Table of Contents

1. [Introduction](#introduction)
2. [What Does a Physiatrist Do? A Focus on Function and Quality of Life](#what-is-a-physiatrist)
3. [Average Physiatrist Salary: A Deep Dive into Compensation](#average-salary)
4. [Key Factors That Influence a Physiatrist's Salary](#key-factors)
5. [Job Outlook and Career Growth for Physiatrists](#job-outlook)
6. [How to Become a Physiatrist: Your Step-by-Step Career Roadmap](#how-to-become)
7. [Conclusion: Is a Career in Physiatry Right for You?](#conclusion)
---
1. Introduction
Imagine a patient whose life has been irrevocably altered. A catastrophic car accident, a debilitating stroke, a chronic condition that brings daily, searing pain. While many medical specialties focus on the immediate, life-saving intervention, who helps the patient reclaim their life *after* the crisis? Who orchestrates the complex journey back to function, independence, and an improved quality of life? This is the domain of the physiatrist, the expert physician in Physical Medicine and Rehabilitation (PM&R).
For those drawn to medicine not just to cure disease but to restore human potential, physiatry offers an incredibly rewarding path. It is a field built on resilience, collaboration, and a holistic view of the patient. Beyond its profound personal fulfillment, a career in physiatry is also financially lucrative, with a competitive salary for physiatrist professionals reflecting their extensive training and critical role in the healthcare continuum. The average annual compensation for a physiatrist in the United States consistently lands in the low-to-mid six-figure range, often exceeding $320,000, with top earners and those in specific subspecialties commanding salaries well over $400,000.
During my years analyzing healthcare careers, I once spoke with a physiatrist who described her work not as 'fixing' what was broken, but as 'rebuilding' lives, brick by brick. She recounted the story of a young musician who lost the use of her hand after a severe nerve injury, and through a combination of meticulous diagnostics, targeted injections, and a tailored therapy plan, was eventually able to play her instrument again. This powerful blend of diagnostic acumen, procedural skill, and profound human impact is the essence of this dynamic specialty.
This guide is designed to be your definitive resource on the salary for physiatrist careers. We will explore every facet of compensation, from national averages and starting salaries to the intricate factors that can significantly elevate your earning potential. We will delve into the job outlook, the required educational path, and the steps you need to take to embark on this fulfilling journey. Whether you are a pre-med student exploring specialties or a medical resident considering your future, this article will provide the authoritative, data-backed insights you need to make an informed decision.
---
2. What Does a Physiatrist Do? A Focus on Function and Quality of Life

A physiatrist, a physician specializing in Physical Medicine and Rehabilitation (PM&R), is a medical doctor who treats a wide variety of medical conditions affecting the brain, spinal cord, nerves, bones, joints, ligaments, muscles, and tendons. Unlike many other medical specialists who may focus on a single organ system, the physiatrist's focus is on a patient's whole-body function and overall quality of life. They are often called the "quality of life" physicians because their primary goal is to maximize patients' independence in activities of daily living and improve their overall well-being without surgery.
The core of physiatry is to diagnose and treat pain, restore maximum function lost through injury, illness, or disabling conditions, and provide patients with the tools they need to lead active, fulfilling lives. They are the leaders of the rehabilitation team, working closely with physical therapists, occupational therapists, speech-language pathologists, psychologists, and other medical professionals to create a comprehensive, patient-centered treatment plan.
Core Responsibilities and Daily Tasks:
A physiatrist's work is incredibly varied, spanning different settings like inpatient rehabilitation facilities, outpatient clinics, and hospitals. Their responsibilities include:
- Diagnosis: Performing detailed physical examinations and using advanced diagnostic tools like electromyography (EMG) and nerve conduction studies (NCS) to pinpoint the source of pain, weakness, or numbness. They also interpret imaging studies like X-rays, CT scans, and MRIs.
- Treatment Planning: Developing and overseeing non-surgical treatment plans tailored to each patient's specific needs and goals.
- Medical Management: Prescribing medications to manage pain, spasticity (muscle stiffness), and other symptoms related to a patient's condition.
- Therapeutic Interventions: Prescribing specific therapies, such as physical, occupational, or speech therapy, and collaborating with therapists to monitor progress.
- Interventional Procedures: Performing a range of minimally invasive procedures, such as:
- Ultrasound-guided injections into joints and soft tissues.
- Fluoroscopy-guided epidural steroid injections for back and neck pain.
- Botulinum toxin (Botox) injections for spasticity after a stroke or spinal cord injury.
- Nerve blocks and ablations.
- Patient & Family Education: Educating patients and their families about the condition, the rehabilitation process, and strategies for preventing future injuries.
- Care Coordination: Acting as the central point of contact for the rehabilitation team, ensuring all members are aligned on the treatment plan and patient goals.
### A Day in the Life of a Physiatrist (Inpatient/Outpatient Mix)
To make this tangible, let's walk through a hypothetical day for a physiatrist who splits their time between an inpatient rehabilitation facility and an outpatient clinic.
- 7:30 AM - 9:00 AM: Inpatient Rounds. Dr. Evans arrives at the inpatient rehabilitation hospital. She reviews overnight notes from nurses and begins her rounds. Her first patient is a 65-year-old man recovering from a major stroke. She assesses his motor function, checks for spasticity, adjusts his medications, and discusses his progress in physical and occupational therapy. Her next patient is a 22-year-old woman who sustained a spinal cord injury in a diving accident. Dr. Evans leads a team meeting at the bedside with the physical therapist, occupational therapist, and social worker to discuss discharge planning and adaptive equipment needs for her home.
- 9:00 AM - 12:00 PM: Outpatient Clinic. Dr. Evans moves to her outpatient clinic. Her schedule is packed with diverse cases: a 45-year-old construction worker with chronic low back pain, a 30-year-old runner with shin splints, a 58-year-old office worker with carpal tunnel syndrome, and a follow-up with a patient who received Botox injections for post-stroke spasticity. For the back-pain patient, she performs a detailed exam and orders an MRI. For the carpal tunnel patient, she performs an in-office EMG/NCS to confirm the diagnosis.
- 12:00 PM - 1:00 PM: Lunch and Administrative Time. Dr. Evans catches up on patient charting, dictates her notes from the morning, reviews lab results, and responds to messages from other physicians.
- 1:00 PM - 3:30 PM: Procedures Clinic. The afternoon is dedicated to interventional procedures. She performs three fluoroscopy-guided lumbar epidural steroid injections for patients with sciatica and two ultrasound-guided injections for patients with shoulder bursitis. These procedures require precision, a deep understanding of anatomy, and careful technique.
- 3:30 PM - 5:00 PM: Finalizing Patient Care and Documentation. Dr. Evans finishes her procedure notes, calls patients with test results, and prepares for the next day's schedule. She consults with a surgeon about a post-operative patient and provides recommendations for their rehabilitation protocol. Her day is a constant blend of hands-on patient care, diagnostic investigation, and collaborative leadership.
---
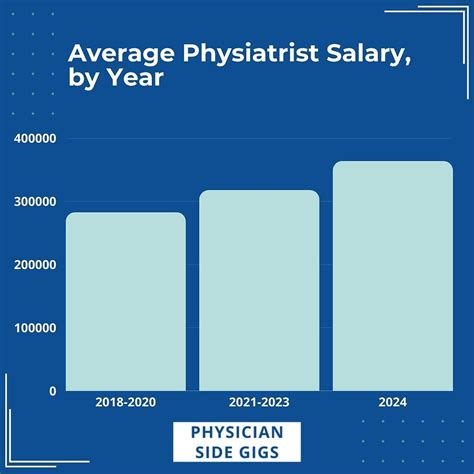
3. Average Physiatrist Salary: A Deep Dive into Compensation
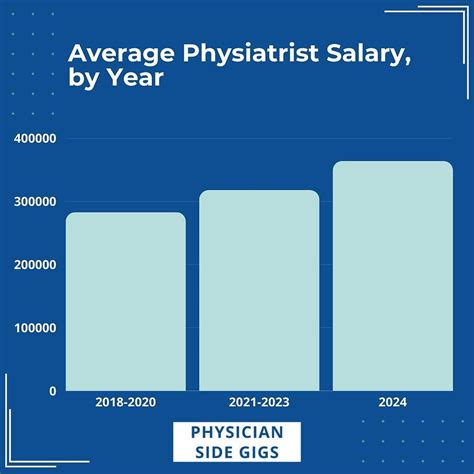
The salary for a physiatrist is a reflection of their extensive medical training, specialized skills, and the high demand for their services. Compensation in this field is robust, placing physiatrists comfortably in the upper echelon of physician earners, though typically not as high as surgical subspecialists. The data from various authoritative sources consistently shows a strong and stable earning potential.
It's important to understand that physician compensation is complex. The "salary" is often a combination of a guaranteed base salary plus productivity incentives, bonuses, and a comprehensive benefits package.
### National Average Salary and Typical Range
Multiple industry reports provide a clear picture of physiatrist earnings. Here’s a summary of the most recent data from leading sources:
- Medscape Physician Compensation Report 2023: This is one of the most respected annual surveys in the medical field. The 2023 report places the average annual salary for a physiatrist at $322,000. This report surveys thousands of physicians across the United States, providing a highly reliable benchmark.
- Doximity 2023 Physician Compensation Report: Another key industry report, Doximity's data shows an average compensation for Physical Medicine & Rehabilitation specialists at $345,752. Doximity's data is drawn from self-reported compensation surveys from over 190,000 U.S. physicians.
- Salary.com: This platform provides real-time salary data based on employer-reported information. As of late 2023, Salary.com reports the median physiatrist salary in the United States is $318,490, with a typical range falling between $288,290 and $352,690.
- Payscale: This site uses crowd-sourced data. Their figures show a slightly wider range, with an average base salary around $262,000, but this often doesn't include the significant bonuses and productivity pay common in the field.
Summary of National Averages:
| Source | Average Annual Salary | Reported Range / Notes |
| ------------------------------------- | --------------------- | -------------------------------------- |
| Medscape 2023 Report | $322,000 | Comprehensive industry survey |
| Doximity 2023 Report | $345,752 | Based on verified physician surveys |
| Salary.com (Late 2023) | $318,490 (Median) | Range: $288k - $353k |
| U.S. Bureau of Labor Statistics (BLS) | $239,200+ | Data for "Physicians & Surgeons, All Other" - Not specific to PM&R but provides a floor. |
The U.S. Bureau of Labor Statistics (BLS) does not track physiatrists as a distinct category, instead grouping them under the broad "Physicians and Surgeons, All Other" category. The median pay for this group was $239,200 per year in May 2022, but the BLS notes that wages for specialists are often much higher, aligning with the industry-specific reports.
### Salary by Experience Level
Like any profession, experience is a primary driver of salary growth. A physiatrist's earning potential increases significantly after completing residency and continues to climb as they build their reputation, expertise, and patient base.
Here is a typical salary progression based on experience, synthesized from industry data:
| Experience Level | Years of Experience | Typical Annual Salary Range | Notes |
| ----------------------- | ------------------- | --------------------------- | ---------------------------------------------------------------------------------------- |
| Entry-Level | 0-3 years | $240,000 - $290,000 | Recently completed residency. Often includes sign-on bonuses and relocation assistance. |
| Mid-Career | 4-10 years | $290,000 - $350,000 | Established practice, increased efficiency, strong referral network. |
| Senior/Experienced | 11-20+ years | $350,000 - $450,000+ | Often in leadership roles, partnership in a private practice, or a highly specialized niche. |
An entry-level physiatrist is one who has just finished their four-year residency program. Their initial offers will be on the lower end of the scale but are still exceptionally strong. These positions frequently come with attractive sign-on bonuses, which can range from $15,000 to $50,000, and relocation packages to entice new graduates to a specific hospital or practice.
A mid-career physiatrist has established themselves in their community or hospital system. They are more efficient, can handle a higher patient volume, and have built a strong referral base from primary care physicians, surgeons, and other specialists. Their compensation reflects this increased value to the practice or health system.
A senior-level physiatrist often has decades of experience and may have taken on additional responsibilities. They might be the Medical Director of a rehabilitation hospital, a partner in a lucrative private practice, or a nationally recognized expert in a subspecialty like pain medicine or brain injury. At this stage, earning potential can push well into the top tier of physician salaries.
### Beyond the Base Salary: Understanding Total Compensation
A physiatrist's offer letter is about much more than just the base salary. Total compensation is a package that includes several other valuable components.
- Productivity Bonuses: This is the most common form of additional income. Many physiatrists are paid a base salary plus a bonus based on their productivity, which is typically measured in Relative Value Units (RVUs). An RVU is a measure of value used by Medicare that factors in the time, skill, and intensity required for a patient visit or procedure. The more patients a physiatrist sees and the more procedures they perform, the more RVUs they generate, leading to a higher bonus.
- Sign-On Bonus: As mentioned, this is a one-time, lump-sum payment offered to new hires to attract them to a position. It is particularly common in areas with a high demand for physiatrists.
- Profit Sharing/Partnership Track: In private practice settings, physiatrists may have the opportunity to become a partner after a few years. As a partner, they share in the profits of the entire practice, which can significantly increase their total income but also comes with the responsibilities of business ownership.
- CME Allowance: A Continuing Medical Education (CME) allowance is standard. This provides $3,000 to $5,000 or more per year to cover the costs of attending conferences, subscribing to medical journals, and completing other educational activities required to maintain their medical license.
- Malpractice Insurance: The employer almost always covers the full cost of medical malpractice insurance, which can be a significant expense (thousands of dollars per year).
- Health and Retirement Benefits: A comprehensive benefits package including health, dental, and vision insurance, as well as a robust retirement plan (e.g., a 401(k) or 403(b) with employer matching contributions) is a standard and valuable part of the compensation package.
- Relocation Assistance: For physicians moving to a new city for a job, employers often provide a stipend of $5,000 to $15,000 to cover moving expenses.
When evaluating a job offer, it is crucial to consider the entire compensation package, as these benefits can add tens of thousands of dollars in value beyond the stated salary for a physiatrist.
---
4. Key Factors That Influence a Physiatrist's Salary
While the national average provides a useful benchmark, the actual salary for a physiatrist can vary dramatically based on a confluence of factors. Understanding these variables is crucial for anyone looking to maximize their earning potential in the field of PM&R. This section will break down the most significant drivers of compensation in detail.
### ### 1. Geographic Location
Where you practice medicine is arguably one of the most powerful determinants of your salary. This variation is driven by local market demand, cost of living, the concentration of other specialists, and state-level insurance reimbursement rates. Often, salaries are higher in less "desirable" or more rural areas where recruitment is difficult, while they may be lower in highly saturated, popular metropolitan areas.
According to the Doximity 2023 Physician Compensation Report, which provides excellent state-level data, there are clear regional trends.
Highest-Paying States/Regions:
States in the Southeast and Midwest often offer higher-than-average compensation for physicians, including physiatrists. This is due to a combination of high demand, lower physician density, and favorable practice environments. For example, states like:
- Alabama, Kentucky, Oklahoma, and Missouri consistently rank among the top for physician compensation across many specialties. A physiatrist setting up practice here might command a salary 10-20% above the national average.
- Example: A physiatrist earning the national average of $322,000 might see offers closer to $350,000 - $380,000 in these regions.
Lower-Paying States/Regions:
Conversely, states in the Northeast and some parts of the West Coast tend to have salaries that are at or below the national average, despite a higher cost of living. This is often due to a higher concentration of physicians and academic medical centers, creating a more competitive job market.
- Maryland, Massachusetts, and Rhode Island are often cited as states with lower relative physician compensation.
- Example: In a major city like Boston or Washington D.C., a physiatrist's salary might be closer to $280,000 - $310,000, which, when adjusted for the high cost of living, represents significantly less purchasing power.
Metropolitan vs. Rural:
There is a clear divide between urban and rural settings. Practices in rural or underserved areas must offer higher salaries and significant sign-on bonuses to attract qualified physiatrists. A position in rural Montana could easily pay more than a similar one in downtown San Francisco.
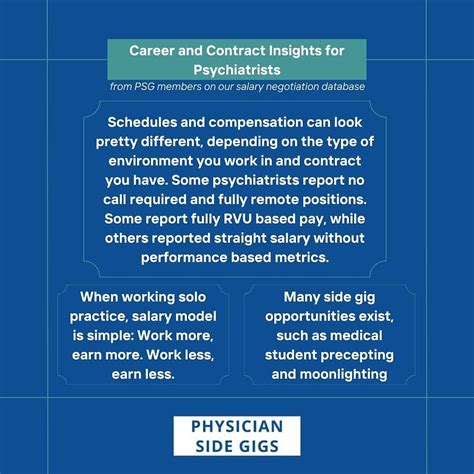
### ### 2. Practice Setting and Ownership Model
The type of organization you work for has a profound impact on your salary structure and earning potential.
- Private Practice (Physician-Owned): This setting traditionally offers the highest earning potential. After an initial period as an employee (typically 2-3 years), a physiatrist may be offered a partnership track. As a partner, you share directly in the practice's profits. This model rewards efficiency and business acumen. Top-earning physiatrists, particularly those in interventional pain, who own their practice can earn well over $500,000 to $700,000+. However, this comes with the risks and responsibilities of business ownership, including managing staff, billing, and marketing.
- Hospital or Health System Employment: This is the most common model for physicians today. It offers stability, predictable hours, and excellent benefits, including generous retirement plans and no administrative burden. The salary is typically a combination of a fixed base plus a productivity bonus. While the ceiling is generally lower than in private practice, it provides a secure and high income, often in the $300,000 to $400,000 range for an experienced physiatrist.
- Academic Medical Centers: Working at a university-affiliated hospital involves a tripartite mission: clinical care, teaching, and research. Compensation in academia is almost always lower than in private practice or general hospital employment. A physiatrist in an academic setting might earn $250,000 - $320,000. The trade-off is the prestige, the opportunity to educate the next generation of doctors, and the ability to conduct cutting-edge research.
- Inpatient Rehabilitation Facilities (IRFs): Many physiatrists work as Medical Directors or staff physicians at standalone IRFs. These roles can be very lucrative, as the physiatrist is central to the facility's operations and patient outcomes. Compensation is often high, rivaling that of hospital employment, and can be structured with significant administrative stipends and productivity bonuses.
### ### 3. Area of Subspecialty and Fellowship Training
General physiatrists have excellent earning potential, but pursuing fellowship training in a subspecialty is one of the most effective ways to significantly boost income. A fellowship is an extra 1-2 years of training after residency focused on a specific area of PM&R.
- Interventional Pain Medicine: This is, by far, the most lucrative PM&R subspecialty. After a one-year, highly competitive fellowship, these physiatrists are experts in advanced, minimally invasive procedures to treat chronic pain (e.g., spinal cord simulators, epidural injections, radiofrequency ablations). Due to the high reimbursement rates for these procedures, an interventional pain physiatrist in private practice can easily earn $500,000 to over $1,000,000 annually.
- Spinal Cord Injury (SCI) Medicine: This fellowship focuses on the complex care of patients with spinal cord injuries. Physiatrists in this field are in high demand and often work as directors of SCI units in major rehabilitation hospitals. Their specialized expertise commands a premium salary, often 10-15% higher than a general physiatrist.
- Brain Injury Medicine (TBI): Similar to SCI, this subspecialty focuses on patients recovering from traumatic brain injuries. These experts are critical in inpatient and outpatient settings, and their specialized knowledge leads to higher compensation packages, typically in the $340,000 - $400,000 range.
- Sports Medicine: A PM&R-trained sports medicine physician focuses on non-operative musculoskeletal injuries in athletes and active individuals. They perform many ultrasound-guided procedures and often work with sports teams. Their earning potential is strong, generally higher than general PM&R, particularly if they incorporate regenerative medicine techniques.
- Pediatric Rehabilitation: This subspecialty focuses on children with conditions like cerebral palsy, spina bifida, and muscular dystrophy. While incredibly rewarding, it is typically one of the lower-paying PM&R subspecialties, often aligning more with general pediatric specialist salaries.
### ### 4. Procedural Skills and In-Demand Expertise
Regardless of subspecialty, the more procedures a physiatrist can perform, the higher their earning potential. Compensation models are heavily weighted towards procedures over cognitive-based "evaluation and management" services.
High-Value Skills That Boost Salary:
- Electromyography (EMG) / Nerve Conduction Studies (NCS): Proficiency in these diagnostic tests is a core skill that adds significant value (and revenue) to a practice.
- Ultrasound Guidance: Using ultrasound for injections (e.g., into joints, tendons, and around nerves) is now