Introduction: The Unseen Guardians of Healthcare
In the complex and often chaotic world of healthcare, there exists a group of highly specialized professionals who act as silent guardians. They are the detectives, the educators, and the strategists working tirelessly behind the scenes to protect every single patient and healthcare worker from the invisible threat of infection. These individuals are Infection Preventionists (IPs), and they are among the most critical and increasingly valued experts in modern medicine.
If you are drawn to a career that combines clinical knowledge with analytical problem-solving, a deep sense of purpose with tangible impact, and offers substantial financial rewards, then the role of an Infection Preventionist might be your calling. This is a field where your work directly translates into saved lives, reduced healthcare costs, and a safer environment for everyone. The salary of an infection preventionist reflects this immense responsibility, with experienced and certified professionals commanding six-figure incomes and enjoying a robust career outlook.
I remember visiting a family member in an intensive care unit several years ago. I was struck not by the advanced machinery, but by the meticulous, almost ritualistic, adherence to protocols—the hand hygiene stations, the specific gowns and gloves for entering the room, the constant environmental cleaning. It was only later, when I delved into the world of healthcare management, that I realized this symphony of safety wasn't accidental; it was orchestrated by an Infection Preventionist, a dedicated expert whose entire job was to keep my loved one safe from a secondary illness.
This guide is designed to be your definitive resource for understanding this vital career. We will delve into every facet of the profession, from the daily responsibilities to a comprehensive breakdown of salary expectations, the factors that can significantly increase your earning potential, and a step-by-step roadmap to launching your own career as a guardian of health.
### Table of Contents
- [What Does an Infection Preventionist Do?](#what-does-an-infection-preventionist-do)
- [Average Infection Preventionist Salary: A Deep Dive](#average-infection-preventionist-salary-a-deep-dive)
- [Key Factors That Influence an Infection Preventionist's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion: Is a Career in Infection Prevention Right for You?](#conclusion)
What Does an Infection Preventionist Do?
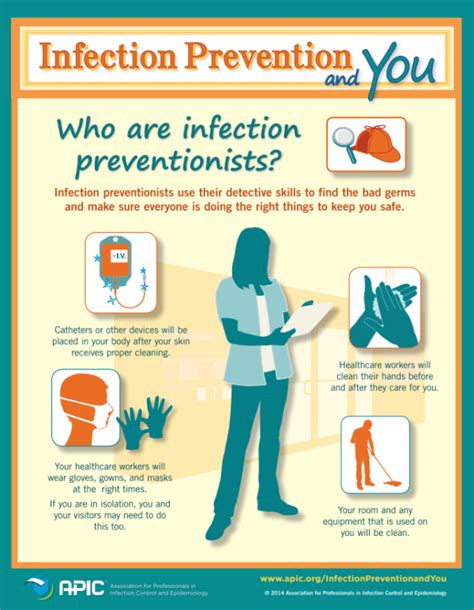
At its core, an Infection Preventionist is a healthcare professional responsible for preventing and controlling the spread of Healthcare-Associated Infections (HAIs). This is a broad mandate that encompasses a fascinating blend of scientific investigation, education, policy development, and data analysis. IPs are the linchpin of a healthcare facility's safety program, collaborating with everyone from frontline nurses and physicians to environmental services staff and executive leadership.
Their work is grounded in the principles of epidemiology—the study of how diseases spread and can be controlled. They use this knowledge to identify risks, investigate outbreaks, and implement evidence-based strategies to mitigate threats.
Core Roles and Responsibilities Include:
- Surveillance: This is the cornerstone of the IP role. They systematically collect, analyze, and interpret health data on infections within the facility. This involves tracking rates of specific HAIs like Central Line-Associated Bloodstream Infections (CLABSIs), Catheter-Associated Urinary Tract Infections (CAUTIs), Surgical Site Infections (SSIs), and multi-drug resistant organisms (MDROs) like MRSA.
- Outbreak Investigation: When a potential outbreak is detected (e.g., a sudden cluster of influenza cases on a specific unit), the IP becomes a detective. They work to identify the source of the infection, determine how it is spreading, and implement immediate control measures to contain it.
- Policy and Procedure Development: IPs develop, review, and update institutional policies and procedures based on the latest scientific evidence and regulatory guidelines from organizations like the Centers for Disease Control and Prevention (CDC) and The Joint Commission. These policies cover everything from hand hygiene and personal protective equipment (PPE) use to sterile processing and environmental disinfection.
- Education and Training: A policy is only as effective as its implementation. A huge part of an IP's job is educating all levels of staff on infection control principles. This can range from new employee orientation to just-in-time training on a new piece of equipment or a specific isolation protocol.
- Compliance and Reporting: IPs ensure the facility adheres to local, state, and federal regulations regarding infection control. They are responsible for reporting specific communicable diseases to public health authorities and preparing data for mandatory public reporting initiatives.
- Consultation: They serve as the go-to expert for the entire organization on matters of infection prevention. This can involve advising on the purchase of new medical equipment, providing input on construction and renovation projects to ensure they are designed safely, and consulting on individual patient cases with complex infectious diseases.
### A Day in the Life of an Infection Preventionist
To make this role more tangible, let's walk through a hypothetical day for "Maria," an IP at a 300-bed community hospital.
- 8:00 AM - 9:30 AM: Morning Surveillance & Rounds: Maria starts her day by reviewing microbiology lab reports from the last 24 hours, flagging any significant positive cultures (like MRSA or C. difficile). She cross-references these with patient charts in the Electronic Health Record (EHR) to determine if they represent new HAIs. She then performs rounds on key units like the ICU and the oncology floor, observing practices, checking in with charge nurses about any concerns, and ensuring patients in isolation are being cared for correctly.
- 9:30 AM - 11:00 AM: Data Analysis & Reporting: Back at her desk, Maria enters the new HAI data into her surveillance software. She analyzes the monthly CLABSI rate for the ICU, noting a slight upward trend. She begins preparing charts and a brief report for the upcoming ICU Quality Committee meeting to discuss potential causes and interventions.
- 11:00 AM - 12:00 PM: Outbreak Huddle: The charge nurse from the surgical unit calls Maria. Three post-operative patients on the floor have developed similar-looking rashes. Maria immediately convenes a huddle with the unit's nurse manager and a hospitalist physician. They review the cases, take photos of the rash, and initiate an investigation, starting with a review of all common products used on the patients, from skin preps to dressings.
- 1:00 PM - 2:30 PM: Staff Education: Maria heads to the medical-surgical unit to conduct a scheduled training session. Today's topic is proper donning and doffing of PPE for C. difficile rooms. She uses a hands-on demonstration and a Q&A session to ensure the nursing staff feels confident and competent.
- 2:30 PM - 4:00 PM: Construction Meeting: The hospital is planning to renovate a patient care unit. Maria meets with the facilities manager, architects, and construction foreman. She reviews the blueprints and provides critical input on setting up proper dust barriers, managing airflow (negative pressure), and a plan for terminal cleaning before the unit reopens to patients. Her input is vital to prevent construction-related fungal infections.
- 4:00 PM - 5:00 PM: Follow-up and Planning: Maria follows up on the rash investigation, sending a summary to the Director of Nursing. She finishes her report for the ICU meeting and responds to a dozen emails that came in throughout the day. Before leaving, she reviews her calendar for tomorrow, which includes a meeting with the hospital's new antibiotic stewardship pharmacist and a policy review session.
This "day in the life" illustrates the dynamic, multi-faceted nature of the job. It requires a unique ability to switch between deep analytical work, hands-on clinical observation, and high-level strategic planning, all within a single day.
---
Average Infection Preventionist Salary: A Deep Dive
One of the most compelling aspects of a career in infection prevention is the strong compensation package, which reflects the high level of expertise and critical importance of the role. The salary for an infection preventionist is not only competitive but also shows significant potential for growth with experience, certification, and specialization.
It's important to note that salary data can vary slightly between sources due to different methodologies, but they all paint a similar picture of a lucrative career path.
National Averages and Typical Salary Ranges
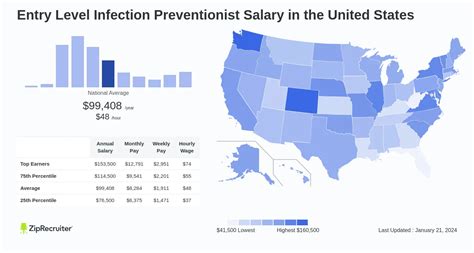
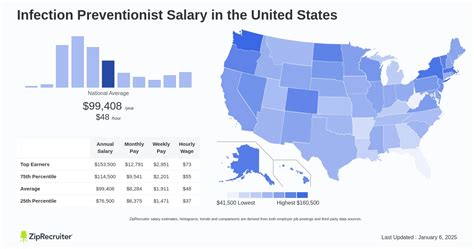
According to several reputable sources, the national average salary for an Infection Preventionist in the United States falls comfortably in the high five-figure to low six-figure range.
- Salary.com: As of late 2023, the median annual salary for an Infection Preventionist is $99,575. The typical salary range falls between $88,582 and $111,260. This range represents the middle 50% of earners, with the top 10% of IPs earning over $121,500 and the bottom 10% earning under $79,600.
- Payscale.com: This source reports a slightly lower average base salary of around $82,135 per year. However, it also highlights a wide range, from $63,000 for entry-level positions to $114,000 for experienced professionals. Payscale also notes that bonuses can add up to $10,000 to the annual compensation.
- Glassdoor: Based on user-submitted data, Glassdoor reports an estimated total pay of $111,833 per year in the United States, with an average base salary of $98,245. The "likely range" for total pay is between $92,000 and $136,000.
Summary of National Salary Data:
| Data Source | Average Base Salary | Typical Salary Range |
| :--- | :--- | :--- |
| Salary.com | $99,575 | $88,582 - $111,260 |
| Payscale.com | $82,135 | $63,000 - $114,000 |
| Glassdoor | $98,245 | $92,000 - $136,000 (Total Pay) |
Taking these sources together, a reasonable expectation for a mid-career Infection Preventionist is a base salary in the $90,000 to $110,000 range, with significant upward potential.
### Salary Progression by Experience Level
Like most professions, compensation in infection prevention grows substantially with experience. As you develop a deeper understanding of surveillance, gain expertise in managing complex outbreaks, and take on leadership responsibilities, your value to an organization—and your salary—increases.
Here is a breakdown of typical salary brackets based on career stage:
| Experience Level | Years of Experience | Typical Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level / IP Trainee | 0-2 Years | $70,000 - $85,000 | Often a registered nurse or public health professional new to the field. Works under the close supervision of a senior IP. Focuses on learning surveillance techniques and basic policies. |
| Mid-Career / IP II | 2-5 Years | $85,000 - $105,000 | Has a solid grasp of core IP functions. Often has or is preparing for CIC® certification. Manages surveillance for specific units and assists with education and smaller projects independently. |
| Senior / Lead IP | 5-10 Years | $100,000 - $125,000 | Almost always CIC® certified. Serves as a subject matter expert, leads complex outbreak investigations, mentors junior IPs, and takes charge of major initiatives like policy overhauls or new program implementation. |
| Manager / Director of Infection Prevention | 10+ Years | $120,000 - $160,000+ | Manages the entire Infection Prevention department and team of IPs. Responsible for the strategic direction of the program, budget management, high-level reporting to executive leadership, and representing the hospital in system-wide or community initiatives. |
*Note: These ranges are estimates and can be influenced by the other factors discussed in the next section.*
### Beyond the Base Salary: Understanding the Full Compensation Package
Your total compensation is more than just your annual salary. When evaluating a job offer, it's crucial to consider the entire package, which often includes:
- Bonuses: Many hospitals and healthcare systems offer annual performance-based bonuses. For an IP, these might be tied to achieving specific targets, such as reducing the rate of a particular HAI by a certain percentage. As noted by Payscale, these bonuses can add a significant amount to your yearly earnings.
- On-Call Pay: Some smaller facilities may only have one or two IPs, requiring them to be on-call for after-hours emergencies or outbreak consultations. This is typically compensated with an on-call stipend and/or hourly pay if called in.
- Retirement Savings Plans: This is a key component of long-term financial health. Most healthcare organizations offer a 401(k) or 403(b) plan, often with a generous employer match (e.g., matching 50% or 100% of your contributions up to a certain percentage of your salary).
- Health and Wellness Benefits: Comprehensive health, dental, and vision insurance are standard. Many employers also offer wellness programs, gym memberships, and mental health support.
- Paid Time Off (PTO): This includes vacation days, sick leave, and paid holidays. The amount of PTO typically increases with years of service.
- Professional Development Funds: This is a particularly valuable benefit for IPs. Many employers will pay for the costs associated with obtaining and maintaining the crucial CIC® certification, as well as covering registration and travel fees for attending major professional conferences like the annual APIC conference. This investment in your growth is a significant financial perk.
When considering a role, always look at the value of these benefits in addition to the base salary. A job with a slightly lower base but an excellent retirement match and full funding for professional development might be a better long-term financial choice.
---
Key Factors That Influence an Infection Preventionist's Salary
While the national averages provide a solid baseline, your individual salary as an Infection Preventionist will be determined by a combination of several key factors. Understanding these variables is the first step to maximizing your earning potential throughout your career. This section provides an in-depth look at the six primary drivers of an IP's salary.
### 1. Education and Professional Certifications
Your educational background and, most importantly, your professional certifications are arguably the most significant determinants of your starting salary and long-term earning power.
Educational Background:
The minimum educational requirement for most IP positions is a bachelor's degree. The specific field of study can vary, but the most common and sought-after backgrounds are:
- Bachelor of Science in Nursing (BSN): This is the most traditional pathway. An RN background provides a strong clinical foundation, immediate credibility with nursing staff, and a deep understanding of patient care workflows. Many IP job descriptions list an RN license as a requirement or strong preference.
- Bachelor's Degree in a Health Science Field: Degrees in Public Health, Microbiology, Epidemiology, or Medical Laboratory Science are also excellent foundations. These candidates bring strong scientific and analytical skills to the role.
While a bachelor's degree is the entry point, pursuing a Master's degree can provide a substantial salary boost and open doors to leadership positions. The most relevant advanced degrees are:
- Master of Public Health (MPH): An MPH with a concentration in epidemiology or infectious diseases is highly valued. It provides advanced training in biostatistics, surveillance methods, and population health, which are directly applicable to the IP role.
- Master of Science in Nursing (MSN): For RNs, an MSN (particularly in a leadership or public health track) demonstrates a commitment to advanced practice and can be a prerequisite for director-level roles.
An IP with a Master's degree can often command a salary that is 10-15% higher than a counterpart with only a bachelor's degree, all other factors being equal.
The Power of Certification: The CIC®
If there is one single thing you can do to maximize your salary as an IP, it is to earn the Certification in Infection Control and Epidemiology (CIC®).
- What it is: The CIC® is the gold-standard credential for Infection Preventionists, administered by the Certification Board of Infection Control and Epidemiology (CBIC). It validates that an individual has met a standard of knowledge and competence in the field.
- Why it Matters: Earning the CIC® is a clear signal to employers that you are a dedicated expert. It demonstrates mastery of a broad body of knowledge, from surveillance and epidemiology to sterilization and environmental hygiene.
- The Salary Impact: The impact of CIC® certification on salary is significant and well-documented. Numerous industry surveys have shown that certified IPs earn, on average, $15,000 to $20,000 more per year than their non-certified peers. Many job postings for mid-career and senior-level positions list CIC® certification as a mandatory requirement.
Other relevant certifications, such as the Long-Term Care Certification in Infection Prevention (LTC-CIP) for those specializing in nursing homes, can also enhance your expertise and marketability within a specific niche.
### 2. Years of Experience
As detailed in the previous section, experience is a primary driver of salary growth. The trajectory is clear and rewarding.
- 0-2 Years (Entry-Level): At this stage, you are learning the ropes. Your salary reflects your trainee status. Your focus should be on absorbing as much knowledge as possible and preparing for your CIC® exam.
- 2-5 Years (Mid-Career): You have moved from trainee to competent practitioner. You can work independently and are a reliable resource for your assigned areas. This is typically when you earn your CIC®, leading to a significant salary jump. According to Salary.com, an Infection Preventionist I (1-3 years experience) earns around $91,000, while an Infection Preventionist II (3-5 years) earns closer to $100,000.
- 5-10 Years (Senior/Lead): You are now a seasoned expert. You lead complex projects, mentor others, and have deep institutional knowledge. Your salary moves well into the six-figure range ($100,000 - $125,000). You may take on "lead" responsibilities even without a formal management title.
- 10+ Years (Management/Director): With a decade or more of experience, you are qualified for leadership roles. As a Manager or Director, you oversee a team and the entire program's strategy. This shift into management comes with a substantial increase in responsibility and compensation, often reaching $130,000 to $160,000 or more, especially in large, complex health systems.
### 3. Geographic Location
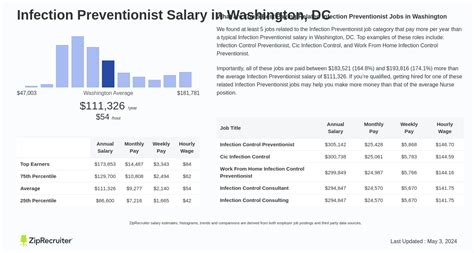
Where you work has a massive impact on your paycheck. Salaries are adjusted based on the local cost of living, demand for healthcare professionals, and the concentration of large, high-paying medical institutions.
High-Paying States and Metropolitan Areas:
Generally, states with a high cost of living and large, urban medical centers offer the highest salaries.
- Top Paying States for Infection Preventionists:
1. California: Cities like San Francisco, San Jose, and Los Angeles consistently offer the highest salaries, often 15-25% above the national average.
2. New York: Particularly in the New York City metropolitan area.
3. Washington: Driven by the Seattle metro area's thriving healthcare and tech sectors.
4. Massachusetts: Home to world-renowned academic medical centers in Boston.
5. Alaska: High salaries are common across many professions to compensate for the high cost of living and remote location.
For example, data from Zippia shows the average IP salary in California is over $119,000, while in Washington it is over $111,000.
Lower-Paying States:
Conversely, states in the Southeast and parts of the Midwest tend to have lower costs of living and, consequently, lower average salaries. States like Alabama, Arkansas, Mississippi, and Oklahoma often have salaries that are 10-20% below the national average. However, the purchasing power of that salary may be equivalent to or even greater than a higher salary in an expensive coastal city.
### 4. Work Setting and Employer Type
The type of facility you work for plays a significant role in your compensation and day-to-day responsibilities.
- Large Academic Medical Centers / Hospital Systems: These are typically the highest-paying employers. They are often unionized, have structured salary scales, and require IPs to manage highly complex patient populations (e.g., transplant, trauma, burn units). The work is demanding but comes with top-tier pay and benefits. A Director of IP at a major academic center could earn upwards of $180,000.
- Community Hospitals: These facilities offer competitive salaries, often right around the national average. The work environment may be less complex than at a major academic center, offering a different kind of work-life balance. An IP might be the sole practitioner or part of a small team, providing a broad range of experience.
- Long-Term Care (LTC) / Skilled Nursing Facilities (SNFs): The demand for IPs in LTC has exploded, especially since the COVID-19 pandemic. A federal mandate now requires all SNFs to have a dedicated, specialized IP. Salaries in this sector have become increasingly competitive, often matching or exceeding those in community hospitals, especially for those with the LTC-CIP certification. Corporate LTC chains may have regional IP consultant roles that are very well-compensated.
- Ambulatory / Outpatient Surgery Centers: As more procedures move to the outpatient setting, the need for skilled IPs is growing. Salaries are generally competitive, and the work often offers a more predictable schedule with no weekend or on-call duties.
- Public Health Departments: Working for a city, county, or state health department offers a different focus. You might be involved in community-wide outbreak investigations, policy development, and public health preparedness. Government salaries may be slightly lower than in the private sector, but they often come with excellent benefits, job security, and a strong pension plan.
- Corporate / Industry Roles: IPs can also work for medical device manufacturers, pharmaceutical companies, or consulting firms. These roles might involve advising on product design, developing educational materials, or consulting with multiple hospitals. These corporate positions can be among the most lucrative, but they often require significant experience and a strong business acumen.
### 5. Area of Specialization
While "Infection Preventionist" is already a specialty, you can develop sub-specializations that make you more valuable. This is less about a formal title and more about cultivating a unique expertise.
- Data Analytics and Informatics: IPs who are highly skilled in using surveillance software (like NHSN, TheraDoc, or MedMined), biostatistics, and data visualization tools are in high demand. The ability to not just collect data, but to turn it into compelling, actionable insights for leadership is a highly paid skill.
- High-Consequence Infectious Diseases / Emergency Preparedness: IPs who specialize in preparing for and managing rare but dangerous pathogens (like Ebola or MERS) are critical assets to hospitals. They lead drills, write comprehensive plans, and are the calm, expert voice in a crisis.
- Construction and Renovation: An IP with deep expertise in managing infection control risk during healthcare construction (known as ICRA) is invaluable. This specialized knowledge can prevent devastating outbreaks and is highly sought after by large facilities undergoing expansion.
- Sterile Processing and High-Level Disinfection: Expertise in the intricate processes of sterilizing surgical instruments and endoscopes is a critical and highly technical niche. An IP who is an expert in this area can prevent surgical site infections and other procedural HAIs.
- Pediatrics or Oncology: Working with vulnerable populations like neonates, children, or immunocompromised cancer patients requires specialized knowledge and protocols. IPs with experience and expertise in these areas are essential for children's hospitals and cancer centers.
### 6. In-Demand Skills
Beyond your formal qualifications, possessing a specific set of soft and hard skills can directly impact your salary negotiations and career progression.
- Leadership and Influence: The best IPs are leaders who can influence change without direct authority. They build relationships, communicate effectively, and persuade staff at all levels to adopt safer practices.
- Communication and Education: You must be able to explain complex scientific concepts to diverse audiences—from surgeons to housekeeping staff—in a way that is clear, compelling, and non-punitive.
- Critical Thinking and Problem Solving: When an outbreak occurs, you need to think like a detective, systematically analyzing clues and ruling out possibilities to find the root cause.
- Regulatory Knowledge: A deep and up-to-date understanding of regulations and standards from The Joint Commission, CMS, OSHA, and the CDC is non-negotiable and a core competency.
- Project Management: Implementing a new hospital-wide hand hygiene campaign or rolling out a new disinfection product is a major project. Skills in planning, execution, and measuring outcomes are essential.
*