Introduction

For those with a unique blend of scientific acumen, unwavering calm under pressure, and a profound sense of compassion, the field of pediatric anesthesiology represents a pinnacle of medical practice. It's a career that asks for everything you have—intellectually, emotionally, and physically—but offers immense rewards in return. Imagine being the steady hand and reassuring presence that guides a child and their family through the anxiety of surgery, ensuring safety and comfort during their most vulnerable moments. This is not just a job; it is a sacred trust.
Financially, the commitment required is mirrored by significant compensation, with the average pediatric anesthesia salary often ranking among the highest in the medical profession. Professionals in this field can expect to earn well into the six-figure range, with top earners exceeding half a million dollars annually. I once had the privilege of speaking with a senior pediatric anesthesiologist at a leading children's hospital. She didn't talk about the money; she described her role as "making a promise to a parent"—a quiet, solemn vow to watch over their child as if they were her own and return them safely. That profound sense of duty, combined with the intellectual challenge and financial stability, makes this a uniquely compelling career path.
This comprehensive guide is designed to be your definitive resource, whether you're a high school student dreaming of a medical career, a medical student choosing a specialty, or a current physician considering a fellowship. We will delve deep into every facet of this profession, providing an authoritative look at salary expectations, the factors that shape your income, the long-term career outlook, and a clear, step-by-step roadmap to achieving your goal.
### Table of Contents
- [What Does a Pediatric Anesthesiologist Do?](#what-does-a-pediatric-anesthesiologist-do)
- [Average Pediatric Anesthesia Salary: A Deep Dive](#average-pediatric-anesthesia-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
---
What Does a Pediatric Anesthesiologist Do?

A pediatric anesthesiologist is a fully trained anesthesiologist who has completed at least one additional year of specialized fellowship training in the anesthetic care of children. Their practice spans the entire spectrum of childhood, from premature neonates weighing just a few pounds to robust teenagers on the cusp of adulthood. Their core responsibility is to ensure a patient's safety, comfort, and physiological stability before, during, and after surgical or diagnostic procedures.
However, the role is far more nuanced than simply "putting a child to sleep." Children are not small adults. Their physiology is dramatically different and constantly changing. A pediatric anesthesiologist must possess an expert understanding of:
- Pediatric Physiology and Pharmacology: How a newborn's heart, lungs, kidneys, and liver function differently from a toddler's or a teen's. This directly impacts how drugs are metabolized and what doses are safe.
- Airway Management: A child's airway is smaller, more conical, and more prone to obstruction. Securing an airway with an endotracheal tube or other device is a critical, high-stakes skill that requires specialized equipment and techniques.
- Fluid and Temperature Management: Infants and small children have a higher surface-area-to-volume ratio, making them susceptible to rapid heat loss and dehydration. Meticulous management is crucial.
- Congenital Conditions: Many pediatric patients have complex congenital heart, lung, or other organ system abnormalities that profoundly affect the anesthetic plan.
- Psychological and Emotional Support: A key part of the job is alleviating the fear and anxiety of both the child and their parents. This involves building rapport, using age-appropriate communication, and sometimes employing pre-medication to ease the separation from parents.
### A Day in the Life of a Pediatric Anesthesiologist
To make this tangible, let's walk through a typical day:
6:15 AM: Arrive at the hospital. Change into scrubs, grab a coffee, and head to the preoperative holding area. Your first case is a 2-year-old scheduled for tympanostomy tube placement (ear tubes). You review their chart, noting a slight recent cold but clear lungs on examination.
6:45 AM: Meet the patient and their parents. The toddler is crying and clinging to his mom. You kneel down, speak in a calm, gentle voice, and engage him with a small toy. You explain the process to the parents in clear, reassuring terms, answering their questions about the risks and what to expect when he wakes up. You confirm he hasn't had anything to eat or drink.
7:30 AM: In the operating room. You allow one parent to accompany the child as you begin the anesthetic. You use a flavored mask to administer sevoflurane gas. As the child drifts off to sleep, the parent gives him a kiss and is escorted out. You swiftly and expertly place a small IV, secure the airway with a mask, and monitor his heart rate, blood pressure, oxygen saturation, and breathing. The surgery takes only 15 minutes.
8:00 AM: The procedure is over. You allow the child to start waking up gently and transport him to the Post-Anesthesia Care Unit (PACU). You give a detailed report to the PACU nurse and ensure the parents are called.
8:15 AM: You quickly prepare for your next case: a 10-year-old with scoliosis undergoing a complex, 6-hour spinal fusion. This is a major procedure with a high risk of blood loss. You've already placed an arterial line and a central venous line for close monitoring and fluid administration. Throughout the case, you will meticulously manage blood pressure, replace blood loss, monitor nerve function with the surgical team, and administer a sophisticated pain management plan involving both IV and regional anesthetic techniques.
2:30 PM: The scoliosis case is complete. You supervise the patient's transfer to the Pediatric Intensive Care Unit (PICU), providing a comprehensive handoff to the intensive care team.
3:00 PM - 5:00 PM: You handle a few shorter cases—a hernia repair on a 4-month-old infant, a sedated MRI for a child with a brain tumor. In between, you may be called to the emergency room to help sedate a child for a painful procedure or to the PICU to assist with a difficult intubation. Your day is a constant blend of routine and emergency, requiring rapid shifts in focus and skill.
5:30 PM: You complete your final charts, check on your post-operative patients, and hand off any ongoing responsibilities to the anesthesiologist on call for the night. You head home, knowing you've made a tangible, critical difference in the lives of several children and their families.
---
Average Pediatric Anesthesia Salary: A Deep Dive
The significant investment in time, education, and emotional energy required to become a pediatric anesthesiologist is rewarded with one of the most competitive compensation packages in the medical field. While figures vary based on numerous factors we'll explore in the next section, the earning potential is substantial from the very beginning of one's career post-fellowship.
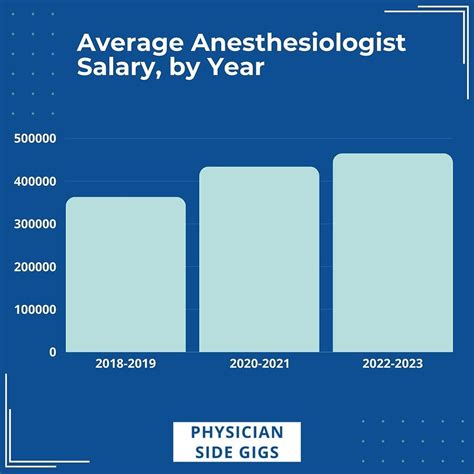
It's important to note that many salary aggregators and official sources like the U.S. Bureau of Labor Statistics (BLS) group all anesthesiologists together. However, sub-specialists like pediatric anesthesiologists typically command a salary at the higher end of that range due to their additional training and the specialized nature of their work.
### National Averages and Salary Ranges
To provide a comprehensive picture, let's look at data from several authoritative sources:
- Salary.com: As of late 2023, this platform reports the average pediatric anesthesiologist salary in the United States to be approximately $450,891. The typical range falls between $388,443 and $513,339. This represents the base salary and does not always include bonuses or other forms of compensation.
- Medscape Physician Compensation Report 2023: This highly respected industry report surveys thousands of physicians. For the general specialty of Anesthesiology, the average annual compensation was $448,000. Pediatric sub-specialists often earn slightly more, pushing them closer to the upper end of the physician pay scale.
- ZipRecruiter: This site reports a slightly lower national average of $362,607 per year, but shows a wide range, with top earners reaching $400,000+ and salaries in some locations going as high as $550,000 or more, likely reflecting total compensation packages in high-demand areas.
The key takeaway is that a starting salary for a new graduate from a pediatric anesthesia fellowship can realistically be in the $350,000 to $400,000 range, with rapid growth potential.
### Salary Progression by Experience Level
Like most professions, compensation in pediatric anesthesiology grows significantly with experience. Increased efficiency, the ability to manage more complex and higher-reimbursement cases, and the potential for leadership or partnership roles all contribute to this upward trajectory.
Here is a representative breakdown of salary expectations by career stage:
| Career Stage | Years of Experience | Estimated Annual Salary Range (Base + Bonus) | Key Drivers |
| :--- | :--- | :--- | :--- |
| Early Career | 0-4 years (Post-Fellowship) | $375,000 - $450,000 | Establishing clinical speed and proficiency; building a reputation. |
| Mid-Career | 5-15 years | $450,000 - $550,000 | Peak clinical efficiency; eligibility for partnership in private groups; taking on junior leadership roles (e.g., committee chair). |
| Senior / Late Career | 15+ years | $500,000 - $650,000+ | Department leadership (Chief of Anesthesia), partnership seniority, ownership in surgery centers, national reputation. |
*Disclaimer: These are estimated ranges based on aggregated data and can vary significantly based on the factors discussed in the next section.*
### Beyond the Base Salary: Understanding Total Compensation
A pediatric anesthesiologist's salary is just one piece of a much larger compensation puzzle. Understanding the full package is crucial when evaluating job offers.
- Bonuses: These are extremely common.
- Productivity Bonuses: Often based on Relative Value Units (RVUs), a measure of the volume and complexity of the care provided. The more cases you do and the more complex they are, the higher the bonus.
- Call Pay: Many positions offer additional stipends for being on call overnight or on weekends, which can add a significant amount ($20,000 - $100,000+ annually) to the base salary.
- Sign-On Bonuses: In-demand markets or institutions may offer substantial sign-on bonuses, ranging from $20,000 to over $100,000, to attract top talent.
- Quality Bonuses: Increasingly, compensation is tied to quality metrics like patient outcomes, safety protocols, and patient satisfaction scores.
- Profit Sharing & Partnership: In private practice, this is the single greatest driver of high-end income. After a few years as an employee, an anesthesiologist may be offered a partnership track. As a partner, they become a part-owner of the business, sharing in its profits. This can elevate total compensation well above what is achievable in an employed model.
- Retirement Benefits: Strong retirement plans are a standard part of the compensation package. This often includes a 401(k) or 403(b) with a generous employer match, and potentially a defined-benefit pension plan or cash balance plan in some practices, allowing for massive tax-deferred savings.
- Other Key Benefits:
- Malpractice Insurance: Comprehensive "claims-made" or "occurrence" malpractice coverage is always included, representing a value of $20,000-$50,000+ per year.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $5,000 - $10,000) to cover costs for conferences, journals, and courses needed to maintain medical licensure and board certification.
- Health, Dental, and Vision Insurance: Comprehensive family plans are standard.
- Relocation Assistance: A stipend to cover moving costs is often negotiable.
- Paid Time Off (PTO): Typically generous, ranging from 6 to 12 weeks per year, reflecting the high-stress nature of the job.
When considering a pediatric anesthesia salary, it is essential to look at the total value proposition. A job with a slightly lower base salary but a clear path to a lucrative partnership and excellent benefits may be far more financially advantageous in the long run than a purely salaried position with a higher initial number.
---
Key Factors That Influence Salary

While the national averages provide a useful benchmark, your actual earnings as a pediatric anesthesiologist will be determined by a complex interplay of factors. Understanding these variables is key to maximizing your income potential and making strategic career choices. This section provides an in-depth analysis of the primary drivers of salary variation.
###
Level of Education and Certification
In medicine, education is the non-negotiable foundation of earning potential. For a pediatric anesthesiologist, the pathway is long and rigorous, and each step is essential.
- The Foundational Path: The journey includes a four-year bachelor's degree, four years of medical school (earning an MD or DO), and a four-year anesthesiology residency. This is the baseline for becoming a general anesthesiologist.
- The Subspecialty Fellowship: The critical differentiator is the mandatory one-year (and sometimes two-year, for research or further specialization) fellowship in pediatric anesthesiology. This additional, highly competitive year of training is what qualifies you for the title and the associated salary premium.
- Board Certification: This is paramount for maximizing salary. To be a top earner, you must achieve board certification from the American Board of Anesthesiology (ABA) in two areas:
1. General Anesthesiology: Achieved after successfully passing written and oral exams upon completion of residency.
2. Pediatric Anesthesiology: A separate subspecialty certification achieved after completing fellowship and passing another rigorous set of exams.
Double board certification is the gold standard. It signals to employers, hospitals, and credentialing bodies that you have met the highest standards of knowledge and practice in the field, making you a more valuable and sought-after candidate. Lacking these certifications can significantly limit job opportunities and suppress earning potential.
###
Years of Experience
As illustrated in the previous section, experience is a powerful salary determinant. The growth, however, isn't just about longevity; it's about the skills and value you accumulate over time.
- 0-4 Years (The Ramp-Up Phase): Fresh out of fellowship, you are clinically proficient but still building speed and confidence in managing the most complex situations independently. Your salary is high but reflects this learning curve. In this phase, employers are investing in your potential.
- 5-15 Years (The Peak Performer): This is the sweet spot for clinical earnings. You are at your most efficient, able to handle a high volume of complex cases with expertise. In private practice, this is when you become a partner and begin to reap the financial rewards of ownership. In academic or hospital settings, you take on more responsibility, mentor junior colleagues, and may lead clinical initiatives, all of which justify a higher salary.
- 15+ Years (The Leader and Strategist): While clinical efficiency may plateau, value and salary continue to grow through leadership. This is the stage where many become the Chief of Anesthesiology, the Medical Director of the Operating Rooms, or take on significant hospital-wide administrative roles. These positions come with substantial administrative stipends on top of clinical pay. Senior partners in private groups also benefit from accumulated ownership and strategic leadership of the practice.
###
Geographic Location
Where you choose to practice has one of the most dramatic impacts on your salary. The dynamics are often counterintuitive; the most "desirable" places to live (e.g., major coastal cities) are often not the highest paying due to market saturation.
- High-Paying States and Regions: Compensation tends to be highest in states and regions that are less saturated with specialists and may have a higher demand or be considered less "popular" places to live. According to various surveys, states in the Midwest (e.g., Wisconsin, Indiana, Ohio) and some parts of the Southeast and Mountain West often offer the highest compensation packages to attract talent. For example, an anesthesiologist might earn over $500,000 in a mid-sized Midwestern city, while their counterpart in New York City or Los Angeles earns closer to $400,000 for the same work.
- Lower-Paying States and Regions: The Northeast and the West Coast tend to have lower average salaries for physicians. This is a simple function of supply and demand. Many doctors want to live in places like Boston, San Francisco, or San Diego, so hospitals and practices there do not need to offer top-tier salaries to attract a large pool of qualified applicants. Furthermore, these areas often have a higher cost of living, meaning a lower salary gets stretched even thinner.
- Rural vs. Urban: Practicing in a rural or underserved area can often lead to significantly higher income, sometimes supplemented by state or federal loan repayment programs. Hospitals in these communities must offer premium pay to entice specialists away from major metropolitan centers.
###
Practice Model (Company Type & Size)
The type of organization you work for is arguably the most significant factor influencing both your day-to-day life and your long-term earning potential.
- Academic Medical Centers:
- Salary: Typically on the lower end of the spectrum. An academic pediatric anesthesiologist at a university hospital might earn $350,000 - $450,000.
- Pros: Excellent benefits, opportunities to teach medical students and residents, dedicated time for research, access to cutting-edge cases, often a more predictable schedule with less call burden. The "currency" here is prestige and intellectual stimulation.
- Cons: Lower direct compensation, more bureaucracy, and pressure to publish or secure research funding ("publish or perish").
- Private Practice (Anesthesiology Group):
- Salary: Highest potential income. An employee of a group might start around $400,000, but a senior partner in a successful group can easily earn $600,000 - $800,000+.
- Pros: Lucrative partnership tracks where you share in the profits. More autonomy in business decisions. Often highly efficient and physician-led.
- Cons: Requires business acumen. Involves managing staff, billing, and contracts. Call burden can be heavy, and income can fluctuate with case volume and reimbursement changes. There is more personal financial risk.
- Hospital/Health System Employed:
- Salary: A solid middle ground, often ranging from $425,000 - $550,000.
- Pros: High degree of stability. You receive a steady paycheck and strong benefits without the administrative headaches of running a business. No need for a "buy-in" for partnership.
- Cons: Less autonomy. You are an employee subject to hospital administration policies. Top-end earning potential is capped compared to private practice partnership.
- Locum Tenens:
- Salary: Very high daily or hourly rates (e.g., $2,500 - $4,000+ per day), but this is pre-tax and without benefits.
- Pros: Ultimate flexibility in schedule and location. Opportunity to "test drive" different hospitals and locations.
- Cons: No job security, no paid time off, no retirement benefits, no malpractice tail coverage (you have to buy your own). Constant travel and living out of a suitcase. It's a trade-off of stability for high short-term cash flow.
###
Area of Sub-Specialization within Pediatrics
Even within the subspecialty of pediatric anesthesiology, further specialization can enhance earning potential. These "niche-within-a-niche" roles are in high demand because of the extreme level of expertise required.
- Pediatric Cardiac Anesthesiology: This is one of the highest-paid areas. These specialists handle anesthesia for surgeries to correct complex congenital heart defects in neonates and children. The cases are long, incredibly high-stress, and require a mastery of cardiac physiology and advanced monitoring techniques like transesophageal echocardiography (TEE). This expertise commands a significant salary premium.
- Pediatric Pain Management: Some pediatric anesthesiologists complete an additional fellowship in pain medicine. They manage complex chronic pain syndromes in children and perform advanced procedures like nerve blocks and spinal cord stimulator trials. This dual-specialization can open up lucrative outpatient clinic opportunities.
- Pediatric Critical Care: While less common, some anesthesiologists are also trained and board-certified in critical care medicine (intensivists). This allows them to work in the Pediatric Intensive Care Unit (PICU), managing the sickest children in the hospital. This dual skill set is highly valuable to hospitals.
###
In-Demand Skills
Beyond certifications, specific skills can make you a more valuable asset and lead to higher compensation.
- Advanced Regional Anesthesia: Proficiency in using ultrasound to perform complex nerve blocks (e.g., epidurals, spinals, peripheral nerve blocks) is highly sought after. It improves patient outcomes by reducing opioid use and providing superior pain control, which is a major priority in modern medicine.
- Leadership and Administrative Skills: The ability to lead a team, manage a budget, navigate hospital politics, and improve operating room efficiency is a ticket to the highest-paying administrative roles (e.g., Department Chair).
- Billing and Coding Expertise: Understanding the business side of medicine, specifically how to accurately document and code for the services you provide, can directly increase the revenue you generate for your group or hospital, which is often reflected in productivity bonuses.
- Exceptional Communication: While a "soft skill," the ability to communicate with anxious families, collaborate effectively with surgeons, and lead a team during a crisis is invaluable. It reduces medical errors, improves patient satisfaction, and is a hallmark of a leader.
---
Job Outlook and Career Growth

Investing over a decade in education is a significant commitment, so understanding the long-term stability and growth prospects of the profession is essential. The outlook for pediatric anesthesiologists is strong and stable, driven by fundamental, non-negotiable healthcare needs.
### Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) Occupational Outlook Handbook provides data for the broader category of "Anesthesiologists." While they don't separate out sub-specialists, the overall trends are highly relevant.
- BLS Projections (2022-2032): The BLS projects employment for all physicians and surgeons to grow by 3% over the next decade. For anesthesiologists specifically, job growth is projected to be about average, with approximately 1,300 openings projected each year, on average, over the
