Table of Contents

- [Introduction](#introduction)
- [What Does an Orthopedic Doctor Actually Do?](#what-does-an-orthopedic-doctor-actually-do)
- [The Average Salary for an Orthopedic Doctor: A Deep Dive](#the-average-salary-for-an-orthopedic-doctor-a-deep-dive)
- [Key Factors That Influence an Orthopedic Doctor's Salary](#key-factors-that-influence-an-orthopedic-doctors-salary)
- [Job Outlook and Career Growth for Orthopedic Doctors](#job-outlook-and-career-growth-for-orthopedic-doctors)
- [How to Become an Orthopedic Doctor: Your Step-by-Step Roadmap](#how-to-become-an-orthopedic-doctor-your-step-by-step-roadmap)
- [Conclusion: Is the Demanding Path Worth the Reward?](#conclusion-is-the-demanding-path-worth-the-reward)
---
Introduction

For those with a passion for human anatomy, a desire to restore function, and the fortitude for a rigorous medical journey, a career in orthopedic surgery stands as one of the most challenging and rewarding in all of medicine. It’s a field where science meets mechanics, where physicians physically rebuild the very framework of their patients' lives. But beyond the profound personal satisfaction, a pragmatic question looms large for every aspiring surgeon: What is the financial reality of this demanding profession? What is the typical salary for an orthopedic doctor?
The answer is compelling. Orthopedic surgery is consistently ranked among the highest-paying medical specialties in the United States. While the journey is long and the cost of education substantial, the potential for a seven-figure income in the later stages of a career is a tangible reality for many. The national average salary consistently hovers well above half a million dollars annually, with top earners in specialized fields and high-demand locations earning significantly more.
I still vividly remember the day my grandfather, a man who had built his life on physical labor, was told he needed a total knee replacement. The look of despair, believing his active life was over, was heartbreaking. A few months later, thanks to the incredible skill of his orthopedic surgeon, he was walking pain-free, his independence and spirit restored. That experience cemented my understanding that these doctors don't just fix bones; they restore hope, mobility, and quality of life.
This guide is designed to be your definitive resource, moving beyond a simple salary figure to provide a comprehensive, 360-degree view of the financial landscape of orthopedic surgery. We will dissect national averages, explore the critical factors that dictate your earning potential, analyze the future job market, and provide a clear roadmap for how to embark on this incredible career path. Whether you are a high school student dreaming of medical school or a medical resident contemplating a specialty, this article will equip you with the data-driven insights you need to make an informed decision.
---
What Does an Orthopedic Doctor Actually Do?

An orthopedic doctor, more formally known as an orthopedic surgeon, is a physician who specializes in the diagnosis, treatment, prevention, and rehabilitation of injuries, disorders, and diseases of the body's musculoskeletal system. This intricate system includes bones, joints, ligaments, tendons, muscles, and nerves—everything that allows you to move, work, and be active.
While the term "surgeon" brings to mind images of the operating room, surgical intervention is only one part of the job. A significant portion of an orthopedic surgeon's work is non-surgical, focusing on diagnostics and conservative treatment plans. They are master problem-solvers, acting like high-level biological mechanics for the human body.
Core Responsibilities and Daily Tasks:
- Patient Consultation & Diagnosis: The journey almost always begins in a clinical setting. Orthopedists meet with patients to discuss their symptoms, review their medical history, and perform physical examinations to assess their range of motion, stability, and sources of pain.
- Diagnostic Imaging Interpretation: They are experts in reading and interpreting X-rays, CT scans, MRIs, and ultrasounds to pinpoint fractures, arthritis, soft tissue injuries, and other musculoskeletal pathologies.
- Developing Treatment Plans: Based on their diagnosis, they create comprehensive treatment strategies. These can range from non-invasive methods like medication, physical therapy, and injections (such as corticosteroids) to surgical interventions.
- Performing Surgery: This is the most recognized aspect of their work. They perform a vast array of procedures, including:
- Joint Replacement: Replacing damaged joints (hip, knee, shoulder) with artificial implants.
- Fracture Repair: Setting broken bones using plates, screws, rods, and casts.
- Arthroscopy: Using minimally invasive camera-guided techniques to repair joint problems (e.g., ACL tears in the knee, rotator cuff tears in the shoulder).
- Spine Surgery: Performing procedures like fusions and discectomies to alleviate back pain and nerve compression.
- Soft Tissue Repair: Reconstructing torn ligaments and tendons.
- Post-Operative Care: A surgeon's job doesn't end when they leave the OR. They monitor patients' recovery, manage pain, and coordinate with physical and occupational therapists to ensure optimal rehabilitation.
- Administrative Work: Like all physicians, they spend a considerable amount of time on charting, documenting patient encounters, corresponding with other doctors, and dealing with insurance matters.
### A "Day in the Life" of an Orthopedic Surgeon
To make this tangible, consider a typical "mixed" day for an orthopedist in a private group practice:
- 6:30 AM: Arrive at the hospital for pre-operative rounds. Check on patients who had surgery yesterday, review their vitals, and speak with the nursing staff.
- 7:30 AM: First surgery of the day: a total knee arthroplasty (knee replacement). This complex procedure takes about 90 minutes.
- 9:30 AM: Second surgery: an arthroscopic repair of a torn meniscus in a young athlete. This is a quicker, minimally invasive procedure.
- 11:00 AM: Final surgery: an open reduction and internal fixation (ORIF) of a complex wrist fracture.
- 1:00 PM: A quick lunch while reviewing patient charts and signing orders.
- 1:30 PM - 5:00 PM: Head to the outpatient clinic. See a mix of post-op follow-ups, new patient consultations for back pain, and patients requiring corticosteroid injections for shoulder bursitis. In a single afternoon, they might see 20-25 patients.
- 5:00 PM - 6:30 PM: "Clean up" time. Finish patient notes, dictate operation reports, review imaging for the next day's cases, and return urgent phone calls.
- After 6:30 PM: Head home, though they may still be "on call" for emergencies from the hospital's emergency department.
This demanding schedule highlights the blend of intense, focused surgical work with the high-volume, diagnostic nature of clinical practice that defines the profession.
---
The Average Salary for an Orthopedic Doctor: A Deep Dive
When it comes to physician compensation, orthopedic surgery consistently occupies the top tier. The combination of highly specialized surgical skills, the procedural nature of the work (which is compensated at a higher rate), and high patient demand creates a powerful formula for high earning potential.
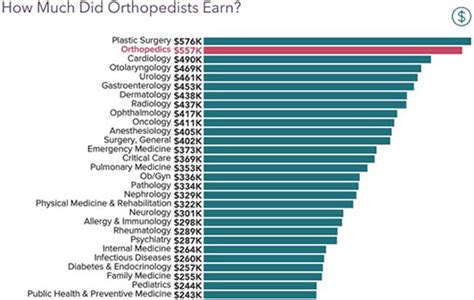
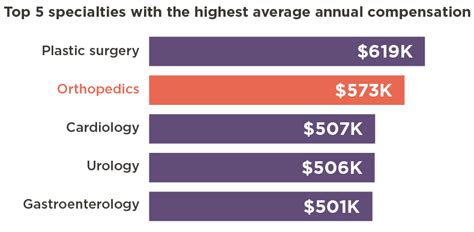
It's important to analyze data from multiple reputable sources to get a well-rounded picture, as methodologies can vary. Here is a synthesis of the most recent data on the salary for an orthopedic doctor:
- Medscape Physician Compensation Report 2023: This is one of the most widely cited reports in the industry. It places the average annual salary for orthopedic surgeons at $573,000. This figure represents a combination of salary, bonuses, and profit-sharing contributions. Notably, orthopedics was the highest-paying specialty in their 2023 survey.
- Doximity 2023 Physician Compensation Report: Another key industry report, Doximity's data shows an even higher average, reporting an average annual compensation of $624,000 for orthopedic surgeons.
- Salary.com: This aggregator provides a more granular view. As of late 2023, it reports the median salary for an Orthopedic Surgeon in the U.S. as $549,429, with a typical range falling between $431,887 and $704,818. This range excludes the top and bottom 10% of earners, highlighting the significant variance in pay.
- U.S. Bureau of Labor Statistics (BLS): The BLS groups all surgeons together under the category "Surgeons, Except Ophthalmologists." For this broader category, the median annual wage was $208,000 or greater in May 2022. The BLS often caps its upper-end data, so while it confirms a high salary, it's less specific for top-earning specialties like orthopedics.
Consensus View: Synthesizing these sources, a realistic national average for an orthopedic surgeon's total compensation is in the $550,000 to $600,000 range. However, this is just the midpoint. "Entry-level" (post-residency) surgeons might start closer to $350,000-$450,000, while experienced surgeons in lucrative subspecialties or private practice partnerships can easily surpass $1,000,000 annually.
### Salary Brackets by Experience Level
Salary progression in orthopedics is steep, rewarding the years of accumulated skill and efficiency. While residency and fellowship are periods of lower income, earnings escalate rapidly once a surgeon begins practicing independently.
| Experience Level | Typical Years of Experience | Estimated Annual Salary Range | Key Notes |
| :--- | :--- | :--- | :--- |
| Resident Physician | PGY 1-5 | $65,000 - $85,000 | Income is set by the hospital (GME funding). Increases slightly each year of residency. |
| Fellow | PGY 6-7 | $75,000 - $95,000 | A slight increase over residency pay. Focus is on subspecialty training. |
| Entry-Level (Associate) | 0-3 Years Post-Fellowship | $350,000 - $550,000 | Often starts with a guaranteed base salary plus a production bonus. Lower end is typical for academic positions. |
| Mid-Career | 4-15 Years | $500,000 - $850,000 | Base salary may decrease as production-based pay (RVUs) becomes the primary driver. Often eligible for partnership in private groups. |
| Senior / Partner | 15+ Years | $700,000 - $1,500,000+ | Peak earning years. Partnership stakes, ancillary service revenue, and surgical efficiency drive income to the highest levels. |
*Source: Data synthesized from Medscape, Doximity, and Salary.com reports, reflecting common compensation structures.*
### Breaking Down the Compensation Package
A surgeon's W-2 is more than just a base salary. Understanding the components is key to grasping the full financial picture.
- Base Salary: This is the guaranteed portion of pay, more common in hospital-employed or academic positions, and for early-career surgeons.
- Production Bonus (RVU-Based): This is the most significant part of most orthopedists' income. Compensation is tied directly to productivity, measured in Relative Value Units (RVUs). Every procedure, clinic visit, and consultation is assigned an RVU value by Medicare. The surgeon is paid a specific dollar amount per RVU generated, incentivizing efficiency and volume.
- Performance Bonuses: These can be tied to quality metrics, patient satisfaction scores, or achieving specific organizational goals.
- Partnership & Profit Sharing: In private practice, becoming a partner is a major financial milestone. Partners not only share in the surgical profits but also in revenue from ancillary services owned by the practice, such as physical therapy centers, MRI scanners, and ambulatory surgery centers (ASCs). This is often the path to the highest levels of income.
- Benefits: Comprehensive benefits packages are standard and include high-quality health, dental, and vision insurance; substantial retirement contributions (401(k) or 403(b) with generous matching); malpractice insurance (a critical and expensive component); and allowances for Continuing Medical Education (CME). The value of this benefits package can easily exceed $50,000-$100,000 annually.
---
Key Factors That Influence an Orthopedic Doctor's Salary

While the national averages are impressive, the actual salary for an orthopedic doctor is subject to immense variability. A surgeon's take-home pay is not a monolith; it's a complex equation determined by a confluence of factors. Understanding these variables is crucial for any aspiring or practicing orthopedist looking to maximize their earning potential.
###
1. Level of Education & Subspecialty Training (Fellowship)
The foundation of an orthopedic surgeon's career is a Doctor of Medicine (M.D.) or Doctor of Osteopathic Medicine (D.O.) degree, followed by a demanding five-year orthopedic surgery residency. However, in today's competitive landscape, the vast majority of residents (over 90%) go on to complete an additional one-to-two-year fellowship to sub-specialize. This decision has a profound impact on career trajectory and salary.
Certain subspecialties are more complex, involve more intricate surgeries (which are assigned higher RVUs), and are in higher demand, leading to significantly higher compensation.
Impact of Subspecialty on Average Annual Compensation:
| Subspecialty | Average Annual Salary Range | Notes on Demand and Complexity |
| :--- | :--- | :--- |
| Spine Surgery | $700,000 - $1,200,000+ | Generally the highest-paid. Involves complex, high-risk procedures with high RVU values. |
| Joint Replacement (Arthroplasty) | $650,000 - $950,000 | Very high demand due to the aging population. High-volume, efficient surgeons can be extremely productive. |
| Orthopedic Trauma | $600,000 - $900,000 | Deals with complex fractures and acute injuries. Often hospital-employed with demanding call schedules. |
| Sports Medicine | $550,000 - $800,000 | Focuses on arthroscopic procedures (knee, shoulder). High volume of younger, active patients. |
| Hand Surgery | $500,000 - $750,000 | Involves intricate, delicate procedures. Can be a mix of orthopedic and plastic surgery training. |
| Foot and Ankle Surgery | $450,000 - $700,000 | A growing field with complex reconstructive procedures. |
| Pediatric Orthopedics | $400,000 - $650,000 | Tends to be on the lower end of the orthopedic scale. Often based in academic/children's hospitals. Reimbursement rates can be lower. |
*Source: Synthesized data from various industry reports including MGMA (Medical Group Management Association) and physician recruiting firm surveys.*
Takeaway: The choice of fellowship is arguably the most significant financial decision a young orthopedic surgeon will make. Spine and joint replacement consistently lead to the highest earning potential.
###
2. Years of Experience & Career Stage
As detailed in the salary bracket table, experience is a primary driver of income. This isn't just about seniority; it's about a tangible increase in skill and efficiency.
- Early Career (Years 1-3): Surgeons are building their practice, refining their techniques, and learning the business of medicine. They are often on a guaranteed salary with a productivity bonus, as their patient volume is not yet at its peak. Their surgical times may be longer, and they are still building a referral network.
- Mid-Career (Years 4-15): This is where surgeons hit their stride. They operate with remarkable efficiency, have established referral patterns, and have often transitioned to a 100% productivity-based compensation model (RVUs). In private practice, this is the period where they become partners, significantly boosting their income through profit-sharing.
- Late Career (Years 16+): Earnings typically peak in the late 40s to late 50s. Surgeons have maximum efficiency, a stellar reputation, and a robust practice. Some may choose to scale back their surgical volume as they approach retirement, which can cause a slight dip in income, but many of the highest earners in the country are in this demographic.
###
3. Geographic Location
Where a surgeon chooses to practice has a massive impact on their salary and overall financial health. The dynamics are driven by supply and demand, cost of living, and the local insurance payor mix. Interestingly, the highest-paying areas are not always the major metropolitan centers on the coasts.
- High-Paying States/Regions: The Midwest and Southeast often offer the highest compensation for orthopedic surgeons. States like Wisconsin, Indiana, Missouri, Alabama, and Tennessee consistently appear in top-paying lists. This is due to a combination of high demand (often a shortage of specialists), a favorable malpractice insurance environment, and a lower density of surgeons, giving practices more negotiating power with insurance companies.
- Lower-Paying States/Regions: Conversely, major metropolitan areas, particularly in the Northeast and on the West Coast (e.g., New York City, Boston, Los Angeles, San Francisco), tend to offer lower compensation. This is a classic supply-and-demand issue: these desirable locations have a high concentration of surgeons, leading to more competition for patients and lower reimbursement rates from insurers. While the salary might be lower, the cost of living and running a practice in these areas is significantly higher.
According to a Doximity report, the metropolitan area with the highest average pay for orthopedic surgeons was Charlotte, NC, while the lowest was in Baltimore, MD. This illustrates the counterintuitive nature of physician geographic pay disparity.
###
4. Practice Setting & Type
The type of organization an orthopedic surgeon works for is a critical determinant of their compensation structure and ceiling.
- Private Practice (Physician-Owned): This model offers the highest earning potential.
- Solo Practice: Increasingly rare due to high overhead. Offers total autonomy but also total risk.
- Single-Specialty Group (SSG): A group of only orthopedic surgeons. This is a very common and lucrative model. It allows for cost-sharing, sub-specialization, and ownership of ancillary services (MRI, physical therapy). The path to partnership is the key to maximizing income.
- Multi-Specialty Group (MSG): A large group with physicians from many specialties (e.g., primary care, radiology, orthopedics). This provides a built-in referral network but may offer less autonomy and a slightly lower compensation ceiling than a well-run SSG.
- Hospital or Health System Employment: This is an increasingly common model, especially for new graduates. It offers stability, a predictable salary (often with a production bonus), excellent benefits, and no administrative burden of running a business. The trade-off is a lower long-term earning potential compared to a partner in a private practice. A hospital-employed surgeon may earn $500,000 - $700,000, while their private practice counterpart with ancillary revenue could be earning over $1,000,000.
- Academic Medicine: Surgeons at universities and academic medical centers are typically the lowest paid. Their compensation is a mix of clinical work, research funding, and a university salary. While the direct pay is lower (often in the $350,000 - $600,000 range), the appeal lies in teaching, research, treating complex cases, and the prestige of the institution.
###
5. In-Demand Skills & Ancillary Contributions
Beyond surgical prowess, certain skills and roles can significantly boost an orthopedist's value and income.
- Business Acumen: For those in private practice, understanding finance, marketing, operations, and negotiation is paramount. The ability to run a practice efficiently as a business is what separates high earners from average earners.
- Leadership Roles: Taking on roles like Chief of Orthopedics at a hospital, Medical Director of a surgery center, or a leadership position within a large medical group often comes with a significant stipend or salary supplement.
- Ancillary Service Development: A key driver of income in private practice is the ability to develop and own ancillary services. A practice that owns its own Ambulatory Surgery Center (ASC) allows its surgeon-partners to collect not only their professional fee for the surgery but also a share of the *facility fee*, which can dramatically increase the profitability of each case. The same applies to physical therapy, imaging centers (MRI/X-ray), and durable medical equipment (DME).
- Expert Witness & Consulting Work: Experienced surgeons with strong reputations are often sought after for legal consulting and to serve as expert witnesses in malpractice or personal injury cases. This work can be extremely lucrative, with some surgeons earning several thousand dollars per hour for their time.
---
Job Outlook and Career Growth for Orthopedic Doctors
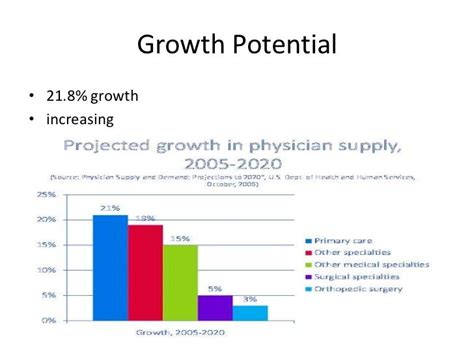
For those investing more than a decade in training, the long-term viability of their chosen profession is a critical concern. Fortunately, the career outlook for orthopedic surgeons is exceptionally strong, driven by powerful demographic and lifestyle trends.
Official Projections from the U.S. Bureau of Labor Statistics (BLS):
The BLS provides employment projections for the category "Physicians and Surgeons," which includes orthopedists. According to the latest data from the Occupational Outlook Handbook:
- Projected Growth (2022-2032): Employment for physicians and surgeons is projected to grow 3 percent over the next decade. While this may seem modest, it's about as fast as the average for all occupations. More importantly, the BLS notes that this will result in about 24,300 openings each year, on average, over the decade. Many of these openings are expected to result from the need to replace workers who transfer to different occupations or exit the labor force, such as to retire.
- Driving Factors: The BLS explicitly states that demand will stem from the "continued expansion of healthcare-related industries" and the needs of a "large and aging population."
Key Trends Fueling Demand for Orthopedic Surgeons:
1. The Aging Population: The primary driver of demand is the aging of the Baby Boomer generation. As people live longer, the incidence of age-related musculoskeletal conditions like osteoarthritis, spinal stenosis, and fragility fractures increases dramatically. Joint replacement surgery (hips and knees) is one of the most common and successful procedures performed on older adults, and the demand for these services is projected to skyrocket.
2. Active Lifestyles: Unlike previous generations, today's adults and seniors are committed to maintaining active lifestyles well into their later years. This leads to a higher incidence of sports-related injuries, overuse conditions, and a greater desire for surgical solutions that preserve mobility and function. The demand for sports medicine and arthroscopic procedures on a middle-aged population is a significant growth area.
3. Rising Rates of Obesity: The obesity epidemic in the United States places enormous stress on weight-bearing joints, particularly the knees and hips. This accelerates the development of osteoarthritis and increases the need for joint replacement surgery at even younger ages.
4. Technological and Procedural Advancements: The field of orthopedics is a hotbed of innovation.
- Robotic-Assisted Surgery: Systems like the Mako, ROSA, and VELYS robots are becoming more common for joint replacement, promising greater precision and potentially better outcomes, which attracts more patients.
- Minimally Invasive Techniques: Advances in arthroscopy and other minimally invasive approaches reduce recovery time, making surgical options more appealing to a broader range of patients.
- Biologics and Regenerative Medicine: While still evolving, the use of biologics like platelet-rich plasma (PRP) and stem cells represents a new frontier in treating certain orthopedic conditions, expanding the toolkit of the modern orthopedist.
Future Challenges and Considerations:
Despite the rosy outlook, the profession is not without its challenges. Aspiring surgeons should be aware of these trends:
- Burnout: The demands of orthopedic surgery—long hours, high-stakes procedures, and significant administrative burdens—can lead to high rates of physician burnout.
- Reimbursement Pressures: Insurance companies and government payers (Medicare/Medicaid) are constantly seeking to control healthcare costs. This can lead to declining reimbursement rates for certain procedures, forcing surgeons to increase volume to maintain their income.
- Shift to Employment: The trend of surgeons moving from private practice to hospital employment is likely to continue. While this offers stability, it may cap the earning potential that was historically possible through practice ownership.
Advice for Future-Proofing Your Career:
- Embrace Lifelong Learning: Continuously train on new technologies like robotics and novel surgical techniques.
- Develop a Niche: Sub-specializing in a high-demand area like spine or complex joint revision surgery can make you an indispensable asset.
- Cultivate Business Skills: Even if you plan to be hospital-employed, understanding the business of healthcare will help you negotiate better contracts and demonstrate your value to your employer.
- Focus on Quality Metrics: The future of compensation will be increasingly tied to patient outcomes and satisfaction scores. A reputation for excellent results will be your greatest career security.
---
How to Become an Orthopedic Doctor: Your Step-by-Step Roadmap
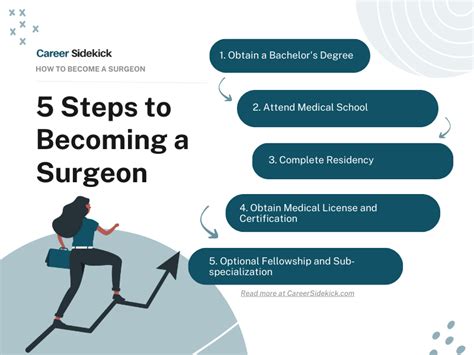
The path to becoming a board-certified orthopedic surgeon is one of the longest and most competitive in all of medicine. It requires immense dedication, academic excellence, and resilience. Here is the step-by-step journey:
Step 1: Undergraduate Education (4 Years)
- Goal: Earn a Bachelor's degree and complete all pre-medical course requirements.
- Major: While you can major in anything, common majors include biology,