The flashing lights, the controlled chaos, the split-second decisions that alter the course of a human life—the world of an Emergency Medicine (EM) physician is one of high stakes and immense responsibility. For those drawn to this intense, fast-paced specialty, the rewards are not just emotional and intellectual but also financial. The career promises a significant income, reflecting the extensive training, unique skills, and the critical nature of the work. But what does an `emergency med doctor salary` actually look like? The answer is far more complex than a single number. It's a dynamic figure shaped by experience, geography, practice setting, and a host of other factors.
I remember standing in a bustling emergency department waiting room years ago, a family member's hand in mine, my anxiety a palpable hum. A physician emerged, her expression a perfect blend of calm authority and empathy, and in a few short minutes, she cut through the fear with clarity and a decisive plan. It was a masterclass in grace under pressure, a profound demonstration of the value this profession brings to society’s most vulnerable moments.
This comprehensive guide is designed to cut through the noise and provide a definitive, data-driven look at the compensation, career trajectory, and future of Emergency Medicine. We will dissect every component of an ER doctor's earnings, explore the factors that can maximize your income, and lay out a clear roadmap for aspiring physicians. Whether you are a pre-med student, a medical resident, or a practicing physician considering a change, this article is your ultimate resource.
### Table of Contents
- [What Does an Emergency Medicine Doctor Do?](#what-do-they-do)
- [Average Emergency Medicine Doctor Salary: A Deep Dive](#deep-dive)
- [Key Factors That Influence Salary](#key-factors)
- [Job Outlook and Career Growth](#job-outlook)
- [How to Get Started in This Career](#how-to-start)
- [Conclusion: Is a Career in Emergency Medicine Right for You?](#conclusion)
What Does an Emergency Medicine Doctor Do?

An Emergency Medicine physician is the ultimate medical generalist, a master of immediate intervention and diagnosis. They are the frontline providers in the healthcare system, treating a vast spectrum of illnesses and injuries, from sore throats and broken bones to heart attacks, strokes, and severe trauma. Their "office" is the emergency department (ED), a dynamic and unpredictable environment where no two shifts are ever the same.
The core of their role is to rapidly assess, stabilize, and treat patients with acute medical conditions. This requires a broad and deep knowledge base covering nearly every medical specialty—cardiology, pulmonology, neurology, orthopedics, pediatrics, and more. They must be able to recognize life-threatening conditions within minutes and initiate life-saving procedures without hesitation.
Core Responsibilities and Daily Tasks:
- Triage and Assessment: Working with nurses to quickly evaluate the severity of a patient's condition and prioritize care. This involves taking a rapid, focused history and performing a physical examination.
- Diagnosis: Ordering and interpreting a wide array of diagnostic tests, including blood work, X-rays, CT scans, and ultrasounds. A key skill is point-of-care ultrasound (POCUS), where the physician performs the ultrasound at the bedside for immediate answers.
- Treatment and Stabilization: Prescribing medications, administering fluids, and managing life support. They treat everything from sepsis and diabetic ketoacidosis to respiratory failure and overdoses.
- Performing Procedures: EM physicians are proceduralists. Common procedures include:
- Airway Management: Intubation (placing a breathing tube).
- Trauma Care: Placing chest tubes, managing bleeding, and performing resuscitation.
- Wound Care: Suturing lacerations and draining abscesses.
- Orthopedics: Reducing dislocations and splinting fractures.
- Cardiac Care: Performing CPR, defibrillation, and cardioversion.
- Communication and Coordination: The EM doctor is the hub of communication. They speak with patients and their families, consult with specialists (cardiologists, surgeons, neurologists), and coordinate with nurses, technicians, and social workers to ensure seamless patient care.
- Disposition: Deciding the next step for every patient. This could be admission to the hospital, transfer to a specialized facility (like a trauma or stroke center), or discharge home with follow-up instructions.
### A "Day in the Life" of an Emergency Medicine Doctor
To make this tangible, consider a typical 8-hour shift:
- 6:45 AM: Arrive at the hospital, grab a coffee, and head to the ED.
- 7:00 AM: "Sign-out." The overnight physician provides a detailed report on all current patients in the department—who is stable, who is waiting for tests, and who is critically ill. You take responsibility for a dozen or more patients instantly.
- 7:15 AM: Your first new patient is an elderly man with chest pain. You immediately order an EKG, blood work, and a chest X-ray, all while assessing him for signs of a heart attack.
- 8:30 AM: A call comes in from paramedics: "25-year-old male, multi-vehicle collision, unstable." The trauma bay is activated. You lead the team as the patient arrives, performing a rapid assessment (the "ABCs" - Airway, Breathing, Circulation), using the ultrasound to check for internal bleeding, and ordering life-saving blood transfusions.
- 10:00 AM: While the trauma patient is being stabilized and prepped for surgery, you simultaneously manage other patients: a child with a high fever, a patient with a severe asthma attack, and someone with a dislocated shoulder. You deftly switch contexts, giving orders and performing a procedural sedation to pop the shoulder back into place.
- 12:30 PM: You find a 10-minute window to sit and "chart." Meticulous documentation is crucial for patient care, billing, and legal protection. You wolf down a protein bar while typing.
- 1:30 PM: The patient with chest pain is diagnosed with a dangerous heart rhythm. You consult with the on-call cardiologist and start medication to stabilize him before he's admitted to the cardiac care unit.
- 2:45 PM: The waiting room is full. You work with the charge nurse to improve patient flow, seeing and treating patients as efficiently and safely as possible.
- 3:00 PM: "Sign-out." You meticulously transfer care of all your patients to the incoming evening physician, ensuring a safe handoff.
- 3:30 PM: You leave the hospital, mentally replaying the critical cases from the day. The intensity is draining, but the feeling of having made a direct, tangible difference is the reason you chose this field.
This cycle of intense activity, multitasking, and critical decision-making defines the profession. It requires resilience, adaptability, and an unshakeable ability to remain calm in the face of chaos.
Average Emergency Medicine Doctor Salary: A Deep Dive
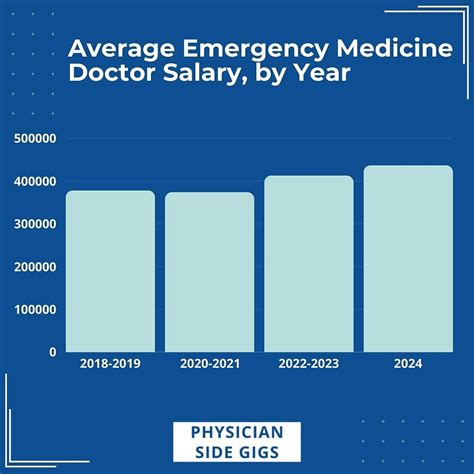
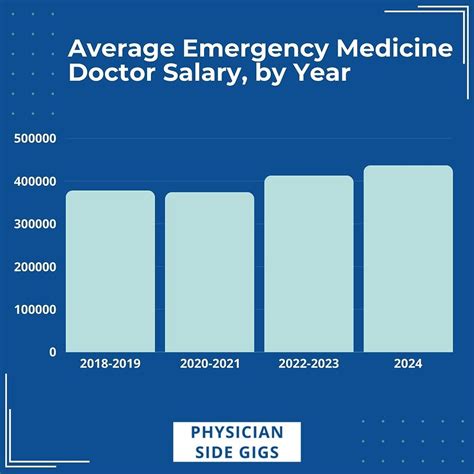
Emergency Medicine is consistently ranked among the higher-paying physician specialties, a reflection of the stressful environment, unsociable hours (nights, weekends, holidays), and the high-stakes nature of the work. However, the "average" salary can be misleading, as it is influenced by numerous factors we will explore in the next section.
To establish a baseline, we'll consult the most reputable, up-to-date sources in the medical industry. It's important to note that different surveys use different methodologies, which can lead to variations in their data.
National Average and Salary Range
The most trusted industry reports place the average emergency med doctor salary well into the six-figure range, typically between $340,000 and $450,000 per year.
- Doximity 2023 Physician Compensation Report: This highly-regarded report, based on data from over 190,000 U.S. physicians, lists the average annual compensation for Emergency Medicine physicians as $398,000.
- Medscape Physician Compensation Report 2023: Another industry standard, Medscape's report found the average salary for EM physicians to be $352,000. The report notes this is a slight decrease from previous years, reflecting some market shifts.
- Salary.com: This aggregator, which analyzes employer-reported data, shows a tighter median salary for an "Emergency Room Physician" at $355,101, with a typical range falling between $299,634 and $401,988 as of early 2024.
- U.S. Bureau of Labor Statistics (BLS): The BLS provides broader categories. For "Physicians and Surgeons, All Other," which includes emergency physicians, the median annual wage was $239,200 in May 2022. However, the BLS also states that wages for specialists in this category often "exceed the median wage," which is consistent with the more specific industry reports.
Taking these sources together, a realistic national average for an experienced Emergency Medicine physician is approximately $375,000 per year. The salary range is vast, with entry-level (post-residency) physicians potentially starting in the high $200s, while highly experienced physicians in lucrative locations or partnership models can earn well over $500,000.
### Salary by Experience Level
Salary in medicine is not static; it grows significantly with experience, efficiency, and responsibility. Here’s a typical progression:
| Experience Level | Years Post-Residency | Typical Annual Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level | 1-3 years | $280,000 - $350,000 | Focus is on gaining speed, confidence, and efficiency. Often paid a straight hourly rate or salary. |
| Mid-Career | 4-10 years | $350,000 - $450,000 | Physicians are highly efficient, see more patients per hour, and may take on leadership or teaching roles. More likely to be on productivity-based pay. |
| Senior/Experienced | 11+ years | $400,000 - $550,000+ | Often in partnership tracks or department leadership roles (e.g., Medical Director). Peak earning potential. May diversify into administration or consulting. |
*(Note: These are estimates based on aggregated industry data and can vary significantly based on the factors discussed below.)*
### A Deeper Look at Compensation Components
An EM physician’s total compensation is rarely just a flat salary. The structure is often complex and designed to incentivize productivity and quality.
- Base Salary vs. Hourly Rate: Many EM physicians are paid an hourly rate rather than an annual salary. A typical full-time schedule is between 120 and 140 hours per month. A rate of $200/hour for 130 hours/month equates to an annual base of $312,000. Rates can range from $150/hour in some academic centers to over $300/hour for locum tenens or in high-demand rural areas.
- Productivity-Based Pay (RVUs): This is a critical component. Relative Value Units (RVUs) are a standardized measure used by Medicare to determine how much to pay physicians for their services. Each patient encounter is assigned an RVU value based on its complexity. Many compensation models include a base hourly rate plus a bonus for generating RVUs above a certain threshold. An efficient doctor who can see and treat more complex patients will generate more RVUs and thus earn a higher income.
- Bonuses and Incentives:
- Signing Bonus: To attract talent, hospitals and physician groups often offer significant signing bonuses, ranging from $20,000 to $50,000 or more, sometimes tied to a multi-year commitment.
- Quality Metrics Bonus: A growing trend is to tie a portion of compensation to quality metrics, such as patient satisfaction scores (HCAHPS), door-to-doctor time, or adherence to specific treatment protocols (e.g., for sepsis or stroke).
- Relocation Allowance: A stipend provided to help cover the costs of moving for a new job.
- Profit Sharing / Partnership Track: In private, physician-owned democratic groups, doctors can become partners after a few years. This means they share in the profits of the group, which can lead to significantly higher income than being a salaried employee. This also comes with administrative and business responsibilities.
- Benefits Package: The value of the benefits package should not be underestimated and can be worth tens of thousands of dollars annually. This includes:
- Health, Dental, and Vision Insurance: Often fully or heavily subsidized.
- Retirement Plans: 401(k) or 403(b) plans with employer matching contributions are standard.
- Malpractice Insurance: Typically covered by the employer, a major expense if paid independently. "Tail coverage," which covers claims made after the physician leaves the practice, is a crucial negotiation point.
- Continuing Medical Education (CME) Stipend: An annual allowance (e.g., $3,000 - $5,000) to pay for conferences, courses, and materials needed to maintain medical licenses and board certification.
- Paid Time Off (PTO): While seemingly standard, in an hourly model, "paid time off" may simply mean flexibility in scheduling, not payment for hours not worked. This is a key detail to clarify in any contract.
Understanding these components is essential to accurately evaluating a job offer. A lower base salary with a strong RVU incentive and partnership track might be far more lucrative long-term than a high-salaried position with no upside.
Key Factors That Influence an Emergency Medicine Doctor Salary

The national average provides a starting point, but an individual physician's earnings are determined by a complex interplay of personal and market factors. This section dissects the most significant drivers of an `emergency med doctor salary`, providing the detailed insight needed to navigate the job market strategically.
###
Level of Education and Specialization
In medicine, the foundational education is extensive and non-negotiable, but advanced training can create distinct career paths and salary potentials.
- MD vs. DO: All practicing Emergency Medicine physicians in the United States must hold a doctorate degree, either a Doctor of Medicine (MD) or a Doctor of Osteopathic Medicine (DO). After completing residency and becoming board-certified, the distinction has virtually no impact on salary or scope of practice.
- Residency: The mandatory 3-4 year Emergency Medicine residency is where physicians gain their specialized skills. The length of the residency (three vs. four years) does not typically have a direct, long-term impact on salary, although some argue four-year programs provide more advanced training.
- Board Certification: To be a credible candidate for most jobs, a physician must be board-certified by the American Board of Emergency Medicine (ABEM) or the American Osteopathic Board of Emergency Medicine (AOBEM). Being "board-eligible" (having finished residency but not yet passed the exams) is acceptable for initial hiring, but certification is expected and required for long-term employment and higher pay.
- Fellowship Sub-specialization: This is the most significant educational differentiator. After residency, a physician can pursue a 1-2 year fellowship to become an expert in a specific niche. While this means another year or two of lower (fellowship-level) pay, it can lead to higher long-term earnings, more desirable jobs, and leadership roles. Key fellowships include:
- Critical Care Medicine: These physicians can work in both the ED and the Intensive Care Unit (ICU), a highly valuable and well-compensated dual skill set.
- Pediatric Emergency Medicine (PEM): PEM specialists are sought after by children's hospitals and large academic centers, which often offer competitive salaries and a different practice environment.
- Ultrasound: An ultrasound fellowship can lead to a role as an Ultrasound Director for an ED, a position that often comes with an administrative stipend and higher pay.
- Toxicology: Medical toxicologists consult on poisonings and overdoses and may have joint appointments with poison control centers, leading to unique income streams.
- Sports Medicine: This can lead to a hybrid practice of seeing patients in both the ED and a sports medicine clinic.
###
Years of Experience
As detailed in the previous section, experience is a primary driver of income growth in Emergency Medicine. This is not simply a reward for loyalty; it's a reflection of tangible value.
- Efficiency and Throughput (The RVU Engine): An experienced physician is simply faster. They can diagnose and treat common complaints more quickly, perform procedures more efficiently, and manage multiple critically ill patients with less cognitive load. In a productivity-based system, this directly translates to higher earnings. A physician in year ten might see 2.5-3 patients per hour, while a new graduate might average 1.5-2.
- Leadership and Administrative Roles: With experience comes the opportunity for leadership. Senior physicians are often tapped for roles like:
- Medical Director / Department Chair: This is a major leadership position responsible for the administrative and clinical operations of the entire emergency department. It comes with a significant administrative stipend, often adding $50,000 to $150,000+ to their clinical income.
- Associate Director, Quality Director, or Informatics Director: These roles focus on specific areas of departmental management and also include stipends.
- Partnership: In private physician groups, experience is the pathway to partnership. Becoming a partner means moving from employee to owner, with a direct share in the group's profits. This typically represents the highest earning potential in the field.
###
Geographic Location
Where you practice is arguably the single biggest determinant of your salary. The variation between states and even between urban and rural areas within the same state can be over $100,000 per year.
The principle is basic supply and demand. Areas with a high cost of living and a large supply of physicians (e.g., major coastal cities like Boston, San Francisco, New York) tend to have lower salaries. Conversely, less "desirable" rural areas or states with a physician shortage must offer higher compensation to attract and retain talent.
Highest-Paying States/Regions (Generally):
According to various industry reports, states in the Southeast, Midwest, and Mountain West often offer the most competitive salaries. Examples of high-paying states include:
1. Wisconsin
2. Indiana
3. Georgia
4. Connecticut
5. Texas
Lowest-Paying States/Regions (Generally):
States in the Northeast and on the West Coast tend to have lower average salaries, though this is often offset by a different lifestyle or proximity to major academic institutions.
1. Maryland
2. Colorado
3. Massachusetts
4. California
Urban vs. Rural vs. Suburban:
- Rural: This is often where the highest hourly rates are found. A hospital in a rural community may offer a rate of $250-$300/hour or more, plus housing stipends and loan repayment options, to attract a physician.
- Suburban: These positions often represent a sweet spot. They are typically busy, high-volume community hospitals with a good patient mix. Salaries are very competitive, often exceeding those in the nearby urban core.
- Urban/Academic: Major city hospitals, especially university-affiliated academic medical centers, tend to pay the least. The trade-off is the prestige, research and teaching opportunities, and access to cutting-edge medicine.
###
Practice Model and Employer Type
The type of group or hospital you work for dramatically impacts your compensation structure, autonomy, and long-term potential.
- Private Democratic Physician Groups: Historically the dominant model, these are groups owned and run by the physicians themselves.
- Pros: High earning potential (partnership track), full transparency in finances, direct say in how the department is run.
- Cons: Requires a partnership buy-in, includes business responsibilities ("sweat equity"), income can fluctuate with patient volume and payer mix.
- Large Contract Management Groups (CMGs): These are large, national corporations (e.g., TeamHealth, Envision Healthcare) that contract with hospitals to staff their emergency departments.
- Pros: Often higher starting salaries, significant signing bonuses, broad geographic mobility (easy to move between company-staffed hospitals), strong benefits.
- Cons: Less autonomy, potential for corporate-driven metrics to influence medical practice, no partnership or ownership stake. Can feel more like a "cog in a machine."
- Hospital-Employed: Many hospitals now directly employ their physicians.
- Pros: Stable and predictable salary, strong integration with the hospital system, often excellent benefits and retirement plans (sometimes including pensions).
- Cons: Salary ceiling may be lower than in private groups, less flexibility, subject to hospital administration's policies.
- Academic Medical Centers: Working for a university hospital.
- Pros: Opportunities for teaching medical students and residents, research, and sub-specialization. Often a more "cerebral" practice style with complex cases. Excellent benefits.
- Cons: Consistently the lowest-paying practice model. Pressure to publish and participate in academic activities ("publish or perish").
- Locum Tenens ("Traveling Doctor"): Working as an independent contractor on temporary assignments.
- Pros: Extremely high hourly rates (often $250-$400+ per hour), complete control over your schedule, ability to travel and experience different practice settings.
- Cons: No benefits (health insurance, retirement), you must pay your own malpractice insurance and self-employment taxes, constant travel can be isolating, lack of job stability.
###
In-Demand Skills and Other Factors
Beyond the major categories, several other skills and factors can add value and increase earning potential.
- Procedural Proficiency (especially Ultrasound): Mastery of point-of-care ultrasound (POCUS) is no longer a bonus; it's becoming a standard of care. Physicians with advanced ultrasound skills or certifications are highly sought after.
- Administrative and Business Acumen: Understanding hospital finances, billing and coding, and departmental metrics can pave the way for leadership roles. Taking an active interest in the business side of medicine is a clear path to higher income.
- Bilingualism: In many parts of the country, fluency in a second language (especially Spanish) is a major asset that can improve patient care and make a candidate more attractive to employers.
- Shift Type: Night shifts and holiday shifts almost always come with a "shift differential"—an extra amount per hour (e.g., an additional $10-$30/hour) to compensate for the unsociable hours.
By strategically considering these factors, a physician can do more than just find a job—they can build a career that aligns with their financial goals, lifestyle preferences, and professional aspirations.
Job Outlook and Career Growth

For anyone investing over a decade in education and training, the long-term stability and growth prospects of their chosen field are paramount. The job outlook for Emergency Medicine is a topic of significant discussion within the medical community, with a blend of strong fundamentals and emerging challenges.
Official Projections: A Growing Need for Physicians
The U.S. Bureau of Labor Statistics (BLS) projects strong overall growth for physicians and surgeons. According to its Occupational Outlook Handbook, employment for physicians and surgeons is projected to grow 3 percent from 2022 to 2032, which is about as fast as the average for all occupations.
The BLS attributes this growth to several key factors:
- An Aging Population: As the large baby-boom generation ages, they will require more medical care, including acute and emergency services for conditions like heart attacks, strokes, and falls.
- Rising Chronic Disease: Increased rates of chronic conditions like diabetes and heart disease often lead to acute complications that necessitate emergency care.
- Expanded Healthcare Access: While debated, expanded access to health insurance can lead more people to seek care in emergency departments.
This macro-level data suggests a stable, long-term demand for physicians, including those in emergency medicine.
The Current Debate: A Physician Surplus?
Despite the positive BLS outlook, there has been significant concern within the Emergency Medicine community itself about a potential oversupply of physicians. This concern, highlighted in reports from organizations like the American College of Emergency Physicians (ACEP), stems from:
- Rapid Growth in Residency Programs: The number of EM residency positions has grown substantially over the past decade.
- Increased Use of Advanced Practice Providers (APPs): Hospitals are increasingly utilizing Physician Assistants (PAs) and Nurse Practitioners (