multiple variables. Understanding these factors is key to maximizing your earning potential and navigating your career path effectively. This section, the most detailed in our guide, will dissect the seven primary drivers of a life flight nurse's salary.
### 1. Level of Education and Advanced Certification
Your educational foundation and specialized credentials are the bedrock of your clinical expertise and, consequently, your salary.
- Degree Level:
- Associate Degree in Nursing (ADN): While some highly experienced ADN-prepared nurses may find positions, the industry standard is shifting. It is increasingly difficult to secure a flight nurse position without a bachelor's degree.
- Bachelor of Science in Nursing (BSN): This is the de facto minimum educational requirement for most reputable flight programs. A BSN provides a broader education in nursing theory, leadership, and research, which is highly valued for the autonomous nature of flight nursing. Possessing a BSN is a prerequisite for entry into most programs and sets the baseline for salary negotiations.
- Master of Science in Nursing (MSN) / Doctor of Nursing Practice (DNP): Nurses with advanced practice degrees (e.g., Nurse Practitioner, Clinical Nurse Specialist) can command higher salaries. They may function in expanded roles, such as providing medical direction, leading quality assurance programs, or serving as a chief flight nurse. An MSN or DNP is often a prerequisite for moving into senior leadership or administrative roles within a flight program, which come with a significant pay increase.
- Mandatory Certifications: These are non-negotiable and include Basic Life Support (BLS), Advanced Cardiovascular Life Support (ACLS), and Pediatric Advanced Life Support (PALS). You must have these to even be considered.
- High-Value Specialty Certifications: This is where you can truly differentiate yourself and boost your pay.
- Certified Flight Registered Nurse (CFRN): This is the gold standard certification for flight nursing, administered by the Board of Certification for Emergency Nursing (BCEN). Earning the CFRN demonstrates a comprehensive body of knowledge specific to the transport environment. Most programs require new hires to obtain their CFRN within one to two years of employment, and nearly all offer a significant pay differential or annual bonus for maintaining it.
- Certified Emergency Nurse (CEN): Also from the BCEN, this is highly valued as it proves expertise in emergency nursing, a core component of scene response.
- Critical Care Registered Nurse (CCRN): Offered by the American Association of Critical-Care Nurses (AACN), this is often a prerequisite for applying. It validates your skills and experience in the ICU setting, where most flight nurses build their foundation.
- Transport Professional Advanced Trauma Course (TPATC) or Pre-Hospital Trauma Life Support (PHTLS): These advanced trauma certifications are often required by employers and show proficiency in managing critically injured patients outside the hospital.
Holding multiple advanced certifications not only makes you a more competitive applicant but often translates directly into higher pay through certification stipends that can add thousands of dollars to your annual income.
### 2. Years of Experience
Experience is paramount in flight nursing. It's not just about the number of years on your resume; it's about the quality and type of experience.
- Pre-Flight Experience (3-5 years minimum): No one becomes a flight nurse straight out of nursing school. Reputable programs require a minimum of three, and more commonly five, years of hands-on experience in a high-acuity critical care setting. This means working in a busy Level I or Level II Trauma Center's Emergency Department (ED) or a complex Intensive Care Unit (ICU), such as a Surgical Trauma ICU (STICU), Medical ICU (MICU), or Cardiovascular ICU (CVICU). This foundational experience is non-negotiable and is the price of entry.
- Experience as a Flight Nurse: Salary growth is directly tied to your time in the specialty.
- Novice (0-2 years): You are learning to adapt your ICU/ED skills to the unique challenges of the aircraft—the noise, the vibrations, the limited space, and the extreme autonomy. Your salary is at the lower end of the flight nurse spectrum.
- Competent (2-5 years): You are fully proficient and operate with confidence. You can handle complex cases independently and begin to act as a resource for newer team members. Your salary will see steady growth into the national average range.
- Expert/Leader (5+ years): You are a seasoned veteran. You have seen a wide variety of complex cases and can anticipate problems before they arise. This is the stage where opportunities for higher pay emerge: becoming a preceptor, a clinical educator, a base manager, or joining a specialized team (e.g., ECMO transport), all of which come with significant salary bumps.
### 3. Geographic Location
Where you work is one of the single most significant factors determining your salary. Pay scales vary dramatically by state, region, and even between urban and rural areas within the same state.
- High-Paying States: States with a high cost of living, strong nursing unions, and/or vast rural areas that rely heavily on air medical services tend to pay the most. According to data from ZipRecruiter and other sources, the top-paying states include:
- California: Often leads the nation in RN salaries across the board. Flight nurse salaries in major cities like San Francisco or Los Angeles can easily exceed $130,000 - $140,000 base pay.
- Alaska: The vast, remote geography makes air transport essential. This high demand, combined with the challenging living and working conditions, drives salaries upward.
- Washington, Oregon, Hawaii, and parts of the Northeast (New York, Massachusetts): These regions also feature a high cost of living and robust healthcare systems, leading to higher compensation.
- Lower-Paying States: States in the Southeast and parts of the Midwest tend to have a lower cost of living and, consequently, lower overall salary scales. While the pay is still excellent relative to the local economy, the absolute dollar amount will be lower than in coastal states.
- Urban vs. Rural: The dynamic can be complex.
- Major Metropolitan Areas: Often have multiple competing flight programs (both hospital-based and private) and large, well-funded health systems, driving up wages.
- Rural/Remote Bases: A base in a remote location may offer a higher "hardship" or "remote location" stipend to attract qualified nurses, sometimes making these positions surprisingly lucrative.
### 4. Company Type and Size
The organization you fly for has a direct impact on your pay structure, benefits, and overall culture.
- Hospital-Based Programs: These programs are owned and operated by a non-profit or university hospital system.
- Pros: Salaries are often competitive and transparent, listed on a clear pay scale. Benefits are typically excellent, mirroring those of the hospital system. These programs are often integrated with a Level I Trauma Center, leading to high-quality training and a strong focus on clinical excellence. Many are unionized, which can lead to better pay and working conditions.
- Cons: There may be less flexibility in salary negotiation compared to private companies.
- Private/For-Profit Companies: These are independent companies contracted by hospitals or operating on their own. Major national players include Air Methods, Global Medical Response (GMR), and Life Flight Network.
- Pros: As the largest employers of flight nurses, they have the most job openings. Pay can be very competitive, and they may offer significant sign-on bonuses to fill positions in high-need areas. There may be more opportunities for rapid advancement due to the scale of their operations.
- Cons: The focus on profit can sometimes create a different culture. Pay structures can be complex, and benefits may vary. It's crucial to carefully review any offer from a private company.
- Government/Military: Flight nurses in the U.S. Armed Forces (e.g., Air Force Critical Care Air Transport Teams - CCATTs).
- Pay Structure: Compensation is not a traditional "salary." It is based on military rank, years of service, and various allowances (housing, food). They also receive special duty pay for flight status. While the base pay might seem lower, the comprehensive benefits (free healthcare, housing allowance, pension) make it an extremely valuable package.
### 5. Clinical Specializations and Patient Populations
Specializing in a particular type of patient transport can increase your value and your salary.
- Adult Critical Care/Trauma: This is the most common flight nurse role, forming the backbone of most helicopter emergency medical services (HEMS).
- Pediatric/Neonatal (Peds/Neo) Transport: This is a highly specialized and demanding field. These nurses require specific experience in a Pediatric ICU (PICU) or Neonatal ICU (NICU) and additional certifications (e.g., C-NPT, CPEN). Due to the niche skill set and high stakes of caring for critically ill children and infants, these positions often command a higher salary or a specialist stipend.
- Fixed-Wing vs. Rotor-Wing:
- Rotor-Wing (Helicopter): Primarily used for scene response and shorter inter-facility transports (typically under 150 miles). This is the classic "life flight" role.
- Fixed-Wing (Airplane): Used for longer-distance transports, often between states or even internationally. These roles may involve more stable but still critically ill patients. The pay structure can differ, sometimes including per diems for overnight stays on long-haul flights. Some nurses are dual-qualified to work on both.
### 6. In-Demand Skills
Beyond certifications, certain practical skills make you a more capable and valuable clinician, which can be leveraged for better pay and opportunities.
- Advanced Procedural Skills: Proven competence in procedures like intubation, surgical cricothyrotomy, chest tube placement, and central line placement (where protocol allows) is highly sought after.
- Point-of-Care Ultrasound (POCUS): The ability to use a portable ultrasound to quickly assess for internal bleeding (eFAST exam), check cardiac activity,