Introduction

Have you ever wondered what it takes to hold a human life—and the very essence of their consciousness—in your hands? For neurosurgeons, this is not a philosophical question; it is the daily reality of their profession. Operating on the intricate and delicate structures of the brain, spine, and nervous system, they stand at the pinnacle of medical practice. This career path is renowned for its immense challenges, years of rigorous training, and profound responsibility. It is also, deservedly, one of the most financially rewarding professions in the world. The salary of a neurosurgeon often reaches into the high six or even seven figures, a reflection of the unparalleled skill, dedication, and stakes involved.
For anyone aspiring to this elite field, or simply curious about its rewards, understanding the financial landscape is crucial. A neurosurgeon’s compensation isn't a single, simple number; it's a complex equation influenced by experience, location, practice type, and specialization. While national averages often cite figures between $600,000 and $900,000 annually, the full spectrum can range from a resident's modest stipend to well over $2 million for a top-tier private practitioner.
I once spoke with the daughter of a patient who underwent a complex surgery to remove a tumor from her spinal cord. She described watching her father, who had been progressively losing his ability to walk, take his first unaided steps just weeks after the procedure. The look of awe and gratitude on her face as she spoke of the neurosurgeon was a powerful reminder that behind the staggering salaries and long hours lies a fundamental, life-altering purpose.
This comprehensive guide will demystify the salary of a neurosurgeon, providing an authoritative, data-driven look into every facet of their compensation. We will explore not only *what* they earn but *why* they earn it, the long road required to get there, and the future outlook for this demanding and esteemed profession.
### Table of Contents
- [What Does a Neurosurgeon Do?](#what-does-a-neurosurgeon-do)
- [Average Neurosurgeon Salary: A Deep Dive](#average-neurosurgeon-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Neurosurgeon Do?

A neurosurgeon is a highly specialized medical doctor (M.D. or D.O.) who diagnoses and surgically treats disorders of the central and peripheral nervous systems. This includes the brain, spinal cord, skull, and the vast network of nerves that extend throughout the body. While the term "surgeon" evokes images of the operating room, a significant portion of a neurosurgeon's work involves non-operative management and diagnosis.
Their responsibilities are vast and require a profound understanding of anatomy, physiology, and pathology. They manage a wide range of conditions, including:
- Trauma: Head injuries, spinal cord injuries, and nerve damage from accidents.
- Tumors: Benign and malignant growths in the brain and spine (neuro-oncology).
- Vascular Disorders: Aneurysms, blood clots, strokes, and arteriovenous malformations (AVMs).
- Degenerative Diseases: Herniated discs, spinal stenosis, and other conditions causing chronic back and neck pain.
- Pediatric Conditions: Congenital malformations like spina bifida, hydrocephalus, and pediatric brain tumors.
- Functional Disorders: Movement disorders like Parkinson's disease, epilepsy, and chronic pain syndromes, which can sometimes be treated with procedures like deep brain stimulation (DBS) or nerve ablation.
- Infections: Brain or spinal abscesses and other infections affecting the nervous system.
The core duties of a neurosurgeon extend far beyond the operating table. They meticulously review patient histories, interpret complex imaging studies like MRIs and CT scans, perform neurological exams, and develop comprehensive treatment plans. These plans may or may not involve surgery. Many patients with back pain, for instance, are managed with physical therapy, medication, or injections, with surgery being the last resort.
### A Day in the Life of a Neurosurgeon
To truly grasp the intensity of the role, consider a typical (though no two days are alike) day for a hospital-employed neurosurgeon:
- 5:30 AM - Morning Rounds: The day begins before sunrise. The neurosurgeon visits post-operative patients and those currently admitted to the neuro-intensive care unit (ICU). They review overnight progress, check vital signs and neurological function, analyze new imaging, and adjust treatment plans with the resident and nursing teams.
- 7:30 AM - Pre-Operative Consultation: Meet with the first surgical patient of the day and their family. They review the plan for the surgery—a multi-hour procedure to resect a brain tumor—reconfirm consent, and answer any last-minute questions, providing reassurance and managing expectations.
- 8:00 AM - Surgery: The main event. The neurosurgeon, leading a team of residents, anesthesiologists, and nurses, begins the delicate and mentally taxing procedure. This requires immense focus, precision, and the ability to adapt to unexpected findings. A complex tumor removal can last anywhere from 4 to 12 hours or more.
- 4:00 PM - Post-Operative Work: After the surgery, the neurosurgeon dictates the operative notes, writes post-op orders for the patient's care in the ICU, and meets with the family to update them on the outcome.
- 5:00 PM - Afternoon Clinic: The day isn't over. They head to their outpatient clinic to see patients for consultations, follow-up appointments, and pre-surgical evaluations. This involves breaking difficult news, explaining complex conditions, and building rapport with patients and their families.
- 7:00 PM - Administrative Tasks & Research: The clinical work may be done, but there are still charts to complete, emails to answer, and calls to return. If they work in an academic center, they may also dedicate time to research, writing papers, or preparing lectures.
- 8:00 PM (and beyond) - On Call: Many neurosurgeons are part of an on-call rotation for emergency trauma cases. A call from the ER at 10 PM about a patient with a severe head injury from a car accident means heading back to the hospital for an emergency craniotomy that could last all night.
This schedule illustrates the extraordinary commitment required. It's a profession that demands not just intellectual and technical brilliance, but also physical stamina and emotional resilience.
Average Neurosurgeon Salary: A Deep Dive
The compensation for a neurosurgeon is among the highest of any profession, a direct result of the extensive training, high-stakes nature of the work, and the limited supply of qualified specialists. Salary data from various authoritative sources consistently places neurosurgery at or near the top of physician earnings.
It's important to distinguish between the salary of a resident—a doctor in training—and a fully licensed, board-certified attending neurosurgeon. The journey begins with a modest stipend and culminates in a substantial income.
According to the Medscape Physician Compensation Report 2023, one of the most respected annual surveys in the medical field, neurosurgery is the second-highest paid specialty.
> Neurosurgeons earned an average annual income of $788,313 in 2023. (Source: Medscape)
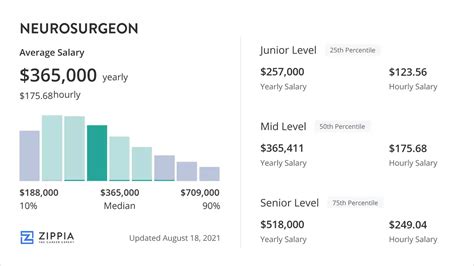
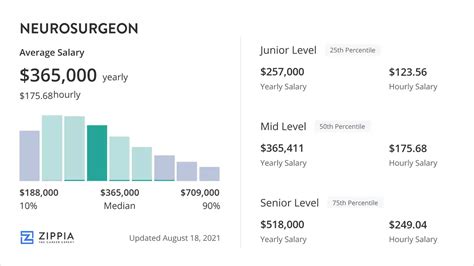
Other reputable sources provide similar figures, often with ranges that highlight the variability in compensation:
- Doximity's 2023 Physician Compensation Report also ranks neurosurgery as the #1 or #2 highest-paid specialty, with an average compensation of $763,908.
- Salary.com reports a median neurosurgeon salary of $698,001 as of late 2023, with the typical range falling between $525,801 and $883,601. The top 10% of earners can exceed $1,089,801.
- Payscale data indicates an average base salary around $485,000, but this figure rises dramatically when bonuses and profit-sharing are included, with total pay potentially reaching over $980,000.
These figures represent attending physicians, not residents. A neurosurgery resident's salary is far lower, typically ranging from $60,000 to $85,000 per year, depending on the institution and postgraduate year (PGY) level. This is a fixed stipend set by the hospital and does not include performance bonuses.
### Salary by Experience Level
The salary of a neurosurgeon grows significantly with experience. The leap from residency to an attending position is the most dramatic, but earnings continue to climb throughout a surgeon's mid-career.
Here is a typical progression, based on aggregated data from Medscape, Doximity, and Salary.com:
| Career Stage | Years of Experience | Typical Annual Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Neurosurgery Resident | 0-7 (Post-Med School) | $60,000 - $85,000 | Fixed institutional stipend. Long hours (often 80+/week). |
| Fellow | 7-8+ | $70,000 - $100,000 | Slight pay increase for sub-specialty training post-residency. |
| Early Career Attending | 1-5 | $400,000 - $650,000 | The largest salary jump occurs here. Often includes a starting bonus or loan repayment assistance. |
| Mid-Career Attending| 6-15 | $650,000 - $950,000+ | Peak earning years. Productivity bonuses (based on wRVUs) become a major component of pay. |
| Senior/Late Career | 16+ | $700,000 - $1,200,000+ | Experienced surgeons, often partners in private practice or department heads. Salary may plateau or slightly decrease if surgical volume declines in favor of administrative or teaching roles. |
### Anatomy of a Neurosurgeon's Compensation Package
The headline salary number is only part of the story. A neurosurgeon's total compensation is a package of several components:
1. Base Salary: This is the guaranteed, fixed portion of their pay. In hospital-employed or academic settings, this makes up the bulk of the income.
2. Productivity Bonuses: This is a critical—and often substantial—part of compensation. Most health systems use a model based on Work Relative Value Units (wRVUs). The Centers for Medicare & Medicaid Services (CMS) assigns a wRVU value to every medical procedure based on its complexity, time, and skill required. A simple consultation has a low wRVU value, while a complex spinal fusion or brain tumor resection has a very high value. Surgeons are often paid a certain dollar amount per wRVU generated above a set threshold. This system directly incentivizes performing more, and more complex, procedures. A neurosurgeon can earn hundreds of thousands of dollars in wRVU bonuses alone.
3. Performance & Quality Bonuses: Many institutions offer smaller bonuses tied to quality metrics, such as patient outcomes, patient satisfaction scores, and low complication rates.
4. On-Call Pay: Surgeons may receive a daily stipend for being on call for the emergency room, with additional compensation if they are called in to operate.
5. Profit Sharing (Private Practice): For neurosurgeons who are partners in a private practice group, a significant portion of their income comes from a share of the group's profits after all expenses (staff salaries, office lease, malpractice insurance) are paid. This model offers the highest earning potential but also carries the most financial risk and administrative responsibility.
6. Benefits and Perks: The value of a comprehensive benefits package should not be underestimated. This typically includes:
- Malpractice Insurance: This is a massive expense, often costing $50,000 to $150,000+ per year. Employer-paid malpractice coverage is a huge financial benefit.
- Health, Dental, and Vision Insurance: Comprehensive family plans.
- Retirement Plans: Generous 401(k) or 403(b) plans with significant employer matching contributions.
- Continuing Medical Education (CME) Allowance: Funds to attend conferences and stay current with new techniques.
- Relocation Bonus / Signing Bonus: Often in the range of $25,000 to $100,000 to attract talent to a new position.
- Student Loan Repayment Assistance: Some hospitals, particularly in underserved areas, offer significant assistance with medical school debt.
Key Factors That Influence Salary

A neurosurgeon's salary is not uniform across the board. Several key variables can cause compensation to swing by hundreds of thousands of dollars. Aspiring neurosurgeons and those negotiating contracts must understand these factors intimately.
###
Level of Education and Training
The educational path to becoming a neurosurgeon is one of the longest and most arduous in all of medicine, typically lasting 15-16 years after high school. While the final M.D. or D.O. degree is a prerequisite, it is the subsequent training that shapes earning potential.
1. Medical School (4 years): This is the foundation. Performance here—grades, research, and scores on the United States Medical Licensing Examination (USMLE)—is critical for matching into a competitive neurosurgery residency.
2. Neurosurgery Residency (7 years): This is the core training period. It is exceptionally competitive to enter a neurosurgery residency program. During these seven years, residents are paid a modest stipend ($60k-$85k) while working grueling hours. Their salary is not negotiable.
3. Fellowship Training (1-2 years): After residency, many neurosurgeons pursue a fellowship to sub-specialize. This is a critical decision that heavily influences career trajectory and salary. A surgeon who completes a fellowship in a high-demand, high-complexity field like complex spine surgery or endovascular neurosurgery can command a significantly higher starting salary and has access to more lucrative procedures than a general neurosurgeon. A fellowship signals an expert level of training that hospitals and private practices are willing to pay a premium for.
4. Board Certification: After completing residency and passing rigorous written and oral exams administered by the American Board of Neurological Surgery (ABNS), a neurosurgeon becomes "board-certified." This is the gold standard of qualification and is essential for hospital credentialing and commanding a top-tier salary. Not being board-certified is a major barrier to high earnings.
###
Years of Experience
As detailed in the table above, experience is a primary driver of salary growth. The financial trajectory is steep and front-loaded.
- The Leap from Training to Practice: The single biggest pay increase in a neurosurgeon's life is finishing residency/fellowship and taking their first attending job. Their salary can jump from ~$80,000 to over $500,000 overnight.
- The Growth Phase (Years 2-10): In the first decade of practice, a neurosurgeon builds their reputation, hones their surgical skills, and becomes more efficient. This directly translates to higher productivity (more wRVUs generated) and, consequently, higher bonus payouts. Their base salary will also increase with contract renewals.
- The Peak Earning Years (Years 10-20): This is often the period of maximum income. The surgeon has a mature practice, a strong referral network, and is operating at peak efficiency. In private practice, this is when they may have achieved full partner status, maximizing their share of the profits.
- The Plateau/Transition Phase (Years 20+): While some neurosurgeons maintain a high surgical volume late into their careers, many begin to transition. They may take on more administrative roles (like Department Chair), focus more on teaching and research, or strategically reduce their caseload to improve work-life balance. In these cases, their salary might plateau or even slightly decrease, though it remains exceptionally high by any standard.
###
Geographic Location
Where a neurosurgeon practices has a profound impact on their salary. This is often counterintuitive; salaries are frequently highest in areas with a lower cost of living, not in major coastal hubs like New York City or Los Angeles.
The primary driver is supply and demand. Major metropolitan areas on the coasts have an abundance of academic medical centers and are seen as desirable places to live, creating a surplus of specialists. This competition drives salaries down. Conversely, less populated states and regions in the Midwest and Southeast have a harder time recruiting top talent, forcing hospitals to offer much higher compensation packages to attract neurosurgeons.
The Medscape 2023 Physician Compensation Report highlights these regional differences for specialists:
| Region | Physician Compensation Rank | General Rationale |
| :--- | :--- | :--- |
| Midwest (e.g., IN, WI, IA) | High | High demand, lower specialist saturation, strong hospital systems. |
| Southeast (e.g., AL, KY, TN) | High | Growing populations, significant need, favorable malpractice environments. |
| Northwest (e.g., OR, WA) | Medium | Mixed market; some rural areas pay well, cities are more competitive. |
| Southwest (e.g., AZ, NM) | Medium | Varies by state; growing demand. |
| Northeast (e.g., MA, NY, MD) | Low | High saturation of specialists, dominant academic centers, higher cost of living. |
For example, a neurosurgeon might earn $950,000 in Wisconsin but $650,000 for a similar role in Boston. The cost of living difference further amplifies this disparity in disposable income.
###
Practice Setting (Company Type & Size)
The type of organization a neurosurgeon works for is arguably the most significant factor in determining both salary and lifestyle.
1. Academic Medical Center:
- Description: Part of a university hospital, with responsibilities for teaching medical students and residents, and conducting clinical research.
- Salary: Generally the *lowest* of the three main settings. The base salary is lower because a portion of the surgeon's time is "protected" for non-clinical (i.e., non-revenue-generating) academic activities.
- Pros: Prestige, cutting-edge technology, intellectual stimulation, opportunities for research and publication, typically better benefits and work-life balance.
- Cons: Lower earning potential, more bureaucracy, pressure to publish or secure research grants ("publish or perish").
2. Hospital-Employed (Community or Health System):
- Description: The surgeon is a direct employee of a hospital or a large, multi-hospital health system (e.g., HCA Healthcare, Mayo Clinic, Cleveland Clinic).
- Salary: Strong, stable base salary combined with a significant productivity bonus (wRVU) structure. This is currently the most common employment model.
- Pros: High and predictable income, relief from administrative burdens (billing, staffing, overhead are handled by the hospital), strong benefits, and built-in referral networks.
- Cons: Less autonomy than private practice, subject to hospital administration policies, and a ceiling on earning potential compared to a successful practice owner.
3. Private Practice (Solo or Group):
- Description: The surgeon owns all or part of the business. They are entrepreneurs as well as clinicians.
- Salary: The *highest potential earnings*, but also the highest risk. After covering massive overhead costs—staff salaries, office rent, equipment, and exorbitant malpractice insurance—the remaining revenue is the surgeon's income.
- Pros: Complete autonomy, potential for extremely high income (well over $1.5M - $2M is possible for successful partners), ability to build equity in a business.
- Cons: Immense administrative burden, financial risk, responsibility for all business operations, and often poorer work-life balance, especially in the early years of building the practice.
###
Area of Specialization
Within neurosurgery, sub-specialization through fellowship training can create distinct career paths and salary expectations. While all neurosurgeons are highly paid, some specialties are more lucrative than others.
- Spine Surgery: This is often the most common and financially rewarding sub-specialty. There is a massive patient population with degenerative spine disease, and procedures like spinal fusions, laminectomies, and disc replacements are in high demand and have high wRVU values. A neurosurgeon specializing in complex spine surgery is consistently among the highest earners.
- Cerebrovascular and Endovascular Neurosurgery: This field deals with aneurysms, AVMs, and stroke. It involves both traditional open-brain surgery and minimally invasive endovascular techniques (coiling, stenting). These are high-risk, high-complexity procedures that are compensated accordingly.
- Neuro-oncology (Tumor Surgery): Surgeons who specialize in removing complex brain and spinal tumors are highly valued. Their work is incredibly demanding and requires a unique skill set.
- Pediatric Neurosurgery: A highly specialized and emotionally demanding field. While compensation is excellent, it may be slightly lower than top-tier spine surgery, in part because the patient volume is smaller and some procedures have lower reimbursement rates.
- Functional Neurosurgery: This includes procedures like Deep Brain Stimulation (DBS) for Parkinson's disease and surgeries for epilepsy. It's a growing field with strong earning potential.
Generally, specialties that involve a higher volume of complex instrumentation (like spine surgery) or deal with life-threatening emergencies (like vascular neurosurgery) tend to have the highest compensation.
###
In-Demand Skills
Beyond the standard board certification, possessing specific advanced skills can increase a neurosurgeon's marketability and salary.
- Minimally Invasive Surgery (MIS): Proficiency in MIS techniques for both spine and cranial surgery is highly sought after. These procedures often lead to faster patient recovery, shorter hospital stays, and are preferred by patients. Hospitals market these capabilities heavily and will pay more for surgeons with this expertise.
- Robotic-Assisted Surgery: Experience with robotic platforms like the Mazor X or ROSA for spine surgery is a significant value-add. As technology becomes more integrated into the OR, this skill is becoming a prerequisite for top jobs.
- Endoscopic and Endonasal Surgery: The ability to perform surgery through the nose (endonasal) to reach skull base tumors is a highly specialized skill that commands a premium.
- Business Acumen: For those in or aspiring to private practice, skills in management, finance, and marketing are just as important as surgical skills for maximizing income.
- Leadership and Communication: Surgeons who can effectively lead a team, communicate empathetically with patients, and collaborate with hospital administration are more likely to be promoted to leadership positions (e.g., Chief of Surgery, Medical Director), which come with additional stipends and influence.
Job Outlook and Career Growth

For those willing to undertake the arduous training, the career outlook for neurosurgeons is exceptionally strong and stable. The demand for their specialized services is projected to grow, driven by several key demographic and technological trends.
The U.S. Bureau of Labor Statistics (BLS) groups neurosurgeons with all other physicians and surgeons. In its latest Occupational Outlook Handbook, the BLS projects that employment for this group will grow by 3% from 2022 to 2032. While this rate is about average for all occupations, it still translates to approximately 24,000 new job openings for physicians and surgeons each year over the decade, arising from both new job creation and the need to replace physicians who are retiring or leaving the profession.
However, the specific outlook for neurosurgery is likely even stronger than this general figure suggests due to several factors:
1. An Aging Population: The primary driver of demand is the aging of the Baby Boomer generation. As people live longer, there is a higher incidence of age-related neurological conditions that neurosurgeons treat, including degenerative spine disease, strokes, Parkinson's disease, and brain tumors.
2. Technological Advancements: The development of new technologies and surgical techniques is expanding the scope of what neurosurgeons can treat. Conditions that were once considered inoperable or untreatable can now be addressed with minimally invasive, robotic, or endoscopic procedures. This creates new demand for services.
3. Increased Access to Care and Diagnosis: Better and more widely available imaging technology (MRI, CT) means that neurological conditions are being diagnosed earlier and more frequently, leading to more referrals to neurosurgeons.
4. Limited Supply of Neurosurgeons: The number of neurosurgery residency positions in the United States is strictly limited and grows very slowly. There are only about 235 new residents accepted each year. This restricted supply, coupled with growing demand, ensures that qualified neurosurgeons will remain in high demand and can command high salaries.
### Future Challenges and Trends
Despite the positive outlook, the profession is not without its challenges. Neurosurgeons of the future will need to navigate a complex and evolving healthcare landscape.
- Burnout: