Introduction

Are you a physician feeling the immense pressure of a healthcare system that often prioritizes volume over value? Do you dream of practicing medicine the way you envisioned in medical school—with ample time for each patient, a focus on proactive wellness, and a genuine connection that fosters better health outcomes? If you're grappling with burnout, administrative overload, and the feeling that you're on a treadmill, you may have started exploring an alternative path: concierge medicine. This rapidly growing practice model offers a compelling proposition: a chance to reclaim your autonomy, deepen patient relationships, and significantly enhance your professional satisfaction and financial well-being. The potential improvement in a concierge medicine salary is often a primary motivator, with many physicians seeing a substantial increase in their earnings while working fewer hours.
For many dedicated doctors, the current system is simply unsustainable. I once spoke with a highly-respected internal medicine physician who was on the verge of leaving clinical practice altogether, worn down by 15-minute appointment slots and overwhelming paperwork. After transitioning her practice to a concierge model, she described the change as "breathing for the first time in a decade," finally able to provide the comprehensive, unhurried care her patients deserved, which in turn revitalized her passion for her calling.
This guide is designed to be your definitive resource on the financial and professional realities of a career in concierge medicine. We will dissect every component of a concierge medicine salary, explore the factors that dictate your earning potential, and provide a clear, step-by-step roadmap for making the transition. Whether you are a resident contemplating your future or an established physician seeking a more sustainable and rewarding career, this article will provide the expert analysis you need to make an informed decision.
### Table of Contents
- [What Does a Concierge Physician Do?](#what-does-a-concierge-physician-do)
- [Average Concierge Medicine Salary: A Deep Dive](#average-concierge-medicine-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Transition into Concierge Medicine](#how-to-transition-into-concierge-medicine)
- [Conclusion](#conclusion)
---
What Does a Concierge Physician Do?

At its core, a concierge physician is a primary care doctor (typically in internal medicine, family medicine, or pediatrics) who offers their professional services to a limited number of patients in exchange for a recurring membership fee. This fundamental shift in the business model—from fee-for-service insurance billing to a direct-to-patient retainer—is what enables the profound differences in the day-to-day practice of medicine.
Unlike a traditional primary care physician who may be responsible for a panel of 2,000 to 3,000 patients, a concierge doctor deliberately limits their practice to a few hundred, often between 100 and 600 patients. This dramatically smaller patient panel is the key that unlocks the model's primary benefits: time and accessibility.
Core Roles and Responsibilities:
The responsibilities of a concierge physician extend far beyond the reactive, problem-oriented care that characterizes much of traditional medicine. Their role is multifaceted and deeply proactive:
1. Comprehensive, Unhurried Appointments: The most significant change is the gift of time. Standard appointments can last 30, 60, or even 90 minutes, allowing for deep dives into a patient's health history, lifestyle, and wellness goals. Annual physicals are exceptionally thorough, often including advanced screenings not typically covered by insurance.
2. Enhanced Accessibility and Communication: Patients pay a premium for unparalleled access. This often includes 24/7 availability via cell phone, text, or email for urgent issues. Same-day or next-day appointments for acute problems are the standard, not the exception.
3. Proactive and Preventive Care: With a deep understanding of each patient, concierge doctors can focus on prevention, longevity, and wellness. This involves creating personalized health plans, nutritional guidance, fitness coaching, and stress management strategies.
4. Care Coordination and Advocacy: A concierge physician acts as the quarterback of their patient's healthcare team. They actively coordinate with specialists, review hospital records, and advocate for their patients within the broader, often fragmented, healthcare system. This can mean personally calling a specialist to secure an appointment or discussing a care plan with a hospitalist.
5. Practice Management: For those who own their practice, the role is also that of an entrepreneur. This involves managing staff, marketing the practice, handling financials, and ensuring regulatory compliance. While there is far less insurance-related administrative work, the physician is now running a small business.
### A "Day in the Life" of a Concierge Physician
To truly understand the difference, consider this sample day, which contrasts sharply with the high-volume churn of a traditional practice.
- 8:00 AM - 8:30 AM: Review the day's schedule, check for any overnight patient messages, and read up on the latest labs for the two patients scheduled for the morning.
- 8:30 AM - 10:00 AM: First patient appointment. This is a 90-minute annual wellness visit with a 55-year-old executive. The visit includes a full physical exam, a detailed review of advanced lipid panels and inflammatory markers, and a robust discussion about sleep hygiene, travel health, and a new strength training regimen.
- 10:00 AM - 10:30 AM: Call a cardiologist to discuss the EKG results of another patient and coordinate a follow-up consultation. The physician makes the call directly, ensuring a seamless handoff.
- 10:30 AM - 11:30 AM: Second patient appointment. A 45-minute follow-up with a patient managing type 2 diabetes. They spend time reviewing blood sugar logs from a continuous glucose monitor and making fine-tuned adjustments to their diet and medication, focusing on lifestyle modifications.
- 11:30 AM - 12:00 PM: Charting and administrative time. Notes are completed while the details are fresh. There are no complex insurance codes to battle.
- 12:00 PM - 1:00 PM: A full, uninterrupted lunch break.
- 1:00 PM - 1:30 PM: A telemedicine video call with a patient who is traveling and has developed a minor sinus infection. A prescription is called in to a pharmacy at their destination.
- 1:30 PM - 3:00 PM: Third and final patient of the day. A 70-year-old patient and their adult child visit to discuss advanced care planning and review a complex medication list after a recent hospitalization. The unhurried pace allows for sensitive, empathetic conversation.
- 3:00 PM - 4:30 PM: Dedicated time for practice development. This could involve writing a monthly wellness newsletter for patients, researching a new piece of diagnostic equipment, or meeting with a financial advisor.
- 4:30 PM: The physician heads home, free from a mountain of paperwork and with the mental energy to enjoy their evening. They remain on call for urgent matters but have built a practice that respects their time and well-being.
---
Average Concierge Medicine Salary: A Deep Dive
The financial landscape of concierge medicine is fundamentally different from traditional, insurance-based practice. A physician's income is no longer dictated by the number of patients seen or procedures billed (volume), but by the number of members enrolled and the annual fee charged (value). This model generally leads to a higher and more predictable revenue stream.
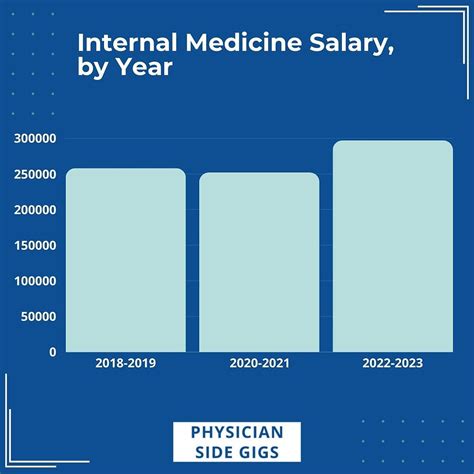
While the U.S. Bureau of Labor Statistics (BLS) does not have a separate category for "Concierge Physician," we can establish a baseline using their data for related specialties. According to the May 2022 BLS Occupational Employment Statistics, the median annual wage for General Internal Medicine Physicians was $225,270, and for Family Medicine Physicians, it was also $225,270. It's important to note these figures often represent employed physicians in large health systems and are subject to the pressures of high patient loads and insurance reimbursement rates.
Concierge physicians, by contrast, consistently report higher earnings. According to *Concierge Medicine Today*, a leading industry publication, the average salary for a concierge doctor can range from $280,000 to $500,000 or more. This represents a significant increase over their counterparts in traditional practice.
The income is a direct function of a simple equation:
Gross Revenue = (Number of Patients) x (Annual Membership Fee)
Net Income (Salary) = Gross Revenue - Practice Overhead
Let's illustrate with a hypothetical scenario:
- A physician caps their patient panel at 300.
- The annual membership fee is $2,200 per patient.
- Gross Revenue: 300 patients * $2,200/patient = $660,000
- Overhead: Concierge practices typically have lower overhead (30-40%) than traditional practices (50-60%) due to smaller staff sizes (no need for extensive billing and coding personnel) and less physical space required. Assuming a 35% overhead: $660,000 * 0.35 = $231,000.
- Net Income (Physician's Salary): $660,000 - $231,000 = $429,000
This figure is substantially higher than the national median for primary care and highlights the financial appeal of the model.
### Salary Brackets by Experience Level
Salary in concierge medicine is less about a traditional "entry-level vs. senior" corporate ladder and more about the maturity and reputation of the physician's practice.
| Career Stage | Typical Experience & Practice Status | Estimated Annual Salary Range | Sources & Rationale |
| :--- | :--- | :--- | :--- |
| Transitioning / Early-Career Concierge Physician | A physician in the first 1-3 years of a new concierge practice. Patient panel is still growing (e.g., 100-150 patients). May still be paying off start-up costs. | $180,000 - $250,000 | Analysis based on initial lower patient loads and higher upfront costs. Income may be temporarily lower than their previous traditional role as they build their panel. |
| Mid-Career / Established Concierge Physician | 3-10 years in a concierge model. Has a full or nearly full patient panel (250-400 patients). Has established a strong reputation in the community. | $280,000 - $450,000 | Reflects data from industry reports like *Concierge Medicine Today* and salary aggregators like Salary.com, which often place the median around $350,000. |
| Senior / Elite Concierge Physician | 10+ years in the model. May have a waiting list, command a premium fee, or operate in a high-demand, affluent market. May have diversified into executive health or consulting. | $450,000 - $700,000+ | Represents the top tier of earners. This level is achieved through exceptional reputation, premium pricing, and often, an advantageous geographic location. Some elite practitioners in major metro areas can exceed this range. |
### Compensation Components: Beyond the Base Salary
The compensation structure in concierge medicine is unique. For a physician who owns their practice, the "salary" is the net profit of the business.
- Membership Fees: This is the primary source of revenue. Fees are typically collected annually, semi-annually, or quarterly. According to *Concierge Medicine Today*, fees can range from $1,800 to $2,500 per year on average, but can easily exceed $5,000 in major metropolitan areas or for highly specialized services.
- Ancillary Services: Some practices may generate additional revenue through services not included in the membership fee, such as aesthetic procedures, advanced nutritional counseling, or specialized testing.
- Hybrid Model Revenue: In a hybrid model, a physician maintains a smaller traditional, insurance-based practice while also seeing a panel of concierge patients. Their income is a blend of insurance reimbursements and membership fees.
- Bonuses and Profit Sharing: In larger concierge group practices (e.g., MDVIP, SignatureMD), physicians are often employed. Their compensation might consist of a base salary plus bonuses tied to patient retention, practice growth, or quality metrics. If they have an equity stake, they may also participate in profit sharing.
- Owner's Draw vs. Salary: A practice owner can pay themselves a formal W-2 salary or take an "owner's draw" from the business profits. This decision has different tax implications and is typically made in consultation with an accountant.
The key takeaway is that the concierge medicine salary is not a fixed number but a dynamic outcome of a physician's business decisions, patient panel size, and fee structure. It offers a direct and transparent link between the value provided and the financial reward received.
---
Key Factors That Influence Salary

While the average concierge medicine salary is attractive, the actual take-home pay for a physician can vary dramatically. Several critical factors influence earning potential, and understanding them is essential for any doctor contemplating this career path. This is not simply a job; it is a business, and its success hinges on a blend of clinical expertise and entrepreneurial acumen.
###
Level of Education and Board Certification
In concierge medicine, the foundational educational requirement is non-negotiable: a Doctor of Medicine (M.D.) or Doctor of Osteopathic Medicine (D.O.) degree, followed by the completion of a residency program in a primary care field. However, beyond this baseline, certain credentials significantly enhance a physician's credibility and, by extension, their ability to attract patients and command higher fees.
Board Certification is paramount. Being board-certified by the American Board of Internal Medicine (ABIM), the American Board of Family Medicine (ABFM), or the American Board of Pediatrics (ABP) is considered the standard of excellence. It signals to prospective patients that the physician has met rigorous, nationally recognized standards for knowledge and practice. Lacking board certification can be a significant barrier to building a successful concierge practice, as patients paying a premium expect a provider at the top of their field.
Advanced Training and Fellowships can also play a role, particularly in differentiating a practice.
- Geriatrics: A fellowship in geriatrics can make a physician highly attractive in markets with a large retiree population (e.g., Florida, Arizona).
- Sports Medicine: A primary care sports medicine (PCSM) fellowship allows a physician to cater to active adults, "weekend warriors," and families with young athletes.
- Functional/Integrative Medicine: Certifications from bodies like the Institute for Functional Medicine (IFM) are increasingly popular. Patients seeking a root-cause, holistic approach to health are often willing to pay a premium for physicians with this specialized training.
While these additional qualifications don't have a direct, formulaic impact on salary in the way a corporate promotion might, they directly influence the practice's value proposition. A physician with advanced credentials can justify a higher annual fee and attract a more specific, motivated patient demographic, ultimately leading to higher revenue and net income.
###
Years of Experience and Established Reputation
Unlike many professions where one can enter at an "entry-level," concierge medicine is generally a mid-career move. Experience and reputation are arguably the most potent drivers of success and salary.
- Early-Career (0-5 Years in Practice): It is very challenging for a physician fresh out of residency to launch a solo concierge practice. They lack an established patient base to convert and have not yet built the community reputation necessary to attract new members. Their path is typically to join a larger, existing concierge group as an employed physician, where they can build their skills and panel under an established brand. Their starting salary in such a role will be on the lower end of the concierge spectrum, likely in the $200,000 to $275,000 range.
- Mid-Career (5-20 Years in Practice): This is the sweet spot for transitioning to a concierge model. These physicians have a deep well of clinical experience and, crucially, a loyal patient following from their years in traditional practice. They have built trust within the community and have a strong referral network of specialists. When they announce their transition, a significant portion of their existing patients may choose to follow them, providing an immediate revenue base. It is in this stage that physicians see their salaries climb into the $300,000 to $500,000 range as their panel fills and the practice matures.
- Senior-Career (20+ Years in Practice): Highly experienced physicians with decades of impeccable reputation are the titans of the concierge world. They are seen as pillars of the medical community. Their practices are often full with long waiting lists. This allows them to be highly selective and command premium fees, pushing their income potential to $500,000 and beyond. Their "salary" is a direct reflection of a lifetime of building trust and delivering exceptional care.
###
Geographic Location
Location is a make-or-break factor for a concierge practice. The viability and profitability of the model are inextricably linked to the demographic and economic characteristics of the surrounding area. The salary potential can vary by hundreds of thousands of dollars based on zip code alone.
High-Paying Areas:
These are typically affluent urban and suburban locales with a high concentration of high-income professionals, executives, and retirees who value health and have the disposable income to pay for premium services.
- Major Metropolitan Hubs: Cities like New York, Los Angeles, San Francisco, and Chicago have dense populations of potential patients who prioritize convenience and high-touch service. Fees in these areas can easily be $5,000 to $10,000+ per year.
- Affluent Suburbs: Areas surrounding major cities, such as Fairfield County, CT; Scottsdale, AZ; Boca Raton, FL; or Newport Beach, CA, are prime territories. They combine wealth with a community-oriented feel that is conducive to building a reputation.
- Wealthy Retirement Communities: Locations popular with affluent retirees are hotspots. These patients are often managing multiple chronic conditions and highly value the advocacy and coordination a concierge doctor provides.
Lower-Paying / Less Viable Areas:
- Rural Communities: In areas with lower average incomes and sparser populations, the math often doesn't work. There may not be a critical mass of residents able to afford an annual fee of several thousand dollars. The related model of Direct Primary Care (DPC), with its much lower monthly fees ($70-$100/month), is often a better fit for these regions.
- Lower-Income Urban Areas: Similarly, the concierge model is generally not viable in neighborhoods with lower socioeconomic status.
A physician in a prime Florida location might charge $3,000/year for a panel of 400 patients (grossing $1.2M), while a physician in a mid-sized Midwestern city might charge $1,800/year for a panel of 250 patients (grossing $450,000). This geographic disparity is a primary determinant of the ultimate salary.
###
Practice Model & Size (Replaces "Company Type")
The business structure a physician chooses has a direct and profound impact on their autonomy, risk, and compensation.
- Solo Practice (The Entrepreneur): Starting a practice from scratch offers the highest potential reward and the highest risk. The physician is the owner and operator, retaining 100% of the profits after overhead. This path offers complete autonomy but requires significant business acumen, marketing skill, and startup capital. The income potential is theoretically unlimited but directly tied to the owner's ability to run a successful business.
- Joining a Concierge Franchise/Group (The Franchisee/Employee): Partnering with a large, national organization like MDVIP or SignatureMD offers a turnkey solution. These companies provide support with marketing, legal setup, and administrative tasks in exchange for a portion of the revenue or a set fee. This lowers the initial risk and administrative burden. Physicians in these models are often considered affiliates or employees. Their compensation is typically a percentage of the revenue they generate, leading to salaries often in the $250,000 to $400,000 range. They trade some autonomy and top-end earning potential for stability and support.
- Hybrid Model (The Transitioner): In this model, a physician converts a portion of their practice to concierge while continuing to see traditional, insurance-based patients. This is a common de-risking strategy. For example, a doctor might see 50-100 concierge patients in the morning and 10-15 traditional patients in the afternoon. The salary is a blend of membership fees and insurance reimbursements. This can be a good transitional step, but it can also be difficult to manage, essentially running two different businesses under one roof.
- Direct Primary Care (DPC) vs. Concierge: It's crucial to distinguish DPC from concierge. DPC is a high-volume, low-cost version of direct care. Fees are much lower (e.g., $75/month), patient panels are larger (e.g., 600-800), and the focus is on affordability and basic primary care. DPC physicians typically do not bill insurance for any services. Concierge physicians, on the other hand, charge higher fees for more comprehensive, high-touch service and *usually* still bill the patient's insurance for covered office visits and procedures (a practice known as "hybrid billing"). The salary potential in a high-fee concierge model is generally higher than in a low-fee DPC model.
###
Area of Specialization
While concierge medicine is dominated by primary care, some specialists are successfully adopting the model, creating a niche with very high earning potential.
- Primary Care (Internal Medicine, Family Medicine): This is the foundation of the concierge movement. The model is perfectly suited to the long-term, relationship-based nature of primary care. Salaries in this area form the basis for the ranges discussed throughout this article.
- Concierge Cardiology: In affluent areas, patients with a history of heart disease may pay a significant premium for a concierge cardiologist. This provides them with enhanced access for urgent concerns, proactive management of risk factors, and close coordination of their cardiac care. The fees, and therefore potential salary, can be substantially higher than in primary care.
- Other Emerging Specialties: We are beginning to see the model applied to endocrinology, rheumatology, and even psychiatry. A patient with a complex, chronic condition who requires frequent monitoring and adjustment may find immense value in a concierge specialist. These are still niche areas, but for a physician with the right reputation and patient base, the financial upside is considerable.
###
In-Demand Skills
A successful concierge physician must be more than a great clinician; they must be a well-rounded professional. The skills that command a higher salary in this field are not technical medical procedures but a blend of business, communication, and wellness expertise.
- Business Acumen: Understanding how to read a profit and loss statement, manage a budget, negotiate vendor contracts, and create a business plan are essential for solo practitioners.
- Marketing and Sales: Physicians must be able to articulate their value proposition and "sell" their services without sounding like a salesperson. This involves networking, public speaking, and digital marketing.
- Exceptional Communication & Empathy (Bedside Manner): This is the core product. Patients are paying for a relationship. The ability to listen, build trust, and communicate with empathy is non-negotiable and directly correlates with patient retention.
- Wellness and Lifestyle Coaching: Many patients are not just seeking sick care; they want a guide for optimal living. Expertise in nutrition, fitness, stress management, and sleep science adds tremendous value and can justify higher fees.
- Technological Proficiency: Comfort with telemedicine platforms, patient portals, wearable health devices (like Oura rings or WHOOP bands), and electronic health records is crucial for delivering modern, convenient care.
---
Job Outlook and Career Growth

The future for concierge medicine is exceptionally bright, driven by powerful, converging trends in the U.S. healthcare landscape. While the BLS projects a modest 3% growth for physicians and surgeons overall from 2022 to 2032, the niche of concierge and direct-to-patient care is expanding at a much faster rate. A 2023 report from Grand View Research projected the global concierge medicine market to grow at a compound annual growth rate (CAGR) of 10.27% from 2023 to 2030.
This robust growth is fueled by two primary forces: widespread patient dissatisfaction and escalating physician burnout.
1. Patient Demand: Patients are increasingly frustrated with the traditional healthcare experience. Long wait times for appointments, rushed 10-minute visits, difficulty communicating with their doctor, and the impersonal nature of large health systems have created a strong market for a better alternative. An aging U.S. population with a higher prevalence of chronic diseases also values the intensive management and advocacy that concierge medicine provides. As awareness of the model grows, so too will the pool of potential patients willing to pay for superior service and access.
2. Physician Burnout: The current fee-for-service system is a leading cause of burnout among primary care physicians. The relentless pressure to see more patients in less time, coupled with a crushing administrative burden from insurance billing and electronic health records, has led many doctors to seek a more sustainable career path. Concierge medicine offers a lifeline—a way to practice medicine on their own terms, restore work-life balance, and rediscover the joy that led them to the profession in the first place. This "supply-side" pressure will continue to
