Table of Contents

- [What Does a UK Doctor Do?](#what-does-a-uk-doctor-do)
- [The Salary of UK Doctors: A Deep Dive](#the-salary-of-uk-doctors-a-deep-dive)
- [Key Factors That Influence a UK Doctor's Salary](#key-factors-that-influence-a-uk-doctors-salary)
- [Job Outlook and Career Growth for UK Doctors](#job-outlook-and-career-growth-for-uk-doctors)
- [How to Become a Doctor in the UK: A Step-by-Step Guide](#how-to-become-a-doctor-in-the-uk-a-step-by-step-guide)
- [Conclusion: Is a Career as a UK Doctor Worth It?](#conclusion-is-a-career-as-a-uk-doctor-worth-it)
---
Pursuing a career in medicine is more than a job choice; it's a profound commitment to a life of service, continuous learning, and immense responsibility. For many, the calling is driven by a deep-seated desire to heal and make a tangible difference in people's lives. But alongside this noble ambition lies a practical reality: the need for a sustainable and rewarding career. Understanding the financial landscape—the salary of UK doctors—is a critical component of making an informed decision about embarking on this demanding yet fulfilling journey.
The path is long and arduous, but the potential rewards, both intrinsic and financial, are significant. In the UK, a doctor's salary is not a single figure but a complex, structured journey that evolves dramatically from the first day as a newly qualified junior doctor to the peak of a consultant or General Practitioner's (GP) career. A doctor just starting their post-graduate training can expect a basic salary of around £32,398, while a highly experienced consultant or a successful GP partner can earn well over £100,000, with some exceeding £200,000 through a combination of NHS work, private practice, and additional responsibilities.
I once spoke with a senior surgical consultant who, after a complex, life-saving operation, quietly reflected on her early years of training. She described the exhaustion and self-doubt as "the price of entry," but the ability to give a family their loved one back as a "priceless dividend" that fueled her through every challenge. This balance of immense sacrifice and unparalleled reward is the very essence of a medical career in the United Kingdom. This guide will demystify the financial side of that equation, providing a comprehensive, data-driven look at what it means to earn a living as a doctor in the UK. We will dissect the intricate NHS pay scales, explore the myriad factors that influence earnings, and map out the long-term career and salary trajectory you can expect.
---
What Does a UK Doctor Do?

To comprehend the salary of a UK doctor, one must first appreciate the sheer breadth and depth of their role. The title "doctor" is an umbrella term for a vast array of specialities and work environments, from the bustling A&E departments of major city hospitals to the quiet, community-focused consultations of a rural GP surgery. However, a set of core responsibilities unites them all, centred on the overarching goal of maintaining and restoring human health.
At its heart, a doctor's job is to diagnose, treat, and prevent illness and injury. This involves a sophisticated blend of scientific knowledge, technical skill, and profound human empathy. They are clinical detectives, gathering clues from patient histories, physical examinations, and diagnostic tests to form a coherent picture of a patient's health status. Based on this diagnosis, they formulate and implement treatment plans, which can range from prescribing medication and recommending lifestyle changes to performing complex surgical procedures.
The daily tasks of a doctor are incredibly varied and depend heavily on their speciality, seniority, and place of work. A hospital-based doctor's day is often structured around ward rounds, where they review the progress of inpatients, adjust treatment plans, and communicate with the nursing team. This is interspersed with outpatient clinics, where they see patients for consultations, and, for many specialities, time in operating theatres, performing procedures. They also dedicate significant time to administrative tasks: updating patient records, writing referral letters, reviewing lab results, and communicating with other healthcare professionals to ensure coordinated patient care. Teaching and supervising junior colleagues are also fundamental responsibilities, especially for more senior doctors.
A General Practitioner (GP), on the other hand, operates as the first point of contact for patients within the community. Their role is broader, dealing with a vast spectrum of conditions, from acute minor illnesses to the long-term management of chronic diseases like diabetes and heart disease. A GP's day is dominated by a series of 10-15 minute appointments, requiring rapid assessment, diagnosis, and management decisions. They are the gatekeepers of the NHS, referring patients to specialist hospital care when necessary and coordinating a patient's overall healthcare journey.
### A "Day in the Life" of a Hospital Specialty Registrar (Cardiology)
To make this tangible, let's consider a hypothetical day for a mid-career doctor, a Specialty Registrar in their fourth year of cardiology training (ST4).
- 7:30 AM: Arrive at the hospital. Grab a quick coffee and head to the cardiology ward to get a handover from the night team. Review any overnight events, check vital signs and new test results for the 25 patients on the ward.
- 8:30 AM: Consultant Ward Round begins. As the senior registrar, you lead the presentation of each patient to the consultant. You discuss each case, propose changes to medication, order further investigations (like ECGs or blood tests), and create a management plan for the day. You also take time to teach the junior doctors (Foundation Year 1 and 2) on the team.
- 11:00 AM: The ward round finishes. You quickly delegate tasks to the junior doctors, double-check critical prescriptions, and then rush to the cardiac catheterisation lab ("cath lab").
- 11:15 AM: You are scheduled to perform two coronary angiograms under the supervision of a consultant. You meet the patients, explain the procedure, obtain consent, and then spend the next couple of hours performing the intricate diagnostic procedures.
- 2:00 PM: A brief, late lunch, often eaten while catching up on paperwork. You review the results of the angiograms, dictate letters to the patients' GPs, and respond to urgent emails and pager bleeps.
- 3:00 PM: You run the cardiology outpatient clinic. You see six patients with a variety of conditions, from follow-ups after a heart attack to new referrals for chest pain. Each consultation requires a thorough history, examination, and clear communication about their diagnosis and treatment.
- 5:30 PM: Clinic finishes. You head back to the ward for the evening handover with the junior team, ensuring all tasks from the morning round are complete and that there is a clear plan for the patients overnight.
- 6:30 PM: You finally sit down to finish your administrative tasks—updating patient records, chasing lab results, and completing a research data entry form for a clinical trial you're involved in.
- 7:30 PM: You hand your bleep over to the on-call registrar and head home, more than 12 hours after you arrived. If you were the registrar on-call, your day would be just beginning, as you would be responsible for all cardiology emergencies in the hospital overnight.
This example illustrates the intense, multi-faceted nature of the role. It is a constant juggling act of clinical care, administrative duties, teaching, and continuous learning, demanding resilience, exceptional time management, and an unwavering commitment to patient welfare.
---
The Salary of UK Doctors: A Deep Dive
The salary of a doctor in the United Kingdom is predominantly dictated by centrally negotiated contracts with the National Health Service (NHS), which is the single largest employer of medical professionals in the country. This results in a highly structured, transparent, and incremental pay system that is directly tied to a doctor's stage of training and years of experience. While private practice offers an alternative and often more lucrative path, the vast majority of doctors will spend all or a significant portion of their career within the NHS framework.
The data presented here is based on the national pay scales for doctors in England for the 2023/2024 financial year, as published by NHS Employers and the British Medical Association (BMA). It's important to note that pay scales are negotiated annually, and there can be slight variations for doctors working in Scotland, Wales, and Northern Ireland, although the structures are broadly similar.
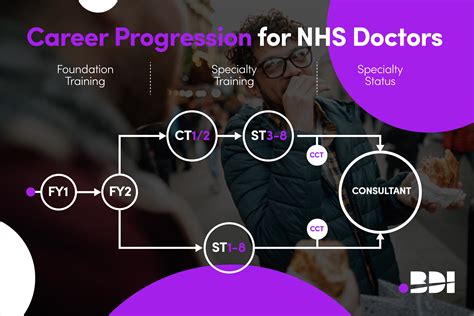
A doctor's journey through the NHS pay scales can be broken down into distinct stages:
1. Foundation Training (Junior Doctors)
2. Specialty Training (Junior Doctors, often called Registrars)
3. Specialty and Associate Specialist (SAS) Doctors
4. Consultants (Senior Doctors)
5. General Practitioners (GPs)
### Junior Doctor Pay
The term "junior doctor" is somewhat misleading, as it encompasses all doctors who have not yet completed their training to become a consultant or a GP. This can include doctors with over a decade of experience. Their pay is governed by the "2016 contract for doctors in training."
- Foundation Training (FY1 & FY2): This is a two-year training programme immediately following graduation from medical school.
- Foundation Year 1 (FY1): Basic Salary: £32,398
- Foundation Year 2 (FY2): Basic Salary: £37,303
- Specialty Training (Core & Higher): After the Foundation Programme, doctors enter specialty training (CT1/ST1 and beyond) to become a GP or a consultant. This period can last from three to eight years. The pay scale is "nodal," meaning there are fixed pay points based on the level of training.
- Core Training (CT1/ST1 - CT3/ST3): Basic Salary: £43,923
- Specialty Registrar (ST4+): As registrars take on more responsibility, their basic pay increases at set points.
- ST4/ST5: Basic Salary: £50,000 - £55,000 (approximate, varies with specific pay scale points)
- ST6 - ST8: Basic Salary: £58,398 - £63,152
### Additional Pay for Junior Doctors
The figures above represent basic pay for a standard 40-hour week. A junior doctor's total salary is often significantly higher due to supplementary payments for additional work, which is standard in most roles. According to the BMA, these additions can increase total pay by 20-40%.
- Weekend Allowance: A percentage enhancement for hours worked on weekends.
- On-Call Allowance: A fixed cash payment for being available on-call.
- Night Shift Enhancement: A 37% enhancement for hours worked during night shifts (typically 9 PM to 7 AM).
- Additional Hours: Payment for any hours worked over the standard 40.
Therefore, a Specialty Registrar with a basic salary of £58,398 could realistically see their gross pay packet reach £70,000 - £85,000 depending on the intensity of their on-call rota and the number of weekends and nights worked.
### Senior Doctor Pay: Consultants and GPs
Once training is complete, doctors move to senior contracts with substantially higher earning potential.
#### Consultant Salary
Consultants are senior doctors who have completed the full specialty training programme and are listed on the GMC's specialist register. They have ultimate clinical responsibility for their patients. The 2003 consultant contract in England has a defined pay scale with yearly increments (pay thresholds).
- Starting Salary (Year 1): £93,666
- Mid-Career (Year 10): £112,426
- Top of Scale (Year 19+): £126,281
Consultant Pay Progression (England, 2023/24)
| Years of Experience as Consultant | Basic Salary (Pay Threshold) |
| :------------------------------ | :--------------------------- |
| 0-1 (Starting) | £93,666 |
| 2-3 | £96,555 |
| 4-5 | £99,444 |
| 6-7 | £104,221 |
| 8-9 | £108,998 |
| 10-13 | £112,426 |
| 14-18 | £119,554 |
| 19+ | £126,281 |
*Source: NHS Employers Pay and Conditions Circular (M&D) 2/2023*
Additional Consultant Pay:
Consultants can significantly increase their earnings through:
- Clinical Excellence Awards (CEAs): National awards that recognise and reward exceptional contributions, adding thousands to an annual salary. (These are being phased out and replaced by Local Clinical Excellence Awards - LCEAs).
- Management Roles: Taking on roles like Clinical Director or Medical Director comes with additional responsibility payments, often adding £10,000 to £40,000+ per year.
- Additional Programmed Activities (PAs): Consultants can be paid to work more than the standard 10 PAs (4-hour blocks) per week.
- Private Practice: Working in the private sector outside of NHS hours.
With these additions, it is common for senior NHS consultants to earn £130,000 - £180,000, with those in high-demand specialties with significant private work earning considerably more.
#### General Practitioner (GP) Salary
GP salaries are not as straightforward as they are not directly employed by the NHS. They are independent contractors, and their income depends on the profitability of their practice. A practice's income comes from the NHS based on its patient list size, the services it provides (e.g., vaccinations, minor surgery), and local health targets.
- Salaried GP: These GPs are employed by a practice for a fixed salary. According to the BMA and NHS Digital data, the average salary for a full-time salaried GP is typically between £68,000 and £100,000 per year, depending on experience.
- GP Partner: These GPs own a share of the business and their income is a share of the practice's profits. This carries more risk and administrative burden but has higher earning potential. NHS Digital's report on GP Earnings and Expenses for 2021/22 showed the average pre-tax income for a partner GP was £148,000. However, this figure is before they pay their own taxes, national insurance, and professional expenses.
The salary landscape for UK doctors is therefore a predictable, structured progression within the NHS, with significant earning potential at the senior level. The transparency of the pay scales allows aspiring doctors to map out their financial future with a degree of certainty unparalleled in many other professions.
---
Key Factors That Influence a UK Doctor's Salary

While the NHS pay scales provide a clear and rigid framework, a doctor's ultimate take-home pay is influenced by a multitude of intersecting factors. Understanding these variables is key to appreciating the nuances of medical careers and the opportunities for financial growth. This section delves into the six most critical elements that shape the salary of a UK doctor.
###
1. Training Stage and Seniority
This is, without question, the single most dominant factor determining a doctor's salary in the UK. The career is a long apprenticeship, with pay explicitly linked to progress along the training pathway. As we detailed in the previous section, the salary structure is designed to reward the increasing levels of skill, experience, and clinical responsibility a doctor assumes over time.
- Medical Student: No salary; in fact, this stage involves accruing significant debt through tuition fees and living costs.
- Foundation Doctor (FY1/FY2): The first rung on the ladder. The FY1 basic salary of £32,398 reflects their status as a provisionally registered doctor requiring close supervision. The jump to £37,303 for FY2 acknowledges a year of experience and full GMC registration.
- Specialty Registrar (ST1-ST8): This long training period (3-8 years) sees steady and predictable salary growth. The jump from FY2 (£37,303) to a first-year registrar role (e.g., ST1 in medicine at £43,923) represents a significant increase. The subsequent rises, culminating in a basic salary of £63,152 for a senior registrar (ST8), are designed to match their growing autonomy and expertise. Total remuneration during these years, including banding for on-call work, often places them in the £55,000 to £85,000 range.
- Consultant/GP: Completing training marks the most substantial pay increase in a doctor's career. The leap from a senior registrar's basic salary of ~£63,000 to a new consultant's starting salary of £93,666 is a near 50% increase in basic pay. From this point, salary progression is no longer about training stages but about years of service. The consultant pay scale rewards loyalty and experience, with an established consultant of 20 years earning a basic salary of £126,281, more than double that of a senior registrar.
The entire system is a transparent escalator, with each step up in responsibility and training completion directly rewarded with a corresponding and significant rise in basic pay.
###
2. Area of Specialization
Once a doctor completes their training, their chosen specialty plays a pivotal role in their long-term earning potential, primarily through opportunities outside of the standard NHS contract.
While the basic NHS consultant pay scale is identical across all hospital specialties—a neurosurgeon and a geriatrician with the same level of experience will have the same basic NHS salary—the potential for supplementary income varies dramatically.
- High-Earning Specialties (Private Practice Potential): Certain specialties have a much larger and more lucrative private market. These tend to be procedure-heavy fields where patients are more willing to pay to skip NHS waiting lists.
- Orthopaedic Surgery: Joint replacements (hip, knee) are in high demand.
- Ophthalmology: Cataract surgery and vision correction procedures are common private treatments.
- Cardiology: Private consultations, diagnostic tests (echocardiograms), and procedures like angioplasty.
- Plastic Surgery: A large market for both cosmetic and reconstructive procedures.
- Dermatology: Consultations for skin conditions and cosmetic procedures.
A consultant in one of these fields could potentially add £50,000 to £150,000+ per year to their NHS salary through private work, pushing their total earnings well over £250,000.
- General Practice (GP): As independent contractors, GPs have a different model. Their income is tied to practice management and efficiency. GP partners in well-run, large practices in affluent areas may earn more than those in smaller, more deprived areas. They can also boost income by specialising in areas like minor surgery, dermatology, or occupational health within the practice. The average GP partner income of £148,000 (pre-expenses) reflects this high earning potential, often exceeding that of a standard NHS consultant's basic pay.
- Specialties with Less Private Practice: Many vital specialties have a much smaller private sector, meaning their practitioners' earnings are more closely tied to the NHS consultant scale.
- Emergency Medicine: Acute, unscheduled care is almost exclusively delivered by the NHS.
- Intensive Care Medicine: Critically ill patients are cared for within the NHS system.
- Geriatrics & Palliative Care: While some private work exists, it is far less common.
- Most areas of Psychiatry: Although a private market for therapy and psychiatric consultation exists, it's smaller than for surgical specialties.
###
3. Geographic Location
Unlike in many other professions where salaries can vary wildly by region, the NHS's national pay contracts create a largely uniform salary landscape across the UK. A consultant in Manchester earns the same basic salary as a consultant with identical experience in Bristol or Newcastle. However, there is one major exception: London.
- London Weighting: To compensate for the significantly higher cost of living in and around the capital, the NHS provides a supplementary payment known as "London Weighting." This is paid to all NHS staff, including doctors, who work in eligible zones.
- According to the BMA, for junior doctors, this is a flat-rate payment. For 2023/24, it is £2,162 per year for those working within the M25.
- For consultants, the weighting is applied as a percentage of basic salary, capped at a certain level. It typically adds between £2,000 and £8,000 to a consultant's annual pay.
While this helps, most analyses conclude that the London Weighting does not fully cover the increased costs of housing and transport in the capital. Therefore, while the nominal salary is highest in London, the disposable income for a doctor may actually be higher in other major UK cities where living costs are lower. This is a critical consideration for doctors deciding where to train and practice. Some less popular or more remote regions may also offer recruitment and retention premia to attract doctors, but these are less common and more specific to certain trusts or specialties facing shortages.
###
4. Employer Type: NHS vs. Private Sector
The vast majority of doctors in the UK work for the National Health Service (NHS). It is the primary training body and the country's largest employer. As discussed, pay is transparent, structured, and secure, with a generous NHS pension scheme that is a major component of the total compensation package.
However, doctors can also work partially or wholly in the private sector.
- Portfolio Career (NHS + Private): This is the most common model for private work. A consultant will typically hold a substantive NHS contract (e.g., for 8-10 Programmed Activities per week) and use their remaining time (evenings, weekends) to see private patients. This provides the stability and pension benefits of the NHS contract while maximising income through private fees.
- Wholly Private Practice: A smaller number of doctors, usually established consultants in high-demand specialties, leave the NHS entirely to work full-time in the private sector. This path offers the highest earning potential but comes with the risks of running a business. There is no guaranteed salary, no sick pay, and no NHS pension. The doctor must cover their own professional indemnity, marketing, administrative staff, and clinic rental costs. Earnings are theoretically uncapped but are highly dependent on reputation, specialty, and business acumen. A top private surgeon in London could earn in excess of £500,000 per year, but this represents the very top percentile.
###
5. Additional Skills and Responsibilities
Within the NHS system, there are numerous avenues for doctors, particularly consultants, to increase their base salary by taking on roles that go beyond standard clinical duties.
- Management and Leadership: Taking on formal leadership roles is a primary way to boost income.
- Clinical Lead/Head of Department: This involves managing a department's rota, budget, and staff. It usually comes with an additional responsibility payment.
- Clinical Director: Overseeing a larger directorate (e.g., all surgical services). This often includes 1-2 additional paid PAs and a significant management allowance, potentially adding £15,000 - £25,000 to a salary.
- Medical Director: The most senior medical position in an NHS Trust, sitting on the hospital board. This is a major leadership role with a salary that can be significantly higher than the standard consultant scale, often in the range of £150,000 - £200,000+.
- Teaching and Academia: Many doctors are involved in teaching medical students. A formal role as a Director of Medical Education or a joint appointment with a university (Clinical Lecturer/Professor) comes with a dedicated salary for that work.
- Research: Doctors who are active in clinical research, leading trials and publishing papers, can attract grant funding and may hold academic positions that supplement their NHS income.
- Intensity of Work: As mentioned for junior doctors, the intensity of the on-call rota directly impacts pay through enhancements. For consultants, agreeing to work more than the standard 10 Programmed Activities (PAs) per week results in extra pay. A consultant working 12 PAs a week will earn 20% more in basic pay than a colleague working 10 PAs.
###
6. In-Demand Skills and Qualifications
While not a direct salary multiplier in the same way as a management role, possessing certain skills can make a doctor more attractive for competitive posts, particularly those with higher earning potential.
- Sub-specialist Expertise: Within a broad specialty like cardiology, having advanced skills in a niche area like interventional cardiology (stenting) or electrophysiology (pacemakers) can open doors to lead roles in tertiary centres.
- Medical Technology/Informatics: With the NHS undergoing digital transformation, doctors with expertise in health informatics, data analysis, or the implementation of electronic patient records are highly valued for leadership roles in this area (e.g., Chief Clinical Information Officer).
- Medical Law and Ethics: A postgraduate qualification in medical law can lead to roles on ethics committees or as an expert witness, which can be a source of supplementary income.
- Appraisal and Revalidation: Becoming a trained appraiser for other doctors is another skill that can provide additional paid work.
In essence, the UK doctor's salary journey begins on a standardized, predictable track. However, as a doctor becomes more senior, their choices—in specialty, location, and the balance between clinical work, management, and private practice—create divergent paths with vastly different long-term financial outcomes.
---
Job Outlook and Career Growth for UK Doctors
The career of a doctor in the United Kingdom offers exceptionally high job security and a clearly defined path for progression. However, the profession is currently navigating a period of significant challenge and transformation, which will shape the working lives and opportunities for doctors over the next decade. The outlook is a complex picture of high demand, workforce pressures, and evolving models of care.
### Demand and Workforce Projections
The demand for doctors in the UK is projected to grow robustly and consistently. This is driven by several key factors: an aging population with more complex, chronic health needs; advancements in medical technology and treatments that require specialist skills; and a renewed focus on public health and preventative medicine.
The NHS Long Term Workforce Plan, published in June 2023, provides the most authoritative projection of future needs. It is a landmark document that sets out the strategy for recruiting and retaining staff for the next 15 years. The plan explicitly states that without intervention, the NHS in England would
