Introduction

In the high-stakes world of healthcare, few roles carry the same weight of responsibility, intellectual challenge, and profound human impact as the Critical Care Nurse Practitioner (CCNP). You are drawn to the place where medicine is at its most intense, where every decision can alter the course of a life, and where clinical expertise is not just valued—it's essential. This is a career for the calmest minds in the storm, the most compassionate hearts in the chaos. But beyond the immense personal and professional satisfaction, a career as a CCNP offers significant financial rewards. The average critical care nurse practitioner salary reflects the high level of skill, autonomy, and dedication required, often ranging from $115,000 to over $150,000 annually, with top earners and those in high-demand areas exceeding this considerably.
I once stood by the bedside of a family member in the ICU, overwhelmed by the beeping machines and the clinical jargon. It was the Critical Care Nurse Practitioner who sat with us, calmly and clearly explaining the complex physiology of what was happening, outlining the plan, and treating not just the patient, but our family's fear. In that moment, I witnessed the unique fusion of profound medical knowledge and deep-seated humanity that defines this role. It is a career that earns not just an impressive salary, but an unparalleled level of respect.
This comprehensive guide is designed to be your definitive resource, whether you are an experienced ICU nurse contemplating your next step or a student mapping out your future in advanced practice nursing. We will delve deep into every facet of the critical care nurse practitioner salary, explore the factors that shape your earning potential, and provide a clear, actionable roadmap to launching and advancing in this exceptional career.
### Table of Contents
- [What Does a Critical Care Nurse Practitioner Do?](#what-does-a-critical-care-nurse-practitioner-do)
- [Average Critical Care Nurse Practitioner Salary: A Deep Dive](#average-critical-care-nurse-practitioner-salary-a-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Become a Critical Care Nurse Practitioner](#how-to-become-a-critical-care-nurse-practitioner)
- [Conclusion: Is This Demanding Career Worth the Reward?](#conclusion-is-this-demanding-career-worth-the-reward)
---
What Does a Critical Care Nurse Practitioner Do?

A Critical Care Nurse Practitioner, often certified as an Adult-Gerontology Acute Care Nurse Practitioner (AG-ACNP), is an advanced practice registered nurse (APRN) who specializes in providing comprehensive care to patients who are critically ill or unstable. They are key leaders within the Intensive Care Unit (ICU) and other critical care settings, functioning with a high degree of autonomy and working collaboratively with physicians, specialists, nurses, respiratory therapists, and other members of the healthcare team.
Unlike a bedside ICU Registered Nurse (RN), whose role is primarily focused on carrying out the plan of care, the CCNP is instrumental in *creating* and *managing* that plan. Their scope of practice bridges the gap between nursing and medicine, allowing them to diagnose conditions, order and interpret diagnostic tests, prescribe medications, and perform complex procedures.
Core responsibilities are extensive and require a sophisticated understanding of pathophysiology, pharmacology, and evidence-based practice. These tasks frequently include:
- Performing Comprehensive Assessments: Conducting advanced physical examinations and taking detailed health histories of critically ill patients.
- Diagnosing and Managing Conditions: Identifying and managing complex acute, critical, and chronic illnesses, such as sepsis, acute respiratory distress syndrome (ARDS), multi-organ failure, and cardiogenic shock.
- Ordering and Interpreting Diagnostics: Ordering and analyzing a wide array of tests, including lab work, imaging studies (X-rays, CT scans), and hemodynamic monitoring data.
- Prescribing and Titrating Medications: Managing complex medication regimens, including potent vasoactive drips, sedatives, antibiotics, and other critical care drugs.
- Performing Advanced Procedures: Depending on state regulations and hospital credentialing, CCNPs may perform invasive procedures such as intubation, central venous line placement, arterial line insertion, and thoracentesis.
- Leading Patient Care Rounds: Presenting patients to the interdisciplinary team, synthesizing data, and formulating the daily plan of care.
- Patient and Family Education: Communicating complex medical information, treatment options, and prognoses to patients and their families with empathy and clarity.
- Collaborating and Consulting: Working closely with attending physicians, consulting specialists (e.g., cardiologists, nephrologists), and other team members to ensure coordinated, high-quality care.
### A Day in the Life of a CCNP
To make this role more tangible, let's follow a fictional CCNP, Alex, through a typical 12-hour day shift in a busy Medical ICU (MICU).
- 7:00 AM - Handoff: Alex arrives and receives a detailed report from the night-shift NP on their shared caseload of 6-8 critically ill patients. They discuss overnight events, any changes in patient status, and pending lab results.
- 8:00 AM - Pre-Rounds and Chart Review: Alex meticulously reviews each patient's chart, analyzing new lab values, imaging reports, vital sign trends, and ventilator settings. They quickly see each patient to perform a focused physical assessment.
- 9:30 AM - Interdisciplinary Rounds: Alex leads the discussion for their patients during rounds with the attending physician, bedside nurses, pharmacist, and respiratory therapist. They present a concise summary of each case and propose a detailed plan for the day, including medication adjustments, diagnostic tests, and ventilator changes.
- 11:00 AM - A "Rapid Response" Call: A rapid response is called on a patient on a different floor who is deteriorating. Alex responds, quickly assesses the patient for septic shock, orders a fluid bolus and antibiotics, and arranges for immediate transfer to the ICU.
- 12:30 PM - Procedures: After the new patient is settled, Alex performs a central line placement under ultrasound guidance to allow for the safe administration of vasopressors.
- 2:00 PM - Family Meeting: Alex meets with the family of a long-term patient to discuss their deteriorating prognosis and to facilitate a difficult conversation about goals of care and a potential transition to comfort measures.
- 4:00 PM - Patient Management: The afternoon is spent managing the ongoing needs of the patient panel—titrating sedation, responding to an arrhythmia, interpreting a chest X-ray, and consulting with nephrology about a patient's acute kidney injury.
- 6:30 PM - Documentation and Handoff: Alex completes their progress notes for the day, ensuring all orders and care plans are clearly documented. They prepare a thorough sign-out for the incoming night-shift NP, highlighting key concerns and tasks to be followed up overnight.
- 7:30 PM - Departure: Alex leaves the unit, mentally exhausted but fulfilled, knowing their expertise was critical in managing multiple complex and life-threatening situations.
---
Average Critical Care Nurse Practitioner Salary: A Deep Dive
The financial compensation for a Critical Care Nurse Practitioner is a direct reflection of the advanced education, specialized skill set, and immense responsibility the role entails. While salaries can vary significantly based on a multitude of factors, the earning potential is consistently strong and places CCNPs among the highest-paid professionals in the nursing field.
It's important to note that the U.S. Bureau of Labor Statistics (BLS) groups all nurse practitioners together in its data. For the broader category of "Nurse Anesthetists, Nurse Midwives, and Nurse Practitioners," the BLS reported a median annual wage of $125,900 as of May 2022. However, specialized fields like critical care often command salaries at the higher end of this spectrum due to the intensity and complexity of the work.
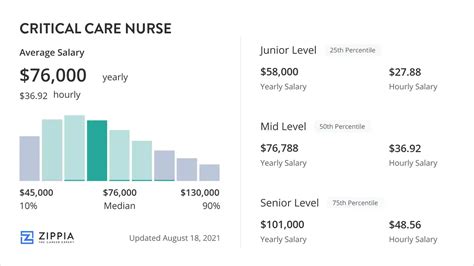
To get a more precise picture of the critical care nurse practitioner salary, we must turn to specialized salary aggregators that account for the nuances of this specific role.
### National Averages and Salary Ranges
Based on an analysis of several authoritative sources, the national average base salary for a Critical Care Nurse Practitioner typically falls within a well-defined range.
- Salary.com reports that the median salary for a Nurse Practitioner - Critical Care in the United States is $129,571 as of late 2023. The typical salary range falls between $120,240 and $137,280. However, the full salary spectrum, including the top 10% of earners, can extend well beyond $145,000 for base pay alone.
- Payscale.com provides data for Acute Care Nurse Practitioners (ACNPs), the certification track for CCNPs. It reports an average salary of approximately $112,656 per year. Their data shows a range from roughly $93,000 for early-career professionals to over $138,000 for highly experienced CCNPs.
- Glassdoor lists the average total pay (including bonuses and other compensation) for a Critical Care Nurse Practitioner at around $139,833 per year, with a likely range between $118,000 and $167,000.
Synthesizing this data, a realistic expectation for a CCNP in the United States is a starting base salary in the low six figures (around $105,000-$115,000) and an average mid-career salary in the $125,000 to $140,000 range.
### Salary Progression by Experience Level
Experience is one of the most significant drivers of salary growth in this field. As a CCNP gains procedural skills, clinical confidence, and the ability to manage more complex patients with greater autonomy, their value to an organization—and their compensation—increases accordingly.
Here is a typical salary progression you can expect throughout your career:
| Experience Level | Typical Years of Practice | Average Annual Base Salary Range | Key Milestones & Responsibilities |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $105,000 - $120,000 | Focus on foundational skills, working under closer supervision, mastering common ICU procedures and protocols. |
| Mid-Career | 3-9 Years | $120,000 - $138,000 | Increased autonomy, managing a full and complex patient load, precepting new NPs, participating in unit-based committees. |
| Senior/Experienced | 10-19 Years | $135,000 - $150,000+ | Seen as a clinical expert, leading quality improvement projects, potential for team lead or management roles, high procedural proficiency. |
| Late-Career | 20+ Years | $140,000 - $165,000+ | Often in leadership (e.g., Director of Advanced Practice), academia, or highly specialized clinical roles. Top-tier clinical and institutional knowledge. |
*Source: Data synthesized from Salary.com, Payscale, and industry observations.*
### Beyond the Base Salary: Understanding Total Compensation
A CCNP's base salary is only one part of their overall financial picture. A comprehensive compensation package often includes several other valuable components that can significantly increase total earnings.
- Shift Differentials: This is a major factor in critical care. Working nights, weekends, and holidays almost always comes with a pay differential, which can add $4 to $15 per hour to the base rate. Over a year, this can easily add $10,000-$20,000 to total pay.
- On-Call Pay: Some positions require CCNPs to be on-call for emergencies or procedures. This is typically compensated with a small hourly rate for being available, and a higher, often overtime, rate if called in.
- Bonuses:
- Sign-On Bonus: To attract talent in a competitive market, hospitals often offer sign-on bonuses ranging from $5,000 to $25,000 or more, sometimes tied to a commitment of 2-3 years.
- Performance/Quality Bonuses: Increasingly common, these bonuses are tied to meeting specific metrics related to patient outcomes, quality of care, or patient satisfaction.
- Retention Bonuses: Offered to experienced, valued CCNPs to encourage them to stay with the organization.
- Overtime Pay: While many NP positions are salaried (exempt), some are hourly (non-exempt), making them eligible for time-and-a-half pay for any hours worked over 40 per week. Given the nature of critical care, overtime opportunities are common.
- Benefits Package: This is a crucial, non-cash part of compensation. A strong benefits package can be worth tens of thousands of dollars and typically includes:
- Health Insurance: Comprehensive medical, dental, and vision coverage.
- Retirement Savings: 401(k) or 403(b) plans, often with a generous employer match.
- Paid Time Off (PTO): Vacation days, sick leave, and holiday pay.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $1,500 - $3,000) and paid time off to attend conferences and maintain licensure.
- Tuition Reimbursement: Support for pursuing a Doctor of Nursing Practice (DNP) or other advanced degrees.
- Malpractice Insurance: Provided by the employer.
When evaluating a job offer, it is essential to look beyond the base salary and calculate the value of the entire compensation and benefits package to understand your true earning potential.
---
Key Factors That Influence Your Salary
While national averages provide a useful benchmark, your individual critical care nurse practitioner salary will be determined by a complex interplay of several key factors. Understanding these variables is crucial for maximizing your earning potential throughout your career. This section will provide an exhaustive breakdown of what drives CCNP compensation.
###
1. Level of Education and Certification
The educational foundation for a CCNP is a graduate degree, but the specific degree and certifications held can impact salary and career trajectory.
- MSN vs. DNP: The two primary educational paths are the Master of Science in Nursing (MSN) and the Doctor of Nursing Practice (DNP).
- MSN (Master of Science in Nursing): This has historically been the standard degree for NP practice. It provides the essential clinical training and knowledge to pass the board exam and practice effectively.
- DNP (Doctor of Nursing Practice): The DNP is a terminal practice doctorate focused on translating research into practice, systems leadership, and quality improvement. While a DNP may not automatically translate to a higher salary for a purely clinical role at the *start* of a career, it is increasingly preferred for leadership and academic positions. Over time, DNP-prepared CCNPs may have a higher lifetime earning potential as they are better positioned for roles like Director of Advanced Practice Providers, clinical faculty positions, or research-focused roles, which often come with higher salaries. Some healthcare systems offer a small, built-in salary differential (e.g., an additional $5,000-$10,000 per year) for doctorate-prepared providers.
- Board Certification: To practice as a CCNP, you must pass a national board certification exam. The primary certification for this role is the Adult-Gerontology Acute Care Nurse Practitioner (ACNPC-AG) offered by the American Association of Critical-Care Nurses (AACN). This certification is not just a formality; it is a mandatory credential that validates your expertise and is a prerequisite for state licensure and hospital credentialing. It is the baseline requirement for earning a CCNP salary.
- Additional Certifications: While the ACNPC-AG is essential, holding additional certifications can demonstrate a deeper level of expertise and make you a more attractive candidate, potentially leading to higher pay or specialized roles.
- CCRN (Critical Care Registered Nurse): Most CCNPs hold this certification from their time as an ICU RN. Maintaining it demonstrates continued commitment and foundational expertise.
- CMC/CSC (Cardiac Medicine/Surgery Certification): For those specializing in cardiovascular ICUs, these subspecialty certifications are highly regarded.
- Procedure-Specific Certifications: Certifications in areas like advanced ultrasound use can also add value.
###
2. Years of Experience
As detailed in the previous section, experience is perhaps the single most powerful factor in salary growth. The trajectory is not linear but grows in stages as you move from novice to expert.
- 0-2 Years (The Foundation Stage): In this phase, your primary value is your potential. You are learning the workflow, building procedural confidence, and solidifying your diagnostic skills. Your salary will be at the lower end of the scale for the profession, but you can expect annual cost-of-living or merit increases.
- 3-9 Years (The Competent/Proficient Stage): You are now a fully independent and highly valuable member of the ICU team. You can manage a diverse and complex patient load with minimal oversight. This is where you see the most significant salary growth. You are now in a position to negotiate for higher pay based on your proven track record. According to Payscale, an experienced ACNP with 10-19 years of experience can earn an average of $123,000, showcasing the clear upward trend.
- 10+ Years (The Expert/Leadership Stage): With a decade or more of experience, you are a clinical authority. Your salary reflects your deep expertise, efficiency, and ability to mentor others. You may take on formal or informal leadership roles, such as team lead, preceptor, or project manager for quality improvement initiatives. At this stage, your salary should be in the top 25th percentile for the profession, often exceeding $140,000 - $150,000 in base pay, especially in high-paying regions.
###
3. Geographic Location
Where you choose to practice will have a dramatic impact on your salary. This variation is driven by local market demand, cost of living, and state regulations regarding NP scope of practice.
- Top-Paying States: States with a high cost of living, strong union presence, and favorable scope-of-practice laws for NPs tend to offer the highest salaries. According to BLS data for all NPs (which serves as a strong indicator), the top-paying states include:
1. California: (Annual Mean Wage: $158,130)
2. New Jersey: (Annual Mean Wage: $143,250)
3. Massachusetts: (Annual Mean Wage: $138,700)
4. Oregon: (Annual Mean Wage: $136,250)
5. New York: (Annual Mean Wage: $133,940)
A CCNP in a major metropolitan area like San Francisco, New York City, or Boston could realistically command a salary well over $160,000 - $180,000.
- Lower-Paying States: Conversely, states with a lower cost of living, particularly in the Southeast and parts of the Midwest, tend to have lower average salaries. For example, states like Alabama, Tennessee, and Arkansas often report average NP salaries below the national median. However, it is crucial to balance salary with the cost of living. A $120,000 salary in a low-cost area may provide more disposable income than a $145,000 salary in a high-cost coastal city.
- Metropolitan vs. Rural Areas: Salaries are typically highest in major metropolitan areas due to higher demand and cost of living. However, rural or underserved areas may offer significant financial incentives to attract providers, such as substantial sign-on bonuses, student loan repayment programs (like the NHSC Loan Repayment Program), and housing assistance. These benefits can sometimes offset a lower base salary.
###
4. Work Setting (Type of Employer)
The type of facility you work for is another critical determinant of your salary and overall compensation package.
- Large Academic Medical Centers / University Hospitals: These institutions are often at the top of the pay scale. They are typically located in major cities, are often unionized, and have well-defined clinical ladders and pay grades. They also offer excellent benefits, CME allowances, and opportunities for teaching and research. A CCNP at a major university hospital in a high-cost city could be one of the highest earners in the field.
- Large Private or Non-Profit Health Systems: These systems are highly competitive with academic centers and often offer very similar salary and benefits packages. They may offer more clinical-track positions without the academic responsibilities.
- Community Hospitals: Salaries at smaller community hospitals can be more variable. While they may not reach the peaks of major academic centers, they can be very competitive, particularly if they are trying to attract highly skilled providers away from larger cities. They may offer a better work-life balance and a strong sense of community.
- Government/VA Hospitals: Working for the Department of Veterans Affairs (VA) or other government entities means you are a federal employee. Salaries are based on a transparent General Schedule (GS) pay scale, which is adjusted for locality. VA positions offer exceptional benefits, including a generous pension plan (FERS), robust job security, and more PTO than most private sector jobs.
- Locum Tenens: This is a unique career path where a CCNP works as an independent contractor, taking on temporary assignments that can last from a few weeks to several months. Locum tenens work offers the highest hourly pay rates in the profession, often $100 - $150 per hour or more. This is because the rate includes compensation for benefits, malpractice insurance, and the instability of contract work. It's an excellent option for experienced CCNPs seeking flexibility and maximum income, but it lacks the stability and benefits of a permanent position.
###
5. Area of Specialization within Critical Care
While all CCNPs work with critically ill patients, sub-specializing within the ICU can sometimes lead to slightly higher pay due to the complexity and demand for specific skills.
- Cardiothoracic ICU (CTICU): This is often considered one of the most demanding and highest-skilled areas. Managing post-operative open-heart surgery patients, ventricular assist devices (VADs), and extracorporeal membrane oxygenation (ECMO) requires a highly specialized skill set that can command a premium salary.
- Surgical Trauma ICU (STICU): Specializing in the care of complex trauma and post-operative surgical patients also requires advanced skills and procedural competency, making it a high-demand specialty.
- Neuro ICU: Managing patients with acute strokes, brain hemorrhages, and traumatic brain injuries is another highly specialized field.
- Medical ICU (MICU): While considered a more "generalist" critical care role, it involves managing a wide breadth of complex medical conditions like sepsis and ARDS and remains a core, high-paying specialty.
###
6. In-Demand Skills and Procedural Competency
Your tangible, hands-on skills directly correlate with your value. A CCNP who is proficient in a wide range of invasive procedures and advanced technologies is more valuable than one who is not. Skills that boost your salary potential include:
- Advanced Procedural Skills: Documented competency in intubation, central and arterial line placement, chest tube insertion, and paracentesis makes you a highly efficient and autonomous provider, which hospitals will pay for.
- Advanced Ventilator Management: Deep expertise in managing complex ventilator modes, troubleshooting, and applying ARDSnet protocols.
*