Are you searching for a stable, in-demand career that places you at the critical intersection of healthcare and finance, but without the years of clinical training? Have you wondered how every doctor's visit, complex surgery, and routine lab test is translated into a language that insurance companies and government payers can understand and process? Welcome to the world of medical billing and coding—a profession that serves as the financial backbone of the entire healthcare industry.
For those with a keen eye for detail, an analytical mind, and a desire to play a vital role in the healthcare system, this career path offers remarkable stability and significant earning potential. The national average medical and billing coding salary demonstrates a rewarding career, with ample room for growth and specialization. I once spoke with a veteran coding auditor who described her job as being a "financial detective for the healthcare world." She said, "Every chart is a puzzle. I ensure that the clinical story is told accurately through codes so the hospital can thrive and patients can get the care they need." This perspective perfectly captures the profound importance and intellectual challenge of the work.
This comprehensive guide is designed to be your definitive resource, whether you're just beginning to explore this field or are a current professional looking to maximize your earning potential. We will dissect every component of a medical and billing coding salary, explore the factors that drive it, and provide a clear, step-by-step roadmap to launch or advance your career.
### Table of Contents
- [What Do a Medical Biller and Coder Do?](#what-do-a-medical-biller-and-coder-do)
- [Average Medical Billing and Coding Salary: A Deep Dive](#average-medical-billing-and-coding-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Do a Medical Biller and Coder Do?

While the terms "medical billing" and "medical coding" are often used interchangeably, they represent two distinct, yet deeply interconnected, functions within the healthcare revenue cycle. Think of it as a two-part process: coding is the translation, and billing is the communication. Together, they ensure that healthcare providers are paid for their services.
Medical Coding: The Art of Translation
A medical coder is a specialized professional responsible for reviewing a patient's medical records—including physician's notes, lab results, imaging reports, and surgical procedures—and translating every piece of relevant information into universal alphanumeric codes. This isn't just data entry; it's a highly analytical process that requires a strong understanding of medical terminology, anatomy, and disease processes.
The primary code sets they use are:
- ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification): These codes represent diagnoses. They answer the question, "Why did the patient seek medical care?" For example, `S82.61XA` signifies a displaced fracture of the lateral malleolus of the right fibula, initial encounter for a closed fracture.
- CPT (Current Procedural Terminology): These codes represent the services and procedures performed by the healthcare provider. They answer the question, "What did the provider do for the patient?" For example, `99213` represents an established patient office visit of low complexity.
- HCPCS Level II (Healthcare Common Procedure Coding System): These codes represent medical supplies, equipment, and services not covered by CPT codes, such as ambulance services, durable medical equipment (DME), and specific drugs.
The accuracy of this coding is paramount. It determines the amount a provider is reimbursed and creates a permanent, data-rich record used for public health statistics, research, and quality improvement studies.
Medical Billing: Securing the Revenue
A medical biller takes the codes assigned by the coder and uses them to create a "superbill" or insurance claim. They are the financial liaisons between the provider, the patient, and the insurance company (the payer). Their work ensures the translated medical story is properly submitted for payment.
Key responsibilities of a medical biller include:
- Creating and submitting accurate claims to insurance companies, Medicare, and Medicaid.
- Verifying patient insurance eligibility and benefits.
- Following up on unpaid or rejected claims, a process known as "accounts receivable (A/R) management."
- Investigating and appealing claim denials.
- Posting payments and adjustments to patient accounts.
- Generating patient statements for co-pays, deductibles, and non-covered services.
### A "Day in the Life" of a Remote Outpatient Coder
To make this more concrete, let's follow a day in the life of "Anna," a Certified Professional Coder (CPC) working remotely for a large multi-specialty clinic.
- 8:00 AM: Anna logs into her secure VPN and opens the clinic's Electronic Health Record (EHR) system, Epic. Her work queue is populated with patient encounters from the previous day's cardiology and family medicine appointments.
- 8:15 AM: She opens her first chart: a 65-year-old male with a history of hypertension and hyperlipidemia, seen for a follow-up. Anna carefully reads the physician's note, confirming the diagnoses and the complexity of the visit. She assigns ICD-10-CM codes for essential hypertension (`I10`) and mixed hyperlipidemia (`E78.2`) and verifies the CPT code for an established patient office visit (`99214`) based on the level of medical decision-making documented.
- 10:30 AM: Anna tackles a more complex chart from a new patient visit. The physician documented suspected asthma. Anna must review the spirometry test results included in the chart to confirm the final diagnosis before assigning the correct code. She uses her 3M Encoder software to help validate her code choices.
- 12:00 PM: Lunch break.
- 1:00 PM: Anna receives a query via the EHR's secure messaging system from a biller. A claim was denied for "lacking medical necessity." Anna re-reviews the chart and realizes the primary diagnosis code didn't fully support the procedure performed. She identifies a more specific secondary diagnosis code from the physician's notes, appends it to the record, and sends a note back to the biller to resubmit the claim.
- 3:00 PM: Anna attends a mandatory 30-minute webinar on upcoming changes to CPT codes for telehealth services. Continuous learning is essential in this field.
- 4:30 PM: Anna clears her queue for the day, having coded over 80 encounters. She checks her productivity and accuracy scores on her team's dashboard—both are well above the 95% accuracy target. She logs off, having played a crucial, behind-the-scenes role in patient care.
Average Medical Billing andCoding Salary: A Deep Dive
One of the most compelling aspects of a career in medical billing and coding is its solid and reliable earning potential, which grows substantially with experience and specialization. While salaries can vary widely based on several key factors we'll explore in the next section, it's essential to first establish a baseline understanding of compensation in the United States.
### National Salary Averages
To get a complete picture, we will look at data from several authoritative sources. The U.S. Bureau of Labor Statistics (BLS) groups medical coders and billers under the broader category of "Medical Records and Health Information Specialists."
- According to the U.S. Bureau of Labor Statistics (BLS), the median annual wage for medical records and health information specialists was $48,780 as of May 2023. The lowest 10 percent earned less than $35,010, and the highest 10 percent earned more than $80,090. This wide range highlights the significant impact of experience, certification, and location on earnings.
Professional organizations provide more granular data specific to certified professionals. The AAPC (American Academy of Professional Coders), the largest training and credentialing organization in the field, conducts an annual, in-depth salary survey.
- The 2024 AAPC Salary Survey reports the average annual salary for a medical coder (holding at least one AAPC credential) is $64,710. This figure is notably higher than the BLS median, underscoring the immense value of professional certification.
Let's look at other major salary aggregators to round out the data:
- Salary.com (as of early 2024) reports the median salary for a Certified Medical Coder in the U.S. is $61,003, with a typical range between $53,674 and $69,963.
- Payscale.com shows an average base salary of $51,698 per year, with a range from $37,000 to $72,000, heavily influenced by years of experience.
- Glassdoor lists a national average salary of $54,890 per year.
Key Takeaway: While entry-level positions may start in the $38,000 to $45,000 range, a certified coder can realistically expect to earn between $55,000 and $65,000 on average. Highly experienced and specialized coders can easily surpass $80,000 annually.
### Salary Progression by Experience Level
Your earning potential is not static; it follows a clear upward trajectory as you gain experience and prove your value. Here is a typical salary progression, compiled from AAPC and Payscale data:
| Experience Level | Years in Field | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $40,000 - $52,000 | Often holds one core credential (e.g., CPC-A, CCA). Focus is on learning systems, building speed, and maintaining accuracy. May have work reviewed by a senior coder. |
| Mid-Career | 3-9 Years | $53,000 - $68,000 | Holds a core credential (CPC) and possibly a second specialty credential. Works independently, handles more complex cases, and may begin to mentor junior coders. |
| Senior/Experienced | 10-19 Years | $69,000 - $80,000 | Holds multiple certifications. Often specializes in a high-demand area like auditing, compliance, or surgical coding. May serve as a team lead or subject matter expert. |
| Expert/Lead | 20+ Years | $80,000+ | Moves into management, education, or high-level auditing/compliance roles. Often holds advanced credentials like the CPMA (Certified Professional Medical Auditor) or CDEO (Certified Documentation Expert Outpatient). |
*(Salary ranges are approximate and can be influenced by all factors discussed in the next section.)*
### Beyond the Base Salary: A Look at Total Compensation
Your salary is just one piece of the puzzle. When evaluating a job offer, it's crucial to consider the full compensation package, which can add significant value. For medical coders and billers, especially those working for hospitals, large clinics, or insurance companies, these benefits are often robust.
- Bonuses: While not universal, performance-based bonuses are common. These can be tied to productivity (number of charts coded per hour) and accuracy (maintaining a 95% or higher accuracy rate). The AAPC survey notes that 34% of respondents received a bonus, with the average bonus amount being around $2,500.
- Health Insurance: Comprehensive medical, dental, and vision insurance is a standard benefit, often with the employer covering a significant portion of the premium. This is a highly valuable, non-taxable benefit.
- Retirement Savings Plans: Access to a 401(k) or 403(b) plan is a cornerstone of compensation. Many employers offer a matching contribution (e.g., matching 100% of your contribution up to 3-6% of your salary), which is essentially free money for your retirement.
- Paid Time Off (PTO): This includes vacation days, sick leave, and paid holidays. The amount typically increases with seniority.
- Continuing Education Units (CEUs): To maintain certification, coders must complete a certain number of CEUs annually. Many employers support this by providing an annual stipend for memberships (AAPC, AHIMA), webinars, and conference attendance.
- Tuition Reimbursement: Some larger organizations offer tuition assistance for employees pursuing higher education, such as an Associate's or Bachelor's degree in Health Information Management.
- Remote Work Stipend: With the rise of remote work, some companies offer a stipend to help cover the costs of home office equipment, internet, and supplies.
When you factor in these benefits, the total value of a medical coding position can be 20-30% higher than the base salary alone.
Key Factors That Influence Salary

Your medical and billing coding salary isn't a single, fixed number. It's a dynamic figure influenced by a combination of your qualifications, choices, and environment. Understanding these factors is the key to maximizing your earning potential throughout your career. This section provides an in-depth analysis of the six primary drivers of compensation.
###
1. Level of Education & Certification
This is arguably the most significant factor you can control. In the world of medical coding, certification is not just an advantage; it is a requirement for most quality jobs. An uncertified coder will earn significantly less—if they can find a position at all.
Educational Pathways:
- Certificate/Diploma Program: This is the fastest route, typically taking 9-12 months. These programs are laser-focused on the core competencies needed for coding certification. They are an excellent, cost-effective choice for career changers.
- Associate's Degree (AAS/AS): A two-year degree in Medical Billing and Coding or Health Information Technology (HIT) is highly regarded by employers. It provides a deeper foundation in healthcare operations, law, and ethics alongside coding skills. An Associate's degree often leads to a higher starting salary and prepares graduates for the RHIT (Registered Health Information Technician) credential.
- Bachelor's Degree (BS): A four-year degree in Health Information Management (HIM) or a related field is the gold standard for those with leadership aspirations. It positions you for higher-level roles like department manager, compliance officer, or data analyst and is a prerequisite for the prestigious RHIA (Registered Health Information Administrator) credential. According to the AAPC, professionals with a Bachelor's degree earn, on average, over $10,000 more annually than those with just a high school diploma.
The Power of Certifications:
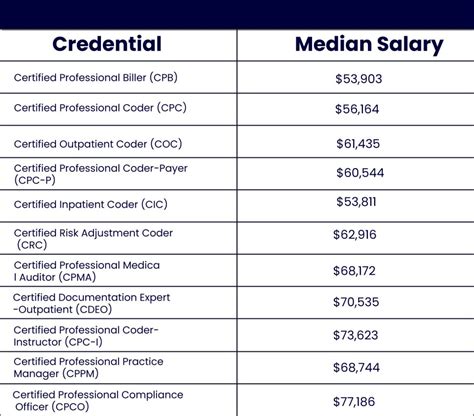
Certifications are issued by professional bodies like the AAPC and AHIMA and serve as proof of your expertise. More (and more advanced) certifications directly translate to higher pay.
AAPC Credentials (The Gold Standard for Physician-Based/Outpatient Coding):
- CPC (Certified Professional Coder): The most recognized and sought-after credential for outpatient coding. Obtaining your CPC is the single most important step you can take to launch your career. The "A" (Apprentice) status is removed after two years of experience, leading to a salary jump.
- *Average Salary with CPC:* $63,095 (Source: AAPC 2024 Survey)
- COC (Certified Outpatient Coder): Formerly CPC-H, this credential focuses on coding for hospital outpatient facilities like emergency departments and ambulatory surgery centers.
- *Average Salary with COC:* $71,118
- CIC (Certified Inpatient Coder): This credential validates expertise in the complex world of hospital inpatient coding (using ICD-10-CM and PCS). It is one of the highest-paying core credentials due to the difficulty of the work.
- *Average Salary with CIC:* $81,034
- CRC (Certified Risk Adjustment Coder): This is a rapidly growing and lucrative specialty focused on coding for patient risk scores, which impacts payments in value-based care models.
- *Average Salary with CRC:* $74,013
AHIMA Credentials (Highly Respected in Hospital/Inpatient Settings):
- CCA (Certified Coding Associate): An entry-level credential demonstrating foundational coding competency.
- CCS (Certified Coding Specialist): A mastery-level credential respected for its rigorous testing of both inpatient and outpatient coding skills.
- RHIT (Registered Health Information Technician): Requires an Associate's degree from a CAHIIM-accredited program. Focuses on broader health information management, including data quality, privacy, and security.
- RHIA (Registered Health Information Administrator): Requires a Bachelor's degree from a CAHIIM-accredited program. Prepares professionals for management and leadership roles.
The Multi-Credential Advantage: The AAPC survey clearly shows a "stacking" effect.
- Coders with one credential average $62,110.
- Coders with two credentials average $71,535.
- Coders with three or more credentials average $79,933.
###
2. Years of Experience
As with most professions, experience is a powerful driver of salary. In medical coding, experience translates to speed, accuracy, and the ability to handle increasingly complex medical cases without supervision.
- 0-2 Years (Entry-Level): This is the learning phase. Coders are building proficiency with EHR systems and coding software. They may hold an apprentice-level credential (CPC-A) and have their work reviewed by auditors. The focus is on proving reliability and accuracy.
- 3-9 Years (Mid-Career): By this stage, coders are fully proficient. They work independently, meet productivity and accuracy standards consistently, and have likely removed their apprentice status. Their salary sees a significant jump as they become dependable assets. Many will pursue a second specialty certification during this period to further boost their value.
- 10+ Years (Senior/Expert): These are the veterans of the field. They possess deep expertise, often in a specialized area. They act as mentors, team leads, or subject matter experts. Many transition into higher-paying adjacent roles like:
- Medical Coding Auditor: Reviewing the work of other coders for accuracy and compliance. Average salary: $82,367 (AAPC, with CPMA credential).
- Compliance Officer: Ensuring the organization adheres to all healthcare regulations.
- Educator/Trainer: Teaching the next generation of coders.
- Manager/Supervisor: Leading a team of coders and managing departmental workflow.
###
3. Geographic Location
Where you live and work has a major impact on your paycheck, driven primarily by local market demand and cost of living. A salary that feels comfortable in a rural state might be difficult to live on in a major metropolitan area.
The BLS provides excellent state and metropolitan-level data for "Medical Records and Health Information Specialists."
Top-Paying States (Annual Mean Wage, BLS May 2023):
1. New Jersey: $73,350
2. District of Columbia: $71,110
3. California: $64,280
4. Maryland: $63,680
5. Hawaii: $62,940
Top-Paying Metropolitan Areas:
1. San Jose-Sunnyvale-Santa Clara, CA: $85,550
2. Trenton, NJ: $78,510
3. San Francisco-Oakland-Hayward, CA: $75,120
4. Sacramento-Roseville-Arden-Arcade, CA: $71,850
5. New York-Newark-Jersey City, NY-NJ-PA: $68,960
Conversely, salaries are typically lower in states with a lower cost of living, primarily in the Southeast and Midwest.
The Rise of Remote Work: The pandemic accelerated the shift to remote work for coders, which adds a new dimension to location-based pay. Many national companies are now adopting location-based pay tiers. This means they may adjust your salary based on the cost-of-living index of your home city, even if the company is based in a high-cost area. However, other companies pay a flat national rate, allowing coders in low-cost areas to significantly increase their real-world earning power. When seeking remote roles, it's crucial to clarify the company's policy on geographic pay differentials.
###
4. Work Environment & Employer Type
The type of facility you work for dictates the complexity of the coding and, consequently, your salary.
- Hospitals (Large Health Systems): These are typically the highest-paying employers.
- Inpatient Coding: This is the most complex type of coding, requiring a deep understanding of the DRG (Diagnosis-Related Group) system. Inpatient coders are in high demand and command top salaries.
- Outpatient/Ambulatory Surgery Coding: Still complex, but generally less so than inpatient. Involves coding for ER visits, same-day surgeries, and clinics owned by the hospital.
- Physician's Offices & Clinics: These can range from a small, single-physician practice to a large multi-specialty group. Salaries are generally solid but may be slightly lower than in a hospital setting. The work-life balance can sometimes be more predictable.
- Specialty Clinics: Working for an oncology, cardiology, or orthopedic practice requires specialized knowledge. Coders who master the intricate procedures and diagnoses of a specific specialty are highly valuable and can command higher-than-average salaries.
- Third-Party Billing/Coding Companies: These companies contract their services out to providers. The environment can be fast-paced and production-driven
