Introduction

Imagine the controlled chaos of an emergency department, a symphony of beeps, hurried footsteps, and urgent voices. Now, picture that same environment scaled down for the most vulnerable of patients: children. This is the world of the Pediatric Emergency Medicine (PEM) physician, a high-stakes, high-reward career that sits at the critical intersection of emergency medicine and pediatrics. For those drawn to the profound challenge of saving young lives, the question of compensation is a practical and important consideration. A career as a pediatric ER doctor is not just a calling; it's a significant professional and financial investment, with salaries often ranging from $220,000 to well over $380,000 per year.
This role demands a unique combination of rapid-fire diagnostic skills, procedural expertise, and the gentle compassion needed to comfort a frightened child and their anxious parents. I once spent an evening in a pediatric ER with my own young son, who had a high, unrelenting fever. The calm, reassuring competence of the PEM physician not only led to a swift diagnosis but also transformed a terrifying experience into a manageable one. It was a powerful reminder that these professionals don't just treat illnesses; they restore peace of mind.
This comprehensive guide is designed to be your definitive resource on the pediatric ER doctor salary and career path. We will dissect every component of a PEM physician's compensation, explore the factors that can significantly increase your earning potential, and provide a clear, step-by-step roadmap to entering this demanding but incredibly fulfilling field.
### Table of Contents
- [What Does a Pediatric ER Doctor Do?](#what-does-a-pediatric-er-doctor-do)
- [Average Pediatric ER Doctor Salary: A Deep Dive](#average-pediatric-er-doctor-salary-a-deep-dive)
- [Key Factors That Influence a Pediatric ER Doctor's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for PEM Physicians](#job-outlook-and-career-growth)
- [How to Become a Pediatric ER Doctor: A Step-by-Step Guide](#how-to-get-started-in-this-career)
- [Conclusion: Is a Career in Pediatric Emergency Medicine Right for You?](#conclusion)
---
What Does a Pediatric ER Doctor Do?
A Pediatric Emergency Medicine (PEM) physician is a medical doctor who has undergone specialized training to care for acutely ill or injured children and adolescents in an emergency setting. They are the front-line experts for everything from a simple broken bone to life-threatening conditions like septic shock or severe trauma in patients ranging from newborns to young adults (typically up to age 18 or 21).
Their core responsibility is to rapidly assess, diagnose, stabilize, and treat a wide spectrum of pediatric emergencies. This requires a deep understanding of pediatric physiology, which differs significantly from that of adults. A child's anatomy, response to medication, and the types of illnesses they contract are all unique. A PEM physician must be adept at recognizing subtle signs of distress in a non-verbal infant or calming a terrified toddler to perform a necessary examination.
Core Responsibilities and Daily Tasks Include:
- Triage and Assessment: Working with nurses to quickly evaluate the severity of a child's condition to prioritize care for the most critical patients.
- Diagnosis: Ordering and interpreting a range of diagnostic tests, including X-rays, CT scans, ultrasounds, and laboratory work, all tailored to pediatric parameters.
- Treatment and Stabilization: Administering medications (with precise, weight-based dosing), providing respiratory support (including intubation), managing fluid and electrolyte imbalances, and treating infections.
- Performing Procedures: Executing a variety of medical procedures such as suturing lacerations, setting broken bones, draining abscesses, performing lumbar punctures (spinal taps), and inserting central lines.
- Pain and Sedation Management: Providing procedural sedation to ensure children are comfortable and still during necessary but painful procedures.
- Communication: Clearly and compassionately communicating complex medical information to worried parents or guardians, explaining diagnoses, treatment plans, and prognoses.
- Collaboration: Working closely with a team of pediatric nurses, respiratory therapists, pharmacists, and consulting with other pediatric subspecialists like cardiologists, surgeons, and neurologists.
### A Day in the Life of a PEM Physician
To make this role more tangible, consider a typical shift:
6:45 AM: Arrive at the hospital for the morning shift. You grab a coffee and head to the pediatric emergency department (ED) for "sign-out" from the overnight physician. They brief you on the current patients: a 5-year-old with an asthma exacerbation who is now stable on continuous nebulizers, a 1-week-old with a fever who is awaiting lab results for a sepsis workup, and a teenager with a fractured wrist who needs a reduction.
7:30 AM: Your first new patient arrives via ambulance. A 2-year-old is having a seizure. You immediately lead the team, calling for anti-seizure medication, checking blood sugar, and ensuring the airway is protected. The seizure stops, and you begin the diagnostic process to find the cause, all while reassuring the frantic parents.
9:00 AM: You move to the next room to see an 8-year-old who fell off his scooter. The X-ray confirms a broken arm (a distal radius fracture). You explain the need for a closed reduction to the parents and child. With the help of a nurse, you administer sedation, carefully manipulate the bone back into place, and apply a splint.
11:00 AM: The infant with the fever is back from their lumbar puncture. The initial results are reassuring, but you coordinate with the inpatient pediatric team for admission and observation, as is standard protocol for a febrile neonate.
1:00 PM: You finally have a moment to chart and grab a quick lunch. During this time, you review lab results for several other patients, including a 12-year-old with abdominal pain you suspect might be appendicitis. You call the pediatric surgery team for a consult.
3:00 PM - 6:00 PM: The afternoon rush begins. You see a succession of patients: a toddler who swallowed a coin, a 10-year-old with a severe allergic reaction, a 6-year-old with a deep cut that needs stitches, and an infant with bronchiolitis struggling to breathe. Each case requires a different set of skills, from procedural dexterity to delicate communication.
6:45 PM: The evening shift physician arrives. You provide a thorough sign-out on the remaining patients, ensuring a safe handoff of care. You leave the hospital exhausted but knowing you made a tangible difference in the lives of more than a dozen children and their families.
---
Average Pediatric ER Doctor Salary: A Deep Dive
The compensation for a Pediatric Emergency Medicine physician reflects the extensive education, specialized training, and high-stress nature of the job. While salaries can vary widely based on several factors, the earning potential is substantial.
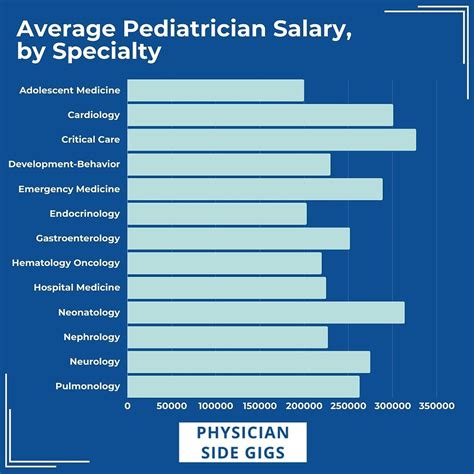
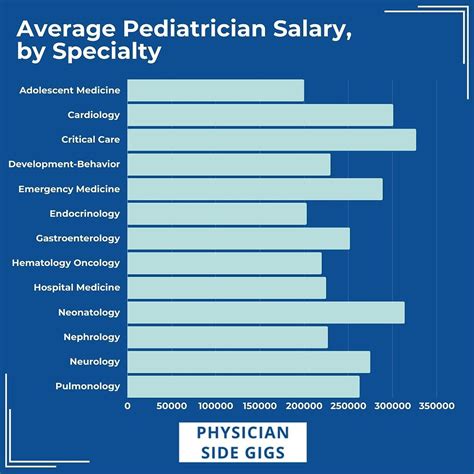
According to data from leading industry sources, the national average salary for a pediatric ER doctor in the United States typically falls between $250,000 and $300,000.
Let's break this down using recent data from authoritative sources:
- Salary.com: As of late 2023, the platform reports the average salary for a Pediatric Emergency Medicine Physician in the U.S. to be $258,800, with a typical range falling between $226,100 and $307,900.
- Medscape Physician Compensation Report 2023: While this report doesn't have a specific category for PEM, it provides excellent benchmarks. Emergency Medicine physicians reported an average income of $352,000, while Pediatricians reported $251,000. PEM physicians, as a hybrid of these specialties, generally fall somewhere within this spectrum, often landing closer to the pediatric average but with potential to earn more, especially in non-academic settings. The discrepancy highlights the significant impact of practice type on earnings.
- Doximity 2023 Physician Compensation Report: This report lists the average compensation for Emergency Medicine at $385,632 and Pediatrics at $242,834. Again, PEM physicians are a subspecialty and their earnings are influenced by which department they primarily work for (an emergency department vs. a children's hospital).
It's crucial to understand that the "average" is just a midpoint. Actual compensation can be significantly higher or lower. For example, a new graduate working in an academic center in a major metropolitan area will earn less than a 15-year veteran working for a private group in a rural area.
### Salary by Experience Level
Salary growth in medicine is directly tied to experience, reputation, and often, a transition into leadership roles. Here is a typical salary progression for a PEM physician:
| Career Stage | Years of Experience | Average Annual Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 years | $220,000 - $260,000 | Post-fellowship; typically in academic or hospital-employed roles. |
| Mid-Career | 4-10 years | $260,000 - $320,000 | Increased productivity, more experience, may take on teaching or committee roles. |
| Senior/Experienced | 11-20 years | $300,000 - $380,000 | Often in leadership positions, highly productive, well-established. |
| Late Career/Leadership | 20+ years | $330,000 - $400,000+ | Division Chief, Department Chair, Medical Director; significant administrative duties. |
*Source: Synthesized data from Salary.com, Medscape, and anecdotal reports from physician recruiting firms.*
### Beyond the Base Salary: Understanding Total Compensation
A PEM physician's salary is just one part of their overall compensation package. When evaluating a job offer, it's essential to look at the complete picture.
Key Components of a Compensation Package:
- Base Salary: The guaranteed annual income. This can be a fixed amount or an hourly rate multiplied by the number of contracted clinical hours.
- Productivity Bonuses (RVU-Based): This is a major component of compensation in many non-academic settings. Physicians earn Relative Value Units (RVUs) for each patient they see and procedure they perform. The more complex the case, the more RVUs are assigned. A bonus is often paid once a physician exceeds a certain RVU threshold. This directly rewards efficiency and seeing a higher volume of patients.
- Sign-On Bonus: Often offered to attract physicians, especially in less desirable locations or highly competitive markets. These can range from $10,000 to $50,000 or more.
- Relocation Assistance: A stipend to cover the costs of moving for a new job, typically ranging from $5,000 to $15,000.
- Retirement Benefits: This includes access to 401(k) or 403(b) retirement plans. A crucial factor is the employer's matching contribution, which can add thousands of dollars to your savings each year.
- Health and Disability Insurance: Comprehensive health, dental, and vision insurance for the physician and their family. Long-term disability and life insurance are also standard components and are critically important for protecting your income.
- Malpractice Insurance: The employer almost always covers the cost of medical malpractice insurance. It's important to know if this is "claims-made" or "occurrence" coverage, as the former may require you to purchase expensive "tail" coverage if you leave the job.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $2,000 - $5,000) to cover the costs of conferences, courses, and materials needed to maintain medical licenses and board certifications.
- Paid Time Off (PTO): Typically includes 4-6 weeks of vacation and sick leave.
When comparing two job offers, an offer with a slightly lower base salary but a generous RVU bonus structure, a high 401(k) match, and excellent benefits could be far more lucrative in the long run.
---
Key Factors That Influence a Pediatric ER Doctor's Salary
The wide salary ranges seen in the previous section are driven by a confluence of factors. Understanding these variables is key for any aspiring or practicing PEM physician looking to maximize their earning potential. This is the most critical section for truly understanding the financial landscape of this career.
###
1. Geographic Location
Where you practice is arguably the single biggest determinant of your salary as a physician. The economics of healthcare are highly localized, driven by supply and demand, cost of living, and local insurance reimbursement rates.
- High-Paying Regions: Contrary to popular belief, the highest physician salaries are often found in the Southeast and Midwest. States like Alabama, Kentucky, Oklahoma, and Indiana often offer higher compensation to attract top talent away from major coastal cities. Rural areas, in general, pay significantly more than urban centers due to a greater need and fewer physicians. According to the Medscape report, physicians in Indiana ($372,000) and Connecticut ($371,000) were among the highest earners across all specialties.
- Lower-Paying Regions: The lowest salaries are typically found in the Northeast, including states like Massachusetts, Maryland, and New York. While the cost of living in these areas is very high, a high concentration of physicians from prestigious training programs creates more competition for jobs, driving salaries down.
- Urban vs. Rural vs. Suburban:
- Urban: Major cities (New York, Boston, Los Angeles, San Francisco) tend to have lower salaries relative to the extremely high cost of living due to market saturation.
- Suburban: These areas often represent a sweet spot, with strong demand, good schools, and salaries that are competitive and go further than in a major city center.
- Rural: Offer the highest income potential due to critical shortages. A PEM physician willing to work in a rural or underserved community can often command a salary at the very top of the national range, along with significant loan forgiveness opportunities.
Example Salary Variation by City (Illustrative):
- A PEM physician in Birmingham, Alabama might earn $330,000.
- A PEM physician in Indianapolis, Indiana might earn $315,000.
- A PEM physician in Boston, Massachusetts might earn $245,000.
- A PEM physician in San Francisco, California might earn $270,000.
###
2. Type of Practice Setting
The type of institution you work for dramatically impacts your compensation structure and overall earning potential.
- Academic Medical Centers: These are university-affiliated hospitals.
- Salary: Generally on the lower end of the spectrum. The focus is on a "three-part mission": clinical care, research, and education. A portion of your time is "protected" for non-clinical academic work.
- Pros: Prestigious environment, opportunities for research and teaching, excellent benefits, often better work-life balance with less pressure on clinical volume.
- Cons: Lower base salary and bonus potential. More bureaucratic and committee-heavy.
- Community Hospitals (Hospital-Employed): These can be non-profit or for-profit hospitals not directly affiliated with a university.
- Salary: Generally in the mid-to-high range. Compensation is often heavily based on clinical productivity (RVUs).
- Pros: High earning potential for productive physicians, less pressure for academic output, often a more straightforward clinical focus.
- Cons: Can be very high-pressure environments, demanding high patient throughput. Benefits may not be as robust as in academia.
- Private Physician Groups: These are independent groups that contract their services to one or more hospitals.
- Salary: Has the highest potential income. Physicians often have the opportunity to become partners in the group after a few years.
- Pros: As a partner, you share in the group's profits, leading to very high earnings. More autonomy over practice decisions.
- Cons: Requires business acumen. Involves more financial risk and administrative responsibility (scheduling, billing, staffing). Less job security than a direct hospital employee.
- Locum Tenens: This means working as a temporary, independent contractor to fill in for physicians who are on vacation, leave, or to cover staffing shortages.
- Salary: Paid a very high hourly or daily rate (e.g., $150-$250+ per hour).
- Pros: Flexibility, high pay, ability to travel and experience different practice settings.
- Cons: No benefits (you must purchase your own health insurance, retirement plan, etc.), no paid time off, constant travel can be disruptive. Malpractice "tail" coverage is a significant consideration.
###
3. Level of Education & Board Certification
In medicine, the educational path is standardized, but certification is key.
- MD vs. DO: Both Doctor of Medicine (MD) and Doctor of Osteopathic Medicine (DO) degrees are pathways to becoming a PEM physician. There is no significant difference in salary between physicians with an MD versus a DO degree.
- Residency & Fellowship: Completing an accredited residency (in either Pediatrics or Emergency Medicine) and a subsequent fellowship in Pediatric Emergency Medicine is the standard requirement.
- Board Certification: This is a non-negotiable factor. To earn a top salary, a physician must be board-certified by the relevant medical boards. For a PEM physician, this means being certified by the American Board of Pediatrics (ABP) or the American Board of Emergency Medicine (ABEM), and then obtaining a subspecialty certification in Pediatric Emergency Medicine. Being "board eligible" (having completed training but not yet passed the exam) will result in a lower salary until certification is achieved. Maintaining this certification through continuous learning is required.
###
4. Years of Experience and Career Progression
As detailed in the table above, experience is a linear driver of salary growth.
- Early Career (Years 1-5): Focus is on building clinical speed, confidence, and efficiency. Salary growth is steady as you become a more proficient and productive clinician.
- Mid-Career (Years 6-15): This is often the period of maximum earning potential from a purely clinical standpoint. Physicians are highly efficient and may take on extra shifts. This is also when many transition into leadership.
- Leadership Roles: Taking on administrative responsibilities is a primary way to break through the typical salary ceiling. These roles come with a stipend or a higher base salary. Examples include:
- PEM Division Chief or Medical Director: Oversees the clinical operations, quality improvement, and staffing of the pediatric ED.
- Fellowship Program Director: Manages the education and training of PEM fellows.
- Director of Pediatric Ultrasound/Toxicology/Simulation: Leads a specialized program within the department.
###
5. Niche Expertise and High-Value Skills
While PEM is already a specialty, developing further niche expertise can increase your value and earning potential, primarily through opening doors to leadership roles and specialized stipends.
- Pediatric Ultrasound: Becoming an expert in point-of-care ultrasound (POCUS) is a highly valued skill that improves diagnostic accuracy and patient safety. Leading a POCUS program can come with a director stipend.
- Toxicology: Deep knowledge in pediatric toxicology is critical for managing poisonings and overdoses.
- Trauma Care: While many PEM docs manage trauma, specialized training or leadership in a hospital's pediatric trauma program is a significant value-add.
- Administrative and Business Acumen: Skills in quality improvement, patient safety, hospital finance, and operational efficiency are highly sought after for leadership positions. An MBA or MHA (Master of Health Administration) can significantly boost earning potential for those aspiring to high-level hospital administration.
- Research: In academic settings, a successful research career with grant funding can supplement a physician's salary and lead to promotion.
---
Job Outlook and Career Growth

The career outlook for physicians, in general, is stable and positive, and the specific demand for Pediatric Emergency Medicine specialists remains strong.
The U.S. Bureau of Labor Statistics (BLS) projects that employment for all Physicians and Surgeons will grow by 3 percent from 2022 to 2032, which is about as fast as the average for all occupations. This will result in about 24,000 openings each year, on average, over the decade, largely due to the need to replace workers who retire or transfer to different occupations.
While the BLS doesn't provide specific data for PEM subspecialists, several factors point to a robust job market:
1. Growing Number of Dedicated Pediatric EDs: More hospitals are recognizing the value and safety benefits of having separate, dedicated emergency departments for children staffed by PEM-trained physicians. This trend directly increases the number of available jobs.
2. Population Growth: A growing general population naturally leads to a greater need for all medical services, including emergency care for children.
3. Lack of Supply in Certain Regions: There is a significant maldistribution of PEM physicians. While major cities may have adequate staffing, there is a critical shortage in many suburban and rural communities, creating high demand and excellent job opportunities in those areas.
4. The Non-Discretionary Nature of Emergency Care: Unlike elective procedures, emergency care is a constant necessity, making the field relatively insulated from economic downturns. Children will always get sick and injured, requiring expert care regardless of the economic climate.
### Emerging Trends and Future Challenges
The field of Pediatric Emergency Medicine is not static. Aspiring and current physicians must be aware of the trends shaping its future.
Emerging Trends:
- Telemedicine: The use of telehealth for post-discharge follow-ups, minor complaint triage, and consultations with rural EDs is growing, creating new models of care.
- Point-of-Care Ultrasound (POCUS): The use of handheld ultrasound machines by the clinician at the bedside is becoming the standard of care for many procedures and diagnoses, reducing the need for radiation and speeding up dispositions.
- Focus on Physician Wellness: There is a growing and much-needed recognition of the high rates of burnout in emergency medicine. Institutions are increasingly implementing strategies to improve work-life balance, provide mental health support, and create more sustainable shift schedules.
- AI and Diagnostic Support: Artificial intelligence tools are being developed to help analyze imaging, predict patient deterioration, and streamline workflow, acting as a powerful assistant to the clinician's judgment.
Future Challenges:
- Physician Burnout: The high-stress, emotionally taxing nature of the job, combined with long hours and administrative burdens, makes burnout a significant and persistent challenge.
- Workforce Distribution: The concentration of PEM specialists in urban academic centers leaves many other communities underserved, a problem that healthcare systems are actively trying to solve.
- Increasing Patient Volumes and Acuity: Pediatric EDs are often crowded, and patients frequently present with complex medical and social needs, stretching resources thin.
### How to Stay Relevant and Advance in the Field
- Embrace Lifelong Learning: Medicine changes constantly. Staying current requires diligently completing Continuing Medical Education (CME), reading journals, and attending conferences.
- Develop a Niche: Cultivate a specific area of expertise, such as ultrasound, toxicology, medical education, or quality improvement. This makes you a more valuable asset to your institution.
- Seek Leadership Training: Take courses on leadership, management,
