Are you a medical professional or student seeking a career that blends clinical expertise with a population-level impact? Do you envision a role that moves beyond the traditional cycle of treating acute illness and instead focuses on prevention, workplace wellness, and shaping healthier work environments? If you're looking for a specialty that offers a compelling combination of intellectual challenge, excellent work-life balance, and a highly competitive salary, then occupational medicine may be the perfect fit. While many medical paths lead to burnout, this field offers a sustainable and deeply rewarding alternative.
The average occupational medicine salary reflects the high value placed on this unique skill set, with most physicians earning well over $250,000 annually. As a career analyst, I once advised a family friend, a brilliant but exhausted emergency room physician, who was on the verge of leaving medicine altogether. After exploring several specialties, she discovered occupational medicine and found not just a new job, but a renewed passion for her profession—one that allowed her to use her skills proactively and enjoy a predictable schedule. This guide is designed to provide you with that same level of clarity, offering an exhaustive look into the financial rewards, career trajectory, and daily realities of this fascinating and vital field.
This comprehensive article will serve as your ultimate resource, breaking down everything you need to know about a career in occupational medicine.
### Table of Contents
- [What Does an Occupational Medicine Physician Do?](#what-does-an-occupational-medicine-physician-do)
- [Average Occupational Medicine Salary: A Deep Dive](#average-occupational-medicine-salary-a-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors-that-influence-your-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in Occupational Medicine](#how-to-get-started-in-occupational-medicine)
- [Is a Career in Occupational Medicine Right for You?](#is-a-career-in-occupational-medicine-right-for-you)
What Does an Occupational Medicine Physician Do?

Occupational medicine is a specialized branch of preventive medicine focused on the health, safety, and performance of workers. At its core, an occupational medicine (OM) physician is the crucial bridge between clinical medicine and the workplace. They are medical detectives, patient advocates, and strategic advisors, all rolled into one. Their "patient" is not just the individual employee but the entire work environment.
Unlike a primary care physician who treats a broad range of community-acquired illnesses, an OM physician's scope is specifically centered on the interaction between a worker's health and their job. This includes preventing and treating work-related injuries and illnesses, promoting overall health and wellness within an organization, and ensuring compliance with a complex web of health and safety regulations.
Their responsibilities are diverse and extend far beyond a typical clinic. Here’s a breakdown of their core duties:
- Clinical Care: This is the most direct patient-facing aspect. It involves diagnosing and treating injuries and illnesses that occur on the job, such as musculoskeletal injuries from repetitive tasks, chemical exposures, or traumatic accidents.
- Medical Surveillance: They design and implement programs to monitor employees who are exposed to specific workplace hazards, like lead, asbestos, or loud noise. This includes regular health screenings to detect early signs of occupational disease.
- Disability Management and Return-to-Work Programs: When a worker is injured or becomes ill (whether work-related or not), the OM physician plays a pivotal role in assessing their fitness for duty. They develop and manage programs to help employees return to work safely and productively, often recommending modified duties or workplace accommodations.
- Workplace Hazard Assessment: OM physicians often leave the clinic to conduct on-site evaluations. They walk through factories, construction sites, and office buildings to identify potential health and safety risks, from poor ergonomics at a desk to inadequate ventilation in a manufacturing plant.
- Preventive Services & Wellness Promotion: This is the proactive side of the job. They may lead corporate wellness initiatives, deliver training on injury prevention, implement vaccination programs, and advise on strategies to reduce workplace stress and burnout.
- Regulatory Compliance and Consultation: They are experts in regulations from the Occupational Safety and Health Administration (OSHA), the Americans with Disabilities Act (ADA), and the Family and Medical Leave Act (FMLA). They advise companies on how to remain compliant, manage workers' compensation cases, and develop sound health and safety policies.
### A Day in the Life of an Occupational Medicine Physician
To make this more concrete, let's imagine a day for Dr. Anya Sharma, a board-certified OM physician working for a large manufacturing company.
- 8:00 AM - 9:30 AM: Dr. Sharma starts her day reviewing new injury reports and outstanding workers' compensation cases with the company's safety manager and HR representative. They discuss an employee who needs modified duty after a back injury and strategize on a return-to-work plan.
- 9:30 AM - 12:00 PM: Clinic hours. She sees several patients: a follow-up for a welder with a corneal flash burn, a new evaluation for an assembly line worker with carpal tunnel syndrome symptoms, and an employee for a pre-placement physical.
- 12:00 PM - 1:00 PM: Lunch meeting with the director of operations to discuss the results of a recent noise survey on the factory floor and recommend areas where improved hearing protection is mandatory.
- 1:00 PM - 3:00 PM: On-site walkthrough. Dr. Sharma puts on a hard hat and safety glasses and walks the factory floor with an industrial hygienist. They observe a new robotic arm installation to assess its ergonomic impact on human workers nearby and identify any potential new hazards.
- 3:00 PM - 4:30 PM: Administrative block. She completes her clinical notes, provides detailed documentation for disability cases, and responds to emails from legal counsel regarding an OSHA inquiry.
- 4:30 PM - 5:00 PM: Dr. Sharma reviews the curriculum for a "back safety" training session she is scheduled to lead for warehouse staff next week, ensuring it is engaging and practical.
This example highlights the dynamic and multifaceted nature of the role—a blend of clinical practice, corporate strategy, and on-the-ground investigation.
Average Occupational Medicine Salary: A Deep Dive
The financial compensation for occupational medicine physicians is a significant draw, reflecting the specialized training and the immense value these professionals bring to organizations. While it may not always reach the highest echelons of surgical subspecialties, it offers an exceptional income combined with a quality of life that is rare in medicine.
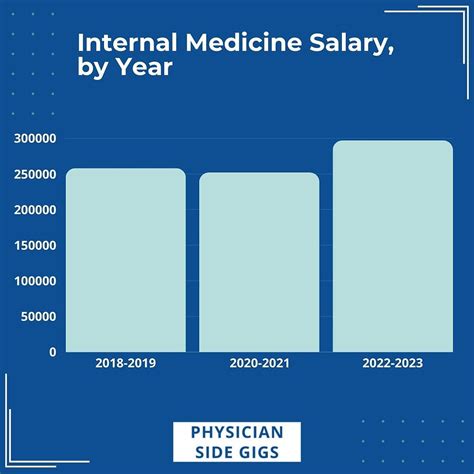
According to the 2023 Medscape Physician Compensation Report, one of the most respected annual surveys in the industry, the average annual salary for physicians in Public Health & Preventive Medicine (the category that includes occupational medicine) is $249,000. However, this figure represents a broad average and often serves as a baseline. Data from other authoritative sources suggests that compensation for dedicated occupational medicine specialists, particularly those with board certification and experience, is significantly higher.
For instance, Salary.com, which aggregates real-time employer-reported data, places the median annual salary for an "Occupational Medicine Physician" in the United States at $280,593 as of late 2023. The typical salary range falls between $242,525 and $334,185. This demonstrates the substantial earning potential within the field.
It's crucial to understand that these numbers represent the base salary and the total compensation package is often much larger.
### Salary Progression by Experience Level
Like all medical specialties, compensation in occupational medicine grows significantly with experience, expertise, and assumption of leadership responsibilities. The salary trajectory is robust, rewarding those who commit to the field for the long term.
| Experience Level | Typical Annual Salary Range | Key Responsibilities & Notes |
| :--- | :--- | :--- |
| Entry-Level (0-3 Years) | $220,000 - $265,000 | Post-residency, often working as a staff physician in a clinic or hospital-based setting. Focus is on clinical duties and learning the specific industry or company's needs. Board certification is typically in progress or recently achieved. |
| Mid-Career (4-10 Years) | $265,000 - $310,000 | Physicians are board-certified and have established expertise. They may take on roles like Clinic Medical Director, manage small teams, and have more involvement in program development and corporate strategy. |
| Senior/Experienced (11-20+ Years) | $310,000 - $400,000+ | These are seasoned experts, often in high-level leadership positions such as Regional Medical Director or Corporate Medical Director. A significant portion of their time is dedicated to strategy, policy, budget management, and C-suite advising. Earnings can exceed $400,000 in corporate roles. |
*Sources: Data compiled and synthesized from Salary.com, Medscape, and industry reports from professional recruiting firms like Merritt Hawkins.*
### Deconstructing the Total Compensation Package
The base salary is only one piece of the puzzle. An OM physician's total compensation package is a comprehensive suite of financial rewards and benefits. Understanding these components is essential for evaluating a job offer.
- Base Salary: The guaranteed annual income. In most occupational medicine roles, this is a fixed salary rather than being based on productivity metrics like Relative Value Units (RVUs), which are common in other specialties. This contributes to lower stress and greater income predictability.
- Annual Bonuses: These are extremely common and can add a significant amount to the total take-home pay. Bonuses can be tied to:
- Company Performance: If the physician is employed directly by a corporation, their bonus may be linked to the overall profitability of the company.
- Departmental Goals: Achieving targets related to reducing lost workdays, lowering injury rates, or successful implementation of a new wellness program.
- Personal Performance: Based on an annual review of the physician's contributions.
- Typical Bonus Amount: Bonuses can range from 10% to 30% or more of the base salary, especially in senior corporate roles.
- Profit Sharing: More common in physician-owned private practice groups. A portion of the practice's annual profits is distributed among the physician partners.
- Retirement Benefits: This is a major component of long-term wealth building.
- 401(k) or 403(b) Plans: Almost all employers offer these tax-advantaged retirement accounts. The key differentiator is the employer match. A generous match (e.g., 100% of contributions up to 6% of salary) can be worth tens of thousands of dollars per year.
- Pension Plans: While increasingly rare, some government and older, established corporate positions may still offer defined-benefit pension plans, providing a guaranteed income stream in retirement.
- Continuing Medical Education (CME) Stipend: Employers provide an annual allowance (typically $3,000 - $7,000) to cover the costs of attending conferences, subscribing to journals, and completing other educational activities required to maintain medical licensure and board certification.
- Insurance: Comprehensive health, dental, and vision insurance for the physician and their family is standard. Crucially, employers also cover the full cost of malpractice insurance.
- Paid Time Off (PTO): Generous vacation, sick leave, and holiday packages are typical, usually starting at 4-6 weeks per year and increasing with seniority.
- Other Perks: Depending on the employer, this can include stock options or grants (highly lucrative in corporate roles), relocation assistance, and coverage for professional association dues (e.g., for the American College of Occupational and Environmental Medicine - ACOEM).
When considering an occupational medicine salary, it's vital to look beyond the base number and evaluate the entire compensation structure. A role with a slightly lower base salary but with a substantial bonus potential, excellent retirement match, and stock options could be far more financially advantageous in the long run.
Key Factors That Influence Your Salary
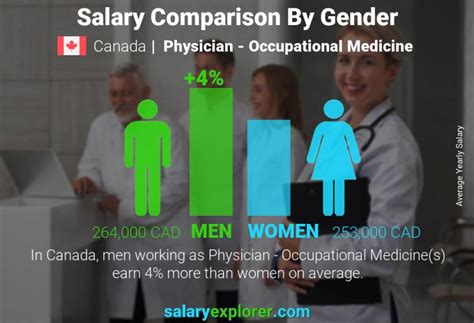
An occupational medicine salary is not a monolith. It is a dynamic figure shaped by a confluence of factors. A physician earning $250,000 and another earning $380,000 in the same field could be separated by their credentials, location, or practice setting. Understanding these variables is the key to maximizing your earning potential throughout your career. This section provides an in-depth analysis of the most significant salary drivers.
###
Level of Education and Board Certification
This is arguably the most important foundational factor. While a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree is the mandatory entry ticket, further specialization is what unlocks the highest salary tiers.
- Board Certification: The single most critical credential is board certification in occupational medicine, administered by the American Board of Preventive Medicine (ABPM). Achieving this certification signifies that a physician has completed a specialized residency program and passed a rigorous examination, demonstrating a high level of expertise in the field. Employers overwhelmingly prefer or require board-certified candidates and compensate them accordingly. A non-board-certified physician performing occupational health duties will almost always earn significantly less than their certified counterparts. The salary difference can easily be $50,000 or more annually.
- Master of Public Health (MPH): This is a highly valuable and common complementary degree for OM physicians. Many residency programs integrate an MPH into their curriculum. An MPH provides essential training in epidemiology, biostatistics, environmental health sciences, and health policy—all of which are central to occupational medicine. It equips physicians with the skills to think on a population level, design effective health programs, and analyze workplace health data. While not a direct 1:1 salary booster like board certification, it makes a candidate far more competitive for top-tier academic, government, and corporate leadership roles.
- Master of Business Administration (MBA): For physicians aiming for the C-suite—roles like Corporate Medical Director or Chief Medical Officer—an MBA can be a powerful differentiator. It provides a deep understanding of finance, operations, management, and strategy. A physician with an MD/MPH/MBA trifecta is exceptionally well-positioned for the highest-paying executive roles in large corporations, where compensation can soar well into the $400,000 - $500,000+ range when including bonuses and stock options.
###
Years of Experience
As detailed in the previous section, experience is a primary driver of salary growth. However, it’s not just about the number of years; it’s about the *type* of experience gained. The career ladder and its corresponding salary increases typically look like this:
- Foundation Stage (Years 0-3): Salary: ~$220k - $265k. The focus is on honing clinical skills related to workplace injuries, understanding regulatory frameworks like OSHA and workers' comp, and achieving board certification.
- Growth Stage (Years 4-10): Salary: ~$265k - $310k. At this point, the physician transitions from a purely clinical role to one with more responsibility. They might become the lead physician at a multi-provider clinic or the primary medical contact for a specific business unit within a large company. Their expertise is now sought for program development and preventive strategy, not just reactive treatment.
- Leadership Stage (Years 11-20): Salary: ~$310k - $400k. Experience now translates into leadership. This is the stage of the Clinic Medical Director, Regional Medical Director, or Associate Corporate Medical Director. Responsibilities shift heavily toward management, budgeting, strategic planning, and mentoring junior physicians.
- Executive Stage (Years 20+): Salary: $400k+. This is the pinnacle of the corporate or large healthcare system track. As a Corporate Medical Director or CMO, the physician is a key executive, shaping health and safety policy for an entire global organization, interacting with other C-suite leaders, and managing a multi-million dollar budget. Their compensation package reflects this executive-level responsibility.
###
Geographic Location
Where you practice has a profound impact on your paycheck. This variation is driven by the cost of living, regional demand for OM specialists, and the concentration of specific industries.
High-Paying States and Regions:
States with a heavy presence of manufacturing, energy (oil and gas), technology, or logistics industries tend to have higher demand and thus pay more for OM physicians.
- California: Particularly in areas with large tech companies and extensive agriculture and manufacturing. (e.g., San Jose, Los Angeles)
- Texas: The booming oil and gas sector, along with massive manufacturing and logistics hubs, creates high demand. (e.g., Houston, Dallas)
- New York: Driven by corporate headquarters, transportation, and complex regulatory environments. (e.g., New York City)
- Midwest States (e.g., Illinois, Ohio, Michigan): A strong, established manufacturing and industrial base ensures a consistent need for OM experts.
- Alaska: Extreme conditions and the oil industry drive salaries significantly higher to attract talent.
According to Salary.com, a physician in San Jose, CA, might earn 25% more than the national average, while a physician in a smaller Midwestern city might earn closer to the average.
Lower-Paying States and Regions:
Conversely, states with lower costs of living and economies less reliant on heavy industry may offer lower salaries, though the purchasing power can still be excellent. These often include rural areas in the Southeast and some parts of the Mountain West.
It is essential to use a cost-of-living calculator to compare offers. A $280,000 salary in Houston, TX may provide a much higher quality of life than a $310,000 salary in San Francisco, CA.
###
Company Type & Size (Practice Setting)
The type of organization you work for is one of the most significant determinants of your salary and overall experience.
- Corporate / In-House: (Highest Potential). Working directly for a large Fortune 500 company (e.g., a tech giant, an automotive manufacturer, or a chemical company) often yields the highest salaries and best benefits. These companies view their medical department as a strategic asset for mitigating risk and enhancing productivity. Compensation includes a high base salary, significant bonuses, and often, lucrative stock options.
- Large Private Occupational Health Groups: (e.g., Concentra, WorkCare). These national or regional groups provide outsourced OM services to a multitude of companies. Pay is very competitive and often includes productivity or clinic-profitability bonuses. The pace can be fast, with a focus on high-volume clinical care.
- Hospital-Employed: Many hospital systems have their own occupational health departments to serve local employers. Salaries are strong and stable, often benchmarked against other hospital-employed specialists. Benefits are typically excellent, but bonus potential may be less than in a corporate setting.
- Government: (e.g., Department of Veterans Affairs (VA), OSHA, NIOSH, Military). (Best Work-Life Balance). The top-end salary is generally lower than in the private sector. However, the trade-off is exceptional job security, a predictable 40-hour work week, generous federal holidays, and a defined-benefit pension plan (a rarity today).
- Academic Medicine: Working for a university medical center involves a mix of clinical work, teaching residents, and conducting research. The base salary is typically lower than in private practice or corporate roles. However, the appeal lies in the intellectual environment, the opportunity to shape the next generation of physicians, and the pursuit of research interests.
- Private Practice / Consulting: This path offers the highest autonomy and potentially unlimited income, but also carries the most risk. An experienced OM physician with a strong reputation can start their own consulting firm, advising multiple companies on health policy, complex disability cases, or toxicology. Success depends entirely on business acumen and the ability to build a client base.
###
Area of Specialization
While occupational medicine is itself a specialty, further sub-specialization can enhance earning potential. This is less about formal fellowships (though some exist) and more about developing deep expertise in a high-demand niche.
- Medical Directorship: The most common form of specialization is leadership. Progressing to a clinic, regional, or corporate medical director role is the clearest path to a higher salary.
- Toxicology: Expertise in the effects of chemical and physical agents on the human body is highly sought after by chemical, pharmaceutical, and manufacturing companies.
- Aerospace Medicine: A niche field focused on the health of pilots, astronauts, and aircrew, dealing with issues like hypoxia, spatial disorientation, and the effects of G-forces.
- Disability and Impairment Evaluation: Becoming a go-to expert in performing complex Independent Medical Examinations (IMEs) and impairment ratings for workers' compensation and legal cases can be a lucrative side-business or a full-time focus.
- Ergonomics: Specializing in the design of workspaces and tasks to prevent musculoskeletal disorders is valuable for companies in both office and industrial settings.
###
In-Demand Skills
Beyond medical knowledge, certain non-clinical skills dramatically increase an OM physician's value and, consequently, their salary.
- Business Acumen: Understanding concepts like Return on Investment (ROI), profit and loss, and operational efficiency. The ability to articulate how a wellness program reduces insurance costs or how an ergonomic intervention increases productivity is invaluable.
- Leadership and Management: The ability to lead a team of nurses, physical therapists, and administrative staff, manage budgets, and align departmental goals with the larger organization's mission.
- Data Analysis: Using data to identify injury trends, measure the effectiveness of interventions, and present clear, compelling reports to non-medical executives.
- Communication and Negotiation: Skillfully communicating with diverse stakeholders—from an injured union worker to the company's CEO and legal team. This includes negotiation skills for developing return-to-work plans that satisfy all parties.
- Regulatory Expertise: Deep, up-to-date knowledge of OSHA, ADA, FMLA, and state-specific workers' compensation laws is non-negotiable and a core competency that commands a premium.
By strategically developing these factors—pursuing board certification, gaining leadership experience, choosing a high-demand location and practice setting, and honing key business skills—a physician can actively steer their occupational medicine salary toward its maximum potential.
Job Outlook and Career Growth

For anyone considering a long-term commitment to a medical specialty, the future viability of the field is just as important as the current salary. The job outlook for occupational medicine physicians is exceptionally strong, driven by enduring economic, regulatory, and social trends. This is a field poised for stability and growth in the coming decade and beyond.
The U.S. Bureau of Labor Statistics (BLS), in its Occupational Outlook Handbook, projects that employment for all physicians and surgeons will grow by 3 percent from 2022 to 2032. While this may seem modest, it's crucial to understand the context for occupational medicine. This overall figure is an average across all specialties, some of which are more saturated. The specific demand for OM physicians is fueled by unique factors that suggest a much more robust outlook.
Why the Future is Bright for Occupational Medicine:
- An Aging Workforce: As the baby boomer generation remains in the workforce longer, there is an increased prevalence of chronic diseases (e.g., heart disease, diabetes) and age-related musculoskeletal issues. OM physicians are essential for managing these conditions in the context of work, ensuring employees can remain productive and safe on the job.
- Increased Focus on Corporate Wellness and ESG: Modern corporations are under growing pressure to prioritize employee well-being as part of their Environmental, Social, and Governance (ESG) initiatives. A healthy, safe workforce is no longer just a cost-mitigation strategy; it's a marker of a responsible and attractive employer. OM physicians are the strategic leaders who design and implement these critical wellness and safety programs.
- Complex and Ever-Evolving Regulations: The landscape of workplace health and safety law (OSHA, ADA, etc.) is constantly changing. Companies rely on the expert guidance of OM physicians to navigate this complexity, avoid costly fines, and mitigate legal risk. This need is perpetual and non-negotiable for businesses of all sizes.
- The Post-Pandemic Legacy: The COVID-19 pandemic permanently elevated the importance of infectious disease preparedness in the workplace. OM physicians are now at the forefront