In the intricate and vital world of healthcare, few roles combine deep scientific knowledge, advanced clinical skill, and profound human compassion as effectively as the Neurology Nurse Practitioner. If you are drawn to the complexities of the human brain and nervous system and aspire to a career at the forefront of patient care, this path offers not only immense personal fulfillment but also significant financial reward. The national average neurology nurse practitioner salary comfortably exceeds six figures, reflecting the critical expertise and responsibility inherent in the role.
As a career analyst who has guided countless healthcare professionals, I've seen firsthand the unique dedication of those in neurology. I once coached a newly certified NP who, just months into her job at a comprehensive stroke center, helped coordinate the care for a patient who had suffered a massive, debilitating stroke. Her calm, expert management—from interpreting initial scans to educating the terrified family about the long road ahead—was a masterclass in what makes this role so invaluable. She wasn't just a clinician; she was a pillar of strength and a source of clarity in a moment of chaos. This is the true value that a high neurology nurse practitioner salary represents: irreplaceable expertise when it matters most.
This comprehensive guide will serve as your roadmap to understanding and achieving a top-tier neurology nurse practitioner salary. We will explore every facet of the career, from daily responsibilities and salary benchmarks to the specific factors you can leverage to maximize your earning potential.
### Table of Contents
- [What Does a Neurology Nurse Practitioner Do?](#what-they-do)
- [Average Neurology Nurse Practitioner Salary: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence Salary](#key-factors)
- [Job Outlook and Career Growth](#job-outlook)
- [How to Get Started in This Career](#how-to-start)
- [Conclusion: Is a Career as a Neurology NP Right for You?](#conclusion)
What Does a Neurology Nurse Practitioner Do?
A Neurology Nurse Practitioner (NP), sometimes called a Neuroscience NP, is an Advanced Practice Registered Nurse (APRN) who has specialized in the diagnosis, treatment, and management of conditions affecting the central and peripheral nervous systems. They are highly autonomous practitioners who blend the diagnostic acumen of a physician with the holistic, patient-centered approach of nursing. They are the essential link in the neurology care team, often serving as the primary point of contact for patients with chronic and acute neurological disorders.
These dedicated professionals work in a variety of settings, including hospital inpatient units (such as stroke units or neuro-intensive care), outpatient specialty clinics, private neurology practices, and academic medical centers. Their patient population is incredibly diverse, ranging from individuals experiencing their first seizure to those managing long-term conditions like multiple sclerosis (MS), Parkinson's disease, epilepsy, or dementia.
Core responsibilities of a Neurology Nurse Practitioner include:
- Comprehensive Patient Assessment: Performing detailed neurological exams, taking extensive patient histories, and evaluating cognitive and motor function.
- Diagnosis of Neurological Conditions: Ordering and interpreting diagnostic tests such as MRI and CT scans, electroencephalograms (EEGs), electromyography (EMG), and lumbar punctures.
- Developing Treatment Plans: Creating and implementing evidence-based treatment strategies, which includes prescribing medications (e.g., anti-epileptics, immunomodulators for MS, medications for Parkinson's disease), and recommending therapies (physical, occupational, speech).
- Managing Chronic Disease: Providing long-term follow-up care for patients with conditions like epilepsy, MS, or migraine, adjusting medications and treatment plans as the disease progresses or as new therapies become available.
- Performing Procedures: Depending on the setting and training, some Neuro NPs perform procedures such as lumbar punctures, trigger point injections, or Botox injections for chronic migraine and spasticity. They may also be involved in managing devices like vagus nerve stimulators (VNS) or deep brain stimulators (DBS).
- Patient and Family Education: A cornerstone of the role is educating patients and their families about their diagnosis, treatment options, medication side effects, and strategies for managing symptoms and improving quality of life.
- Collaboration: Working closely with neurologists, neurosurgeons, radiologists, pharmacists, and rehabilitation therapists to provide coordinated, multidisciplinary care.
### A Day in the Life: Outpatient Neurology Clinic
To make this role more tangible, let's walk through a typical day for a Neurology NP working in an outpatient clinic specializing in movement disorders.
- 8:00 AM: Arrives at the clinic. Reviews the day’s schedule of 12 patients, flagging complex cases. Quickly checks patient charts, recent lab results, and imaging reports that came in overnight.
- 8:30 AM: First patient arrives. A 68-year-old male with Parkinson’s disease for a 6-month follow-up. The NP conducts a full assessment, including the Unified Parkinson's Disease Rating Scale (UPDRS), and discusses the patient's increasing "off" periods. They decide to adjust his carbidopa/levodopa timing and add a new medication, spending significant time educating the patient and his wife about the new drug's potential side effects.
- 10:00 AM: Sees a new patient, a 55-year-old woman referred for a persistent tremor. The NP takes a detailed history, performs a meticulous neurological exam to differentiate between an essential tremor and early Parkinson's, and orders a DaTscan to aid in diagnosis.
- 11:30 AM: A patient with a Deep Brain Stimulator (DBS) comes in for programming adjustments. The NP uses a specialized device to communicate with the implanted neurostimulator, carefully adjusting the electrical parameters to optimize symptom control (e.g., reduce tremor) while minimizing side effects like speech difficulty.
- 12:30 PM: Lunch break, which often involves catching up on charting, returning urgent patient calls, and responding to messages in the electronic health record (EHR) from patients asking about medication refills or new symptoms.
- 1:30 PM: The afternoon begins with follow-up appointments for patients with Huntington's disease and dystonia, requiring both medication management and deep empathy for the psychosocial challenges these conditions present.
- 3:00 PM: The NP dedicates a 45-minute slot to a telehealth visit with a long-standing patient who lives two hours away, ensuring continuity of care without the burden of travel for the patient.
- 4:00 PM: The final patient is a follow-up for a patient who recently started Botox injections for cervical dystonia. The NP assesses the efficacy of the treatment and plans the next injection cycle.
- 4:30 PM - 5:30 PM (or later): "Desktop medicine." This is dedicated time for completing all patient charts from the day, signing off on prescription refills, reviewing incoming test results, and making referral calls to physical therapists or social workers. The NP also drafts a letter to the referring physician of the new patient seen this morning, outlining the initial findings and plan.
This "day in the life" illustrates the incredible blend of technical skill, critical thinking, and compassionate communication that defines the neurology NP role.
Average Neurology Nurse Practitioner Salary: A Deep Dive

The financial compensation for a neurology nurse practitioner is a direct reflection of their advanced education, specialized skillset, and the high level of responsibility they undertake. While salaries can vary significantly based on several factors we will explore later, the overall earning potential is robust and highly competitive within the healthcare industry.
According to a comprehensive analysis of recent data from leading salary aggregators, the national average neurology nurse practitioner salary in the United States falls within a strong range.
- Salary.com reports the average salary for a Nurse Practitioner - Neurology to be $125,189 per year as of late 2023, with a typical range falling between $116,211 and $132,963.
- Payscale.com indicates an average base salary of approximately $118,500 per year for professionals with neuroscience skills.
- ZipRecruiter shows a higher national average, citing $134,179 per year for a Neurology Nurse Practitioner.
Synthesizing this data, it's reasonable to establish a national average base salary for a Neurology NP in the $120,000 to $135,000 range. However, this is just the base salary. The total compensation package often pushes the overall value much higher.
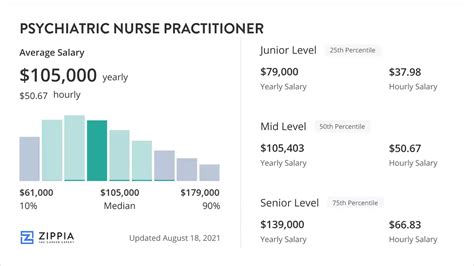
### Neurology NP Salary by Experience Level
Like any profession, experience is a primary driver of salary growth. As a Neurology NP gains clinical autonomy, hones their diagnostic skills, and develops expertise in specific sub-specialties, their value to an organization—and their corresponding paycheck—increases significantly.
Here is a breakdown of typical salary expectations based on years of experience. These figures are estimates synthesized from industry data and represent base salary before bonuses or other compensation.
| Career Stage | Years of Experience | Estimated Annual Salary Range | Description of Role & Responsibilities |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $105,000 - $122,000 | Recently graduated and certified NPs, often working under closer supervision of a neurologist. May start in a general neurology setting or a structured fellowship program to build foundational skills. Focus is on learning practice-specific protocols and gaining confidence in patient management. |
| Mid-Career | 3-9 Years | $120,000 - $140,000 | An autonomous and proficient practitioner who manages a full patient panel. Often develops a niche in a sub-specialty (e.g., MS, epilepsy). May begin to take on additional responsibilities like precepting new NPs or students and participating in quality improvement projects. |
| Senior / Experienced | 10+ Years | $135,000 - $160,000+ | A recognized expert within their practice or hospital system. Manages the most complex cases and may lead a sub-specialty clinic. Often holds leadership roles, serves on hospital committees, engages in research, and may have a DNP degree. Salaries at the highest end often belong to those in high-cost-of-living areas, high-acuity settings (like neuro-ICU), or private practices with productivity bonuses. |
*Source: Analysis of data from Salary.com, Payscale, and ZipRecruiter, updated for 2023-2024.*
### Beyond the Base Salary: Understanding Total Compensation
A savvy career professional knows that base salary is only one part of the financial picture. A comprehensive compensation package for a neurology nurse practitioner can add tens of thousands of dollars in value each year. When evaluating a job offer, it's crucial to consider these other components:
- Bonuses:
- Sign-On Bonus: Increasingly common, especially in competitive markets or for hard-to-fill positions. These can range from $5,000 to $25,000 or more.
- Performance/Productivity Bonus: Common in private practice and some hospital systems. This is often based on metrics like patient volume (Relative Value Units, or RVUs), patient satisfaction scores, or achieving specific quality outcomes.
- Retention Bonus: Offered to valued, long-term employees to encourage them to stay with the organization.
- Retirement & Benefits:
- 401(k) or 403(b) Matching: A strong employer match is essentially free money. A common match is 50% of the first 6% you contribute, effectively adding 3% of your salary to your retirement savings.
- Health Insurance: Premium health, dental, and vision insurance plans with low deductibles and out-of-pocket maximums represent significant financial value.
- Paid Time Off (PTO): Generous PTO, sick leave, and paid holidays are standard. Many healthcare systems offer 4-6 weeks of combined time off per year.
- Professional Development Allowances:
- Continuing Medical Education (CME): Most employers provide an annual stipend (typically $1,500 - $3,000) and paid time off to attend conferences, workshops, and other educational activities required to maintain licensure and certification.
- Tuition Reimbursement: Many hospital systems offer tuition assistance for employees pursuing further education, such as a Doctor of Nursing Practice (DNP) degree.
- Licensure and Certification Fees: Employers typically cover the costs of state licensure renewal, DEA license fees, and specialty certification (like CNRN or SCRN) fees.
When you sum the value of these benefits, a job offer with a $130,000 base salary can easily have a total compensation value exceeding $160,000 per year.
Key Factors That Influence Neurology Nurse Practitioner Salary

While we've established a solid baseline, the actual salary you can command is influenced by a powerful combination of personal qualifications, geographic location, and workplace dynamics. Understanding these levers is the key to maximizing your earning potential throughout your career. This section provides a granular analysis of the most impactful factors.
### 1. Level of Education and Certification
Your educational foundation and specialized credentials are the bedrock of your clinical authority and, consequently, your salary.
- MSN vs. DNP: The two primary educational pathways to becoming an NP are the Master of Science in Nursing (MSN) and the Doctor of Nursing Practice (DNP).
- MSN: The traditional degree for NP preparation, focusing on advanced clinical practice.
- DNP: A terminal practice doctorate that builds on the MSN with additional coursework in leadership, evidence-based practice, quality improvement, and systems-level thinking.
Currently, the direct salary difference for a new graduate with an MSN versus a DNP in a purely clinical role may be minimal to non-existent. However, the DNP is rapidly becoming the preferred degree and can provide a significant long-term salary advantage. DNP-prepared NPs are better positioned for leadership roles (e.g., Director of Advanced Practice Providers), academic positions, and high-level research or policy roles, all of which come with higher compensation. Think of the DNP as an investment in your future career ceiling.
- Specialty Certifications: This is where you can create a significant competitive and financial edge. Standard NP board certification (e.g., FNP-C, AGACNP-BC) is required for licensure. However, neurology-specific certifications demonstrate a validated, high level of expertise.
- Certified Neuroscience Registered Nurse (CNRN®): Offered by the American Board of Neuroscience Nursing (ABNN), this certification is for nurses who have specialized experience in neuroscience. While it's an RN-level certification, many NPs maintain it to demonstrate foundational expertise. Holding it can make you a more attractive candidate.
- Stroke Certified Registered Nurse (SCRN®): Also offered by the ABNN, this is a highly respected certification for nurses and NPs working extensively with stroke patients in settings like stroke centers and neuro-ICUs. In a competitive job market for a stroke NP position, holding an SCRN can be a deciding factor and a point of salary negotiation.
- Other Relevant Certifications: Certifications in areas like Multiple Sclerosis (MS-C) or palliative care (ACHPN®) can also increase your value if your practice focuses on these patient populations.
Holding advanced certifications signals to an employer that you are a dedicated expert committed to the highest standards of care, which is a powerful argument for a higher salary.
### 2. Years of Clinical Experience
As detailed in the salary table above, experience is arguably the single most powerful driver of salary growth in a clinical role. However, it's not just the *quantity* of years but the *quality* of that experience that matters.
- Entry-Level (0-2 Years): The primary focus is on consolidating skills. Salary is typically at the lower end of the spectrum. The most valuable experience to gain here is in a high-volume setting with strong mentorship, even if the pay is slightly lower than other initial offers. A post-graduate NP Neurology Fellowship can be invaluable here, providing structured, intensive training that can accelerate your career and earning trajectory.
- Mid-Career (3-9 Years): You have moved from novice to expert. You have likely developed a reputation for managing a specific patient population exceptionally well. This is the prime time for salary negotiation during performance reviews or when changing jobs. Your proven track record of managing a full patient load efficiently and with excellent outcomes is your main bargaining chip.
- Senior Level (10+ Years): At this stage, salary growth is often tied to expanding your role beyond direct patient care. Your experience is leveraged for mentorship, leadership, program development (e.g., starting a new headache clinic), or leading research initiatives. These activities add immense value to an organization and are compensated accordingly. Senior NPs who have cultivated deep expertise in a lucrative subspecialty (like interventional headache medicine) can command salaries well into the upper $100s.
### 3. Geographic Location
Where you choose to practice has a dramatic impact on your salary, though it must always be balanced against the local cost of living. NP practice authority also varies by state (Full, Reduced, or Restricted Practice), which can influence roles and compensation.
Top-Paying States for Nurse Practitioners:
Generally, states with a high cost of living and high demand for healthcare providers offer the highest salaries. According to the U.S. Bureau of Labor Statistics (BLS) Occupational Employment and Wage Statistics for Nurse Practitioners (May 2022), the top-paying states are:
1. California: Annual Mean Wage: $158,130
2. New Jersey: Annual Mean Wage: $143,250
3. Massachusetts: Annual Mean Wage: $138,700
4. Oregon: Annual Mean Wage: $136,250
5. Nevada: Annual Mean Wage: $136,230
*Note: These are figures for all NP specialties, but neurology NP salaries follow similar geographic trends.*
Salary Variation by Metro Area vs. Rural Area:
Salaries are typically highest in major metropolitan areas. A Neurology NP in San Francisco, New York City, or Boston can expect to earn significantly more than one in a smaller city or rural area. However, the cost of living in these metros can consume a large portion of that extra income.
Conversely, some rural or underserved areas, desperate to attract qualified providers, may offer competitive salaries, significant sign-on bonuses, and even student loan repayment assistance through programs like the National Health Service Corps (NHSC). A $125,000 salary in a low-cost-of-living area in the Midwest could provide a higher quality of life than a $150,000 salary in a major coastal city.
Example Salary Comparison (Illustrative):
- Neurology NP in Los Angeles, CA: ~$145,000 - $165,000+
- Neurology NP in Chicago, IL: ~$125,000 - $145,000
- Neurology NP in Kansas City, MO: ~$115,000 - $130,000
- Neurology NP in a rural Southern town: ~$105,000 - $120,000 (but may include loan repayment)
### 4. Work Setting / Type of Employer
The environment where you work dictates your daily tasks, patient acuity, and compensation structure.
- Large Academic Medical Centers: These institutions are often on the cutting edge of research and technology.
- Pros: Access to novel treatments, opportunities for research and teaching, often excellent benefits and retirement packages, prestige.
- Cons: Salaries can be more rigid and determined by structured pay scales. Bureaucracy can be significant.
- Salary: Tends to be competitive and stable, often in the mid-to-high end of the national average.
- Private Neurology Practice: These can range from small, single-physician practices to large, multi-specialty neurology groups.
- Pros: More autonomy, potentially a faster-paced environment, often includes a productivity bonus structure which can significantly increase total income.
- Cons: Benefits might be less robust than a large hospital system. More direct pressure related to billing and practice revenue.
- Salary: Can have the highest earning potential, especially for experienced NPs who can generate significant revenue. Base salary might be average, but a strong productivity bonus can push total compensation to the top of the range.
- Inpatient Hospital Setting (Neuro-ICU, Stroke Unit, EMU): This is a high-acuity, high-stress environment.
- Pros: You will manage the most critical and complex cases. Work is often shift-based (e.g., three 12-hour shifts), which can be appealing.
- Cons: High emotional toll, risk of burnout. Requires exceptional critical thinking and procedural skills.
- Salary: Often among the highest due to the intensity and acuity of the work. Shift differentials for nights, weekends, and holidays can add another 10-20% to the base salary. An inpatient Neuro-ICU NP can be one of the highest-paid specialists.
- Outpatient Community Clinics: These settings focus on chronic disease management and continuity of care.
- Pros: More predictable hours (typically M-F, 9-5), opportunity to build long-term relationships with patients.
- Cons: Patient volume can be very high. May not see the same level of acuity as in a hospital.
- Salary: Tends to be in the solid middle of the national average range.
### 5. Area of Sub-Specialization within Neurology
Just as neurologists sub-specialize, so do Neurology NPs. Developing deep expertise in a specific area can make you an invaluable asset and boost your salary.
- Stroke and Neuro-critical Care: As mentioned, this high-acuity field commands top-tier salaries due to the life-or-death nature of the work.
- Epilepsy: Managing complex seizure disorders, interpreting EEGs, and managing VNS devices requires specialized knowledge that is in high demand.
- Movement Disorders: Expertise in managing Parkinson's disease, dystonia, and especially programming Deep Brain Stimulators (DBS) is a highly marketable and well-compensated skill.
- Multiple Sclerosis (MS) / Neuroimmunology: The treatment landscape for MS is complex and rapidly evolving with expensive biologic therapies. An NP who is an expert in this area is a huge asset to a practice.
- Headache Medicine: This is a surprisingly lucrative and growing subspecialty. NPs who can perform procedures like Botox injections for chronic migraine and various nerve blocks can be significant revenue generators for a practice, leading to higher compensation.
### 6. In-Demand Skills
Beyond your core clinical knowledge, certain tangible skills can directly translate into a higher salary.
- Procedural Competence: The ability to perform and bill for procedures is a major value-add. This includes:
- Lumbar Punctures (LPs)
- Botox injections (for