Introduction

In the high-stakes, technology-driven environment of the Intensive Care Unit (ICU), a special kind of leader emerges. They are the calm in the storm, the clinical decision-makers at the bedside, and the compassionate communicators for families in crisis. They are Critical Care Nurse Practitioners (NPs), and they represent one of the most challenging, respected, and financially rewarding specialties in advanced practice nursing. If you are driven by a passion for complex patient care and a desire to practice at the pinnacle of your clinical abilities, this career is likely on your radar.
But passion alone doesn't pay the bills. Understanding the financial landscape is a crucial part of your career planning. A career as a Critical Care NP is not just a calling; it's a significant professional and financial investment that yields substantial returns. The national average critical care NP salary consistently surpasses the six-figure mark, often landing in the $120,000 to $145,000 range, with top earners in high-demand areas exceeding $180,000 or more annually when including bonuses and differentials.
I once spoke with a seasoned Critical Care NP who had just managed a complex case involving a patient on advanced life support. She described her role not as a job, but as the "privilege of standing in the gap between uncertainty and hope for families at their most vulnerable." This article is for those who feel that same pull—to combine deep clinical expertise with profound human connection, all while building a secure and prosperous future.
This guide will serve as your definitive resource, breaking down every facet of the Critical Care NP salary, the factors that shape it, and the precise steps you need to take to enter and excel in this elite field.
### Table of Contents
- [What Does a Critical Care Nurse Practitioner Do?](#what-does-a-critical-care-nurse-practitioner-do)
- [Average Critical Care NP Salary: A Deep Dive](#average-critical-care-np-salary-a-deep-dive)
- [Key Factors That Influence a Critical Care NP Salary](#key-factors-that-influence-a-critical-care-np-salary)
- [Job Outlook and Career Growth for Critical Care NPs](#job-outlook-and-career-growth-for-critical-care-nps)
- [How to Become a Critical Care Nurse Practitioner](#how-to-become-a-critical-care-nurse-practitioner)
- [Conclusion: Is a Career as a Critical Care NP Right for You?](#conclusion-is-a-career-as-a-critical-care-np-right-for-you)
---
What Does a Critical Care Nurse Practitioner Do?

A Critical Care Nurse Practitioner, also known as an Acute Care Nurse Practitioner (ACNP) working in a critical care setting, is an advanced practice registered nurse (APRN) who provides comprehensive care to patients who are critically ill or unstable. They are the clinical quarterbacks of the ICU, working with a high degree of autonomy, often in collaboration with intensivists (physicians specializing in critical care), to manage the most complex and life-threatening conditions.
Their scope of practice is vast and requires an immense depth of knowledge in pathophysiology, pharmacology, and advanced diagnostic reasoning. They don't just follow orders; they create and direct the plan of care.
Core Responsibilities Include:
- Advanced Assessment and Diagnosis: Performing comprehensive physical examinations, interpreting complex patient data from monitors, ventilators, and lab results, and diagnosing acute and chronic critical illnesses.
- Developing and Implementing Treatment Plans: Ordering and interpreting diagnostic tests (e.g., X-rays, CT scans, blood work), prescribing medications and therapies, and managing life-support equipment like mechanical ventilators, dialysis machines, and extracorporeal membrane oxygenation (ECMO).
- Performing Advanced Procedures: This is a key differentiator. Critical Care NPs are trained and credentialed to perform invasive procedures such as intubation, central line insertion, arterial line placement, chest tube insertion, and lumbar punctures.
- Collaboration and Leadership: Working as a vital member of the interdisciplinary team, which includes physicians, respiratory therapists, pharmacists, RNs, and other specialists. They often lead rounds, direct the flow of care for a cohort of patients, and serve as a primary point of contact for the team.
- Patient and Family Education and Counseling: The role extends beyond the patient to their families. A CCT NP is responsible for explaining complex medical conditions, discussing treatment options and prognosis, and providing compassionate support during times of extreme stress and grief.
### A Day in the Life of a Critical Care NP
To make this role more tangible, let's walk through a typical 12-hour shift in a Surgical ICU (SICU).
> 7:00 AM: Arrive and receive a detailed handoff report from the night-shift NP on your patient load (typically 4-8 patients). You review overnight events, vital sign trends, lab results, and any new imaging.
>
> 8:00 AM: Begin your first round of patient assessments. For a post-op heart surgery patient, this means a detailed cardiac and pulmonary exam, checking chest tube outputs, and reviewing ventilator settings. For a trauma patient, it involves a neurological assessment and checking for any signs of infection.
>
> 9:30 AM: Huddle with the bedside nurses to discuss the morning plan. You place orders for new medications, lab draws, and a stat chest X-ray for a patient with worsening oxygen levels.
>
> 10:00 AM: Interdisciplinary rounds begin. You present each of your patients to the team, led by the attending intensivist. You provide your assessment, discuss the plan, and field questions from pharmacy, respiratory therapy, and nutrition.
>
> 11:30 AM: A patient's blood pressure drops precipitously. You rush to the bedside, quickly assess the situation, and order fluid boluses and a vasopressor drip. You decide the patient needs a central line for better monitoring and medication delivery and perform the procedure yourself at the bedside using ultrasound guidance.
>
> 1:00 PM: Charting. Documentation in the ICU is meticulous. You document your assessments, procedures, and any changes to the plan of care for all your patients.
>
> 2:30 PM: Family meeting. You and the attending physician meet with the family of a patient with a severe brain injury to discuss the grim prognosis and transition to comfort care. This requires immense empathy and clear communication.
>
> 4:00 PM: A new admission arrives from the Emergency Department—a patient with septic shock. You perform the initial history and physical, place admission orders, and work to stabilize the patient, which includes managing fluids, antibiotics, and ventilator support.
>
> 6:30 PM: You complete your final patient rounds, ensuring all plans are in place for the night shift. You meticulously update your sign-out report for the oncoming NP, highlighting any ongoing issues or patients to watch closely.
>
> 7:30 PM: Handoff is complete. You leave the unit, mentally exhausted but fulfilled, knowing you made critical, life-altering decisions throughout your day.
---
Average Critical Care NP Salary: A Deep Dive
The financial compensation for a Critical Care NP reflects the high level of responsibility, extensive education, and specialized skills required for the role. Salaries are consistently robust and are among the highest within the nurse practitioner profession.
According to the U.S. Bureau of Labor Statistics (BLS), the median annual wage for all nurse practitioners was $128,490 as of May 2023. However, specialties like critical care that involve high acuity, procedural skills, and often non-traditional hours tend to command salaries on the higher end of this spectrum.
More specific, real-time data from salary aggregators confirms this trend.
- Salary.com reports that the average Critical Care Nurse Practitioner salary in the United States is $135,108 as of May 2024, with a typical salary range falling between $125,404 and $143,151.
- Payscale.com indicates a similar average base salary of approximately $122,548, with a total pay range (including bonuses and other compensation) extending from $98,000 to $158,000.
- Glassdoor lists the estimated total pay for a Critical Care Nurse Practitioner at $144,401 per year, combining a base salary of around $131,000 with additional pay like bonuses and profit sharing.
It's important to view these figures as a starting point. Your personal earning potential is influenced by a multitude of factors, most notably your years of experience.
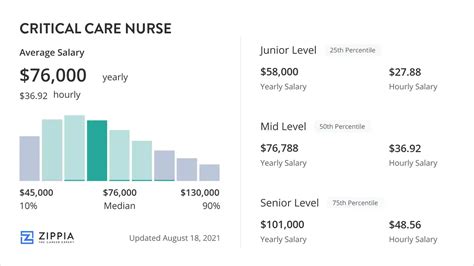
### Salary by Experience Level
Like most professions, compensation for Critical Care NPs grows significantly with experience. As you gain clinical confidence, procedural proficiency, and a reputation for excellent patient outcomes, your value to an organization increases dramatically.
| Experience Level | Typical Years of Experience | Average Annual Base Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $105,000 - $125,000 | Recently graduated and certified. Focus is on consolidating skills under mentorship. May require a longer orientation period. |
| Mid-Career | 3-9 Years | $125,000 - $145,000 | Proficient and autonomous clinician. Manages complex patients with confidence. Often precepts new NPs and participates in unit-based committees. |
| Senior/Experienced | 10+ Years | $145,000 - $170,000+ | Clinical expert and leader on the unit. May hold a formal leadership role (Lead NP), specialize in a highly technical area (e.g., ECMO), or be involved in research and quality improvement. |
*Source: Synthesized data from Salary.com, Payscale, and industry reports.*
### Beyond the Base Salary: Understanding Your Total Compensation Package
The annual salary is only one piece of the financial puzzle. The total compensation for a Critical Care NP is often substantially higher due to a variety of additional pay structures and benefits common in hospital settings. When evaluating a job offer, you must consider the entire package.
Key Components of Total Compensation:
- Base Salary: The guaranteed annual pay for a full-time position.
- Shift Differentials: This is a significant income booster. Hospitals pay a premium for working evenings, nights, weekends, and holidays. These differentials can add $5 to $15 per hour to your base rate, potentially increasing your annual income by $10,000 to $25,000 or more, depending on your schedule.
- On-Call Pay: Some positions require being on-call, for which you receive a small hourly stipend. If you are called in to work, you are then paid your full hourly rate, often with a guaranteed minimum number of hours.
- Overtime Pay: For hourly employees, any hours worked over 40 in a week (or over a certain number per pay period) are paid at 1.5 times the base rate. Salaried employees may receive a flat bonus or extra PTO for working significant extra hours.
- Sign-On Bonus: To attract top talent in a competitive market, hospitals frequently offer sign-on bonuses, which can range from $5,000 to $25,000, sometimes tied to a commitment to stay with the organization for a set period (e.g., two years).
- Performance or Quality Bonuses: An increasing number of health systems tie a portion of compensation to achieving specific quality metrics (e.g., reducing central line-associated bloodstream infections) or patient satisfaction scores. These annual bonuses can range from 2% to 10% of the base salary.
- Relocation Assistance: For candidates moving from another city or state, employers often provide a relocation package (typically $5,000 to $15,000) to cover moving expenses.
- Retirement Savings: This includes 401(k) or 403(b) plans. The employer match is critical—a common offering is a 50% match on the first 6% of your contribution, which is essentially free money.
- Paid Time Off (PTO): Generous PTO is standard, often starting at 4-5 weeks per year and increasing with seniority.
- Continuing Medical Education (CME): Employers provide an annual allowance (typically $1,500 to $3,500) and paid time off to attend conferences and workshops to maintain your certification and license.
- Tuition Reimbursement/Loan Forgiveness: Some non-profit hospitals and academic centers offer tuition assistance for further education (like pursuing a DNP) or are eligible for programs like Public Service Loan Forgiveness (PSLF).
When you combine a base salary of $135,000 with significant night/weekend differentials, a performance bonus, and a strong retirement match, the total value of a Critical Care NP's compensation package can easily approach $170,000 or more.
---
Key Factors That Influence a Critical Care NP Salary
While we've established a strong baseline salary, your individual earnings can vary significantly. Understanding the levers that control your pay is the first step toward maximizing your career-long earning potential. Let's dissect the seven most influential factors.
###
1. Level of Education and Certification
The minimum educational requirement to be a Critical Care NP is a Master of Science in Nursing (MSN) from an accredited Acute Care Nurse Practitioner program. However, the Doctor of Nursing Practice (DNP) is increasingly becoming a preferred terminal degree.
- MSN vs. DNP: For a purely clinical role, the immediate salary difference between an MSN-prepared NP and a DNP-prepared NP is often minimal, perhaps a few thousand dollars per year. The real value of the DNP emerges in long-term career trajectory. A DNP prepares you for leadership roles (e.g., Director of Advanced Practice Providers, Clinical Program Manager), academic positions, and high-level quality improvement and research initiatives, all of which command higher salaries. Think of the DNP as an investment in your future earning potential beyond the bedside.
- Essential Certification: The non-negotiable credential for this role is the Acute Care Nurse Practitioner Certification for Adults and Gerontology (ACNPC-AG), administered by the American Association of Critical-Care Nurses (AACN). Holding this certification is a prerequisite for licensure and employment.
- Additional Certifications: While not always leading to a direct pay bump, additional certifications showcase expertise and can make you a more competitive candidate. The most relevant for an experienced RN heading to NP school is the CCRN (Certification for Adult, Pediatric, or Neonatal Critical Care Nurses). As an NP, certifications in specific procedures (e.g., Registered Nurse in Vascular Access) or technologies can also add value.
###
2. Years of Experience
Experience is arguably the most significant driver of salary growth in this field. It's a direct proxy for clinical competence, speed, and judgment.
- The Novice Phase (0-2 years): In this stage, you're transitioning from the RN role and applying your new theoretical knowledge. You're fast, but not yet efficient. You know the "what," but you're still mastering the "why" and "when." Salaries are at the lower end of the spectrum ($105k - $125k) as the institution is investing heavily in your mentorship and development.
- The Competent/Proficient Phase (3-9 years): You've seen most common critical care scenarios multiple times. Your procedural skills are smooth, and your diagnostic reasoning is sharp. You can manage a full, complex patient load with minimal supervision and begin to act as a resource for newer NPs and RNs. This is where you see the most significant salary growth, with earnings firmly in the $125k - $145k range.
- The Expert Phase (10+ years): You are a clinical pillar of the ICU. You handle the rarest and most complex cases with an intuitive grasp of the situation. You lead quality improvement projects, mentor entire cohorts of new providers, and may have a specialized niche (e.g., the go-to NP for ECMO or post-transplant patients). Your salary reflects this expertise, pushing into the $145k - $170k+ range. You become eligible for lead NP roles which can add another $10,000 - $20,000 to your base pay.
###
3. Geographic Location
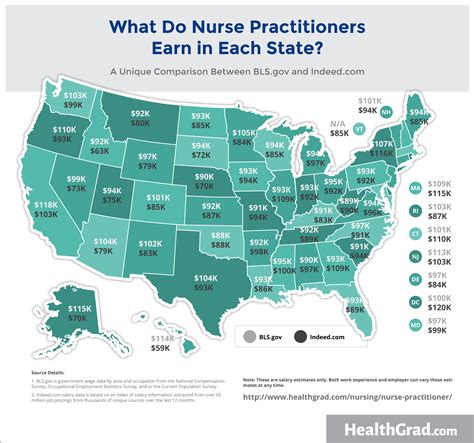
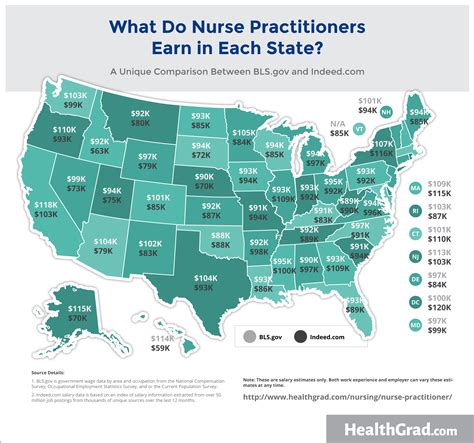
Where you work matters—a lot. Salaries for Critical Care NPs vary dramatically by state and even by metropolitan area, largely driven by cost of living and local market demand.
According to the BLS May 2023 data for all Nurse Practitioners, the top-paying states are:
| State | Annual Mean Wage for NPs | Notes on the Critical Care Market |
| :--- | :--- | :--- |
| California | $161,540 | High cost of living, but also high demand and union presence in some areas drive up wages significantly. Major metro areas like San Francisco and Los Angeles can see CCT NP salaries approaching or exceeding $200,000. |
| New Jersey | $147,380 | Proximity to NYC and Philadelphia, along with numerous major hospital systems, creates a competitive market. |
| Massachusetts | $146,120 | Home to many world-renowned academic medical centers, creating high demand for specialized NPs. High cost of living, particularly in Boston. |
| Oregon | $144,770 | Strong demand and a favorable practice environment for NPs contribute to high wages. |
| Nevada | $141,330 | A rapidly growing population and a competitive healthcare market, particularly in Las Vegas and Reno. |
Conversely, states in the Southeast and parts of the Midwest tend to have lower average salaries, though this is often offset by a significantly lower cost of living. For example, states like Alabama, Tennessee, and Missouri may have average NP salaries closer to the $105,000 - $115,000 range.
Key Takeaway: A $160,000 salary in San Francisco may provide a similar or even lower quality of life than a $130,000 salary in a city like St. Louis or Phoenix due to vast differences in housing costs, taxes, and daily expenses.
###
4. Work Setting / Type of Facility
The type of institution you work for has a profound impact on your salary, benefits, and day-to-day work environment.
- Large Academic Medical Centers: These are university-affiliated hospitals (e.g., Johns Hopkins, Mayo Clinic, UCLA Health).
- *Salary:* Often slightly *lower* or on par with the market average.
- *Pros:* Excellent benefits, pension plans, tuition remission for yourself and family, prestigious reputation, opportunities for research and teaching, exposure to cutting-edge medicine and highly complex cases. The non-monetary benefits are a huge draw.
- *Cons:* Can be more bureaucratic, potentially slower to adopt change.
- Large Private, Non-Profit Hospital Systems: These are the large community health systems that dominate most major metro areas (e.g., HCA Healthcare, Advocate Aurora Health, Providence).
- *Salary:* Often the most competitive, market-driven salaries. They need to attract and retain talent to compete.
- *Pros:* High patient volume, often very efficient systems, strong sign-on bonuses and relocation packages.
- *Cons:* Can be more corporate and business-focused, with pressure on metrics like patient throughput.
- Government/VA Hospitals: Working for the Department of Veterans Affairs or military hospitals.
- *Salary:* Follows a set government pay scale (GS scale), which is transparent and predictable. It may start lower but has regular step increases.
- *Pros:* Unbeatable federal benefits, including a generous pension, excellent job security, and often a better work-life balance. Any state license works at any VA facility.
- *Cons:* The bureaucracy can be significant, and salary potential may be capped compared to the private sector's highest earners.
- Locum Tenens (Temporary/Contract Work): Working for an agency that places you in hospitals for short-term assignments (e.g., 3-6 months) to fill staffing gaps.
- *Salary:* The highest hourly pay rates, often $100 - $150+ per hour. This is because the hospital is paying a premium for a flexible, immediate solution.
- *Pros:* Extremely high earning potential, flexibility to travel and choose assignments.
- *Cons:* No benefits (no PTO, retirement, health insurance—you must buy your own). Lack of stability, constant need to adapt to new systems and teams. It's a high-reward, high-risk path best suited for experienced NPs.
###
5. Area of Sub-Specialization within Critical Care
While all ICU work is complex, some sub-specialties are perceived as more technically demanding and may command a slight salary premium or offer more opportunities for overtime and specialized roles.
- Cardiothoracic ICU (CTICU/CVICU): Cares for patients after open-heart surgery, heart/lung transplants, and those on advanced support like ECMO and ventricular assist devices (VADs). This is often considered the most technically complex environment and may offer a slight pay advantage due to the high skill level required.
- Neuro ICU: Manages patients with severe strokes, brain bleeds, traumatic brain injuries, and post-neurosurgical procedures. Requires deep expertise in neurological assessment.
- Surgical/Trauma ICU (SICU/TICU): Cares for critically ill patients after major general surgery or severe traumatic injuries.
- Medical ICU (MICU): Manages patients with complex medical conditions like septic shock, acute respiratory distress syndrome (ARDS), and multi-organ failure.
- Pediatric ICU (PICU) / Neonatal ICU (NICU): These are entirely separate educational tracks (PNP-AC for pediatric) but follow similar salary principles. They are highly specialized and always in demand.
While a hospital might not have a different salary band for a MICU NP vs. a SICU NP, the CVICU NPs may have more opportunities for specialized roles (e.g., VAD coordinator, ECMO specialist) that come with additional stipends or higher pay grades.
###
6. In-Demand Skills and Procedural Competency
Your skillset is your currency. The more you can do, the more valuable you are. While core competencies are expected, certain high-level skills can increase your leverage during salary negotiations or qualify you for higher-paying positions.
High-Value Clinical Skills:
- Advanced Procedural Competence: Being the go-to provider for difficult intubations, ultrasound-guided line placements, or bronchoscopies.
- Expertise in Advanced Mechanical Support: Proficiency in managing technologies like ECMO, continuous renal replacement therapy (CRRT), and advanced ventilator modes.
- Point-of-Care Ultrasound (POCUS): Using ultrasound at the bedside for diagnostic purposes (e.g., cardiac echo, lung scans) is a rapidly growing skill that sets candidates apart.
High-Value Soft Skills:
- Leadership and Mentorship: Formally precepting new NPs or leading unit-based initiatives.
- Bilingualism: The ability to communicate directly with a diverse patient population (e.g., Spanish) is a huge asset in many parts of the country and can sometimes come with a pay differential.
- Data Analysis and Quality Improvement: Skills in analyzing unit data to improve patient outcomes are highly valued by hospital administration.
---
Job Outlook and Career Growth for Critical Care NPs

The professional forecast for Critical Care Nurse Practitioners is exceptionally bright. The demand for their skills is intense and projected to grow rapidly for the foreseeable future.
The U.S. Bureau of Labor Statistics (BLS) provides a stunning projection for the entire nurse practitioner profession. Employment of NPs is projected to grow 45 percent from 2022 to 2032, which is vastly faster than the average for all occupations. The BLS anticipates about 118,600 openings for nurse practitioners each year, on average, over the decade.
While the BLS doesn't separate data for the critical care specialty, several powerful trends ensure that CCT NPs will be at the forefront of this growth:
1. An Aging Population: The baby boomer generation is aging, leading to a higher prevalence of complex, chronic conditions that often result in critical illness. This