Introduction

Have you ever wondered what it takes to work on the front lines of one of medicine's most complex and fascinating frontiers? The human brain and nervous system represent a universe of discovery, and a career as a Neurology Physician Assistant (PA) places you directly at the heart of it. This isn't just a job; it's a calling for the intellectually curious, the deeply empathetic, and the clinically skilled. It’s a role where you directly impact the lives of patients grappling with conditions like epilepsy, Parkinson's disease, stroke, and multiple sclerosis, offering them not just treatment, but hope and quality of life.
For those considering this challenging yet immensely rewarding path, a crucial question naturally arises: "What is a neurology physician assistant salary?" The answer is compelling. Nationally, PAs in neurology are highly compensated professionals, with average salaries often ranging from $115,000 to over $150,000 annually, depending on a confluence of factors we will explore in detail. This financial stability, combined with exceptional job growth projections, makes it one of the most attractive specializations in modern healthcare.
I once had the privilege of shadowing a neurology team where I observed a PA manage a patient's newly diagnosed multiple sclerosis. The PA's ability to translate complex neurological concepts into understandable, reassuring language for the terrified patient and their family was a masterclass in compassionate care. It was a profound reminder that this role is as much about human connection as it is about clinical acumen.
This comprehensive guide is designed to be your definitive resource, whether you are a student mapping out your future, a current PA considering a specialty change, or a seasoned professional seeking to maximize your earning potential. We will dissect every component of a Neurology PA's career, from daily responsibilities to the nuanced factors that shape your salary and long-term growth.
### Table of Contents
- [What Does a Neurology Physician Assistant Do?](#what-does-a-neurology-physician-assistant-do)
- [Average Neurology Physician Assistant Salary: A Deep Dive](#average-neurology-physician-assistant-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Neurology Physician Assistant Do?

A Neurology Physician Assistant is a highly skilled, nationally certified, and state-licensed medical professional who practices medicine on a healthcare team with a supervising neurologist. They are not merely "assistants" but are critical extenders of the neurologist, exercising considerable autonomy in diagnosing and treating patients with a wide spectrum of neurological disorders. Their work is a dynamic blend of intellectual challenge, procedural skill, and long-term patient relationship management.
The scope of practice for a Neurology PA is vast and can vary significantly based on the practice setting (inpatient vs. outpatient), the sub-specialty, and state laws. However, their core responsibilities consistently revolve around delivering high-quality patient care.
Core Responsibilities and Daily Tasks:
- Comprehensive Patient Evaluation: Conducting detailed patient histories and performing sophisticated neurological physical examinations. This includes assessing cranial nerves, motor and sensory function, reflexes, gait, balance, and mental status.
- Diagnosis and Treatment Planning: Formulating differential diagnoses for complex symptoms like headaches, dizziness, weakness, or memory loss. They order and interpret a variety of diagnostic tests, including MRIs and CT scans of the brain and spine, electroencephalograms (EEGs), electromyography (EMG), and lumbar punctures.
- Medication Management: Prescribing and managing complex medication regimens for chronic neurological conditions such as epilepsy (anticonvulsants), Parkinson's disease (dopaminergic agents), and multiple sclerosis (disease-modifying therapies). This requires a deep understanding of pharmacology and potential side effects.
- Performing Procedures: Depending on the setting and training, Neurology PAs may perform procedures such as:
- Lumbar Punctures (Spinal Taps): To analyze cerebrospinal fluid for signs of infection, inflammation, or other abnormalities.
- Botox Injections: For treating chronic migraines, dystonia, or spasticity.
- Trigger Point Injections: For certain types of headache and neck pain.
- Nerve Blocks: To manage specific pain syndromes.
- Patient and Family Education: A cornerstone of the role. PAs spend significant time explaining diagnoses, treatment options, and lifestyle modifications to patients and their families. They empower patients to become active participants in their own care.
- Interdisciplinary Collaboration: Working closely with a team of neurologists, neurosurgeons, physical therapists, occupational therapists, speech therapists, social workers, and primary care providers to ensure holistic patient care.
- Documentation: Meticulously documenting all patient encounters, test results, and treatment plans in the Electronic Health Record (EHR).
---
### A Day in the Life: Outpatient Neurology Clinic PA
To make this tangible, let's walk through a typical day for a PA in a busy outpatient neurology practice.
- 8:00 AM - Morning Huddle: The day begins with a brief meeting with the supervising neurologist and other clinic staff. They review the day's schedule, discuss complex cases from the previous day, and flag any urgent patient messages or lab results.
- 8:30 AM - First Patient: New Onset Seizure: A 25-year-old patient referred by their PCP for a first-time seizure. The PA takes an exhaustive history from the patient and a family member who witnessed the event. They perform a full neurological exam, looking for any focal deficits. The PA then counsels the patient on seizure precautions (e.g., driving restrictions), orders an EEG and a brain MRI to investigate the cause, and schedules a follow-up appointment to discuss the results.
- 9:30 AM - Follow-Up: Chronic Migraine Management: A 45-year-old patient returns for a 3-month follow-up. The PA reviews the patient's headache diary, assesses the effectiveness of their current preventative medication, and discusses potential side effects. Since the patient is still having frequent, debilitating migraines, the PA proposes and performs a series of Botox injections for chronic migraine prophylaxis, a procedure they are trained and credentialed to do.
- 10:45 AM - Follow-Up: Parkinson's Disease: An established 70-year-old patient with Parkinson's disease. The PA assesses for disease progression, focusing on motor symptoms (tremor, rigidity, bradykinesia) and non-motor symptoms (mood changes, constipation). They adjust the patient's carbidopa/levodopa dosage to optimize symptom control while minimizing "off" time. They also provide a referral to physical therapy to work on gait and balance.
- 12:00 PM - Administrative Time & Lunch: The PA catches up on charting, answers patient portal messages, reviews incoming lab and imaging reports, and handles prescription refill requests. They might use this time to call a patient to discuss an abnormal MRI finding and reassure them about the next steps.
- 1:00 PM - Urgent Add-On: Bell's Palsy: A patient calls with sudden facial drooping. The clinic adds them to the schedule. The PA performs a targeted exam to differentiate Bell's palsy from a more serious condition like a stroke. After confirming the diagnosis, they prescribe a course of steroids and antivirals and provide extensive education on eye care to prevent corneal abrasion.
- 2:00 PM - New Patient: Memory Concerns: A 65-year-old patient brought in by their daughter due to concerns about progressive memory loss. The PA conducts a thorough history and performs cognitive screening tests like the Montreal Cognitive Assessment (MoCA). They discuss the wide range of potential causes, from vitamin deficiencies to early-stage dementia, and order initial bloodwork and imaging to begin the diagnostic workup.
- 3:30 PM - Infusion Center Check-in: The clinic has an associated infusion suite where MS patients receive their biologic medications. The PA quickly checks in on a patient receiving a Tysabri infusion, assessing for any adverse reactions and answering their questions.
- 4:00 PM - Finalizing the Day: The last patient is seen. The remainder of the afternoon is dedicated to finishing all clinical documentation, signing off on charts, and creating a plan for the next day. The PA discusses the day's complex cases with the supervising neurologist, ensuring alignment on treatment plans and follow-up.
- 5:30 PM - End of Day: The PA leaves the clinic, having managed a diverse and challenging caseload that directly improved the lives of their patients.
Average Neurology Physician Assistant Salary: A Deep Dive
The financial compensation for a Neurology Physician Assistant is a significant draw, reflecting the high level of skill, responsibility, and demand for this specialty. While salaries can vary widely, the field offers a robust income and a strong return on educational investment.
It's crucial to understand that "salary" is just one part of the total compensation package. We will dissect base salary figures and then explore the additional financial components that contribute to overall earnings.
National Average Salary and Typical Range
The most authoritative source for PA salary data is the American Academy of Physician Associates (AAPA). Their annual salary report provides detailed breakdowns by specialty, experience, and location.
- According to the 2023 AAPA Salary Report, the median total compensation for PAs in Neurology was $128,000 per year. This report, based on data from over 13,000 PAs, is a trusted benchmark for the profession.
- Other reputable salary aggregators provide corroborating data, often reflecting slightly different averages based on their unique data sets:
- Salary.com reports the average Neurology Physician Assistant salary in the United States is around $135,101 as of late 2023, with a typical range falling between $124,420 and $147,783.
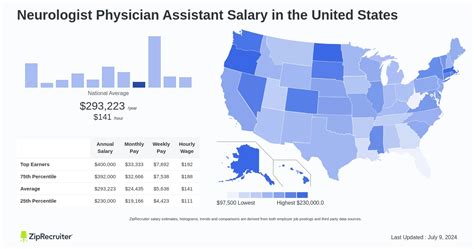
- ZipRecruiter shows a national average of approximately $141,500 per year, with top earners reaching $175,000 or more.
- Payscale notes an average base salary closer to $115,000, highlighting the importance of looking at total compensation rather than just the base figure.
The general consensus is that a starting Neurology PA can expect a salary well over $100,000, with significant growth potential. It is not uncommon for experienced PAs in high-demand areas or specific sub-specialties to earn upwards of $160,000 to $180,000 annually.
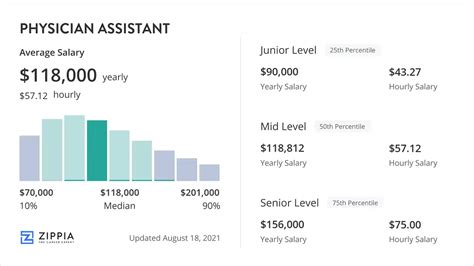
Salary by Experience Level
Experience is one of the most powerful drivers of salary growth. As a Neurology PA gains clinical expertise, autonomy, and procedural proficiency, their value to a practice increases exponentially.
| Experience Level | Years of Experience | Typical Annual Base Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $105,000 - $120,000 | Focus on foundational skills, working with close supervision. Learning clinic flow and managing common neurological conditions. |
| Mid-Career | 3-9 Years | $120,000 - $145,000 | Increased autonomy. Managing a more complex patient panel. Often involved in precepting students or new hires. May begin sub-specializing. |
| Senior/Experienced| 10+ Years | $145,000 - $170,000+ | Clinical expert. Often holds leadership roles (Lead PA). May have advanced certifications (CAQ). High level of procedural skill and efficiency. |
*Source: Data compiled and synthesized from AAPA, Salary.com, and industry observations.*
It's important to note that the leap from entry-level to mid-career often brings the most significant percentage increase in salary, as the PA proves their competence and becomes a fully productive member of the team.
Dissecting the Compensation Package: Beyond the Base Salary
An offer letter contains much more than just a base salary. Understanding the full compensation package is vital for accurately assessing your financial picture.
- Base Salary: This is the guaranteed, fixed amount you earn, paid bi-weekly or monthly. It forms the foundation of your compensation.
- Bonuses: Many neurology practices, especially private ones, offer bonuses tied to productivity or practice performance.
- Productivity Bonus: This is often based on Relative Value Units (RVUs), a measure of physician work. PAs who see more patients or perform more procedures generate more RVUs and can earn a percentage of the revenue they bring in above a certain threshold.
- Performance Bonus: This might be tied to quality metrics, patient satisfaction scores, or achieving specific practice goals.
- Year-End/Profit-Sharing Bonus: In profitable private practices, a portion of the year's profits may be distributed among providers. The AAPA reports that the median bonus amount for PAs who received one was approximately $7,000.
- CME Allowance: Employers almost universally provide an allowance for Continuing Medical Education (CME). This is typically $1,500 to $3,500 per year and is intended to cover the cost of conferences, online courses, and other educational activities required to maintain certification and licensure. Many also provide paid time off specifically for attending these events.
- Retirement Plans: This is a critical component of long-term wealth building.
- 401(k) or 403(b): Employers often offer a matching contribution, such as matching 50% of your contributions up to 6% of your salary. This is essentially free money and a powerful savings tool.
- Other Benefits: The value of these benefits can add tens of thousands of dollars to your total compensation.
- Health, Dental, and Vision Insurance: Employer-subsidized plans are standard.
- Professional Liability (Malpractice) Insurance: This is always covered by the employer. It's crucial to understand the type of policy (claims-made vs. occurrence).
- Licensure and Certification Fees: Most employers will reimburse the costs of state licensure, DEA registration, and NCCPA recertification fees.
- Paid Time Off (PTO): This typically includes vacation, sick leave, and holidays, and can range from 3 to 6 weeks per year depending on the institution and years of service.
- Student Loan Repayment Assistance: This is becoming an increasingly common and valuable perk, particularly in non-profit or government settings (e.g., the PSLF program) or in underserved areas.
When evaluating a job offer, it's essential to calculate the total value. A job with a $125,000 base salary and a generous bonus structure, 401(k) match, and student loan assistance could be far more lucrative than a job with a flat $135,000 salary and minimal benefits.
Key Factors That Influence Salary

While the national averages provide a useful benchmark, a Neurology PA's actual salary is a complex equation influenced by a multitude of intersecting factors. Understanding these variables is the key to negotiating effectively and maximizing your earning potential throughout your career. This section provides an exhaustive breakdown of the elements that will most significantly impact your paycheck.
###
Level of Education and Advanced Certification
While the standard entry-level degree for all PAs is a Master's degree from an ARC-PA accredited program, the pursuit of advanced credentials within neurology can have a direct and substantial impact on salary and career opportunities.
The Certificate of Added Qualifications (CAQ) in Neurology
The single most important post-graduate credential for a Neurology PA is the CAQ in Neurology, offered by the National Commission on Certification of Physician Assistants (NCCPA). This is not a requirement to practice in neurology, but it is the gold standard for demonstrating expertise and commitment to the specialty.
- What it Signifies: The CAQ is a voluntary credential that certifies a PA has met rigorous standards of experience, continuing education, and specialized knowledge in neurology. It signals to employers, colleagues, and patients that you are a top-tier clinician in the field.
- Requirements: To earn the CAQ, a PA must:
1. Hold a current PA-C certification.
2. Possess a valid, unrestricted license to practice.
3. Complete at least two years of full-time experience working as a PA in neurology (minimum of 4,000 hours).
4. Submit an attestation from a supervising neurologist confirming their skills and experience.
5. Complete at least 150 credits of Category 1 CME focused on neurology within the last six years.
6. Pass the Neurology Specialty Exam, a comprehensive 120-question exam covering the breadth of neurological practice.
- Salary Impact: While exact figures are hard to isolate, PAs holding a CAQ are more competitive candidates for higher-paying jobs, particularly in academic centers and leadership roles. Employers view the CAQ as a de-risking factor; it proves a candidate's competency. This leverage can easily translate into a 5% to 15% higher salary offer compared to a non-certified peer with similar experience. It also opens doors to roles with higher base salaries, such as a "Senior Neurology PA" or a "Neurology Sub-specialty Coordinator."
###
Years of Experience: The Autonomy-to-Income Trajectory
Experience is perhaps the most linear and predictable driver of salary growth. In a complex specialty like neurology, the learning curve is steep, and clinical judgment is honed over years of practice, not just in the classroom.
- 0-2 Years (The Apprentice Phase): In the first two years, a PA is solidifying their knowledge base. They learn to efficiently perform a neurological exam, manage common conditions like migraines and essential tremor, and navigate the healthcare system. Salary is reflective of this training period, typically in the $105,000 - $120,000 range. The focus is on learning, not earning.
- 3-9 Years (The Journeyman Phase): This is the period of greatest growth. By year three, a Neurology PA is often managing their own panel of patients with significant autonomy. They are comfortable with more complex diagnoses, such as distinguishing between different types of dementia or managing refractory epilepsy. Their efficiency increases, allowing them to see more patients and generate more revenue for the practice. This is where salaries climb steeply into the $120,000 - $145,000 range, and productivity bonuses become a significant part of compensation.
- 10+ Years (The Master Phase): After a decade, a PA is a seasoned expert. They are often the go-to person in the clinic for difficult cases. They may have a highly specialized patient panel (e.g., exclusively movement disorders or MS). They are often involved in leadership, administration, research, or education. Their clinical efficiency and expertise command top-tier salaries, often exceeding $150,000, with highly experienced PAs in lucrative settings pushing towards $180,000 or more with bonuses.
###
Geographic Location: The Cost of Living and Demand Equation
Where you choose to practice has one of the most significant impacts on your salary. This variation is driven by a combination of local market demand, state-level scope of practice laws, the density of healthcare systems, and, most importantly, the cost of living.
Top-Paying States for Physician Assistants:
States with high costs of living and/or high demand for healthcare providers consistently offer the highest salaries. According to the U.S. Bureau of Labor Statistics (BLS) and other sources, the top-paying states for PAs in general (which strongly correlates for neurology) include:
1. California: Average salaries can be 15-25% higher than the national average. A Neurology PA in Los Angeles or the Bay Area could command $150,000 - $180,000+.
2. New York: Particularly in the New York City metro area, high demand and cost of living drive salaries up, often in the $145,000 - $175,000 range.
3. Washington: A strong healthcare market in Seattle and favorable PA practice laws contribute to high salaries.
4. Alaska: To attract providers to a remote location, salaries are often inflated.
5. Connecticut & New Jersey: Proximity to major metro areas like NYC and Boston keeps salaries competitive.
Lower-Paying States:
Conversely, states in the Southeast and parts of the Midwest with a lower cost of living tend to have lower average salaries. States like Alabama, Arkansas, and Mississippi may offer salaries closer to the $100,000 - $115,000 range. However, it is critical to weigh salary against the cost of living. A $115,000 salary in a city with low housing costs and taxes may provide a higher quality of life than a $140,000 salary in a city like San Diego or Boston.
Urban vs. Rural Divide:
The dynamic between urban and rural settings is complex.
- Urban/Suburban: Major metropolitan areas typically have higher base salaries due to the cost of living and the presence of large, competitive academic medical centers and private practice groups.
- Rural: While base salaries may be slightly lower, rural or underserved areas often offer significant financial incentives to attract providers. These can include large sign-on bonuses ($10,000 - $25,000+), student loan repayment programs (like the National Health Service Corps), and potentially a lower patient volume, which can improve work-life balance.
###
Practice Setting & Size
The type of institution you work for profoundly shapes your day-to-day work, compensation structure, and career trajectory.
- Academic Medical Centers / University Hospitals:
- Salary: Base salaries are often competitive but may be slightly lower on average than top-tier private practices. The compensation is often more structured and less flexible.
- Pros: Excellent benefits packages, strong retirement plans (often with pensions or generous 403(b) contributions), opportunities for teaching and research, access to cutting-edge technology and clinical trials, and a strong brand name on your resume. Great for those interested in the CAQ.
- Cons: Can be more bureaucratic, with less flexibility in scheduling and potentially higher administrative burdens.
- Large Private Multi-Specialty or Single-Specialty Groups:
- Salary: Often offers the highest earning potential, particularly for experienced PAs. Compensation is frequently tied to productivity (RVUs), meaning high-performing PAs can earn significantly more than their salaried counterparts.
- Pros: Potential for partnership/profit-sharing after several years, more autonomy and business-side involvement, and often more agile and less bureaucratic than large hospitals.
- Cons: Benefits may be less comprehensive than in academic settings. Income can be variable and dependent on patient volume, and there can be high pressure to be productive.
- Community Hospitals (Non-Profit or For-Profit):
- Salary: Highly variable. Non-profits may offer eligibility for Public Service Loan Forgiveness (PSLF). For-profit hospitals may offer more aggressive, productivity-based compensation.
- Pros: Often provide a good work-life balance and a strong sense of community. May serve a diverse patient population.
- Cons: May have fewer resources or sub-specialty support compared to large academic centers.
- Inpatient vs. Outpatient Roles:
- Inpatient/Neurocritical Care/Stroke Neurology: These roles often involve shift work (including nights and weekends) and managing critically ill patients. Due to the high acuity, intensity, and less desirable hours, these positions frequently command a higher base salary or shift differentials, pushing compensation higher.
- Outpatient Clinic: This is the more common setting, typically with a Monday-to-Friday schedule. While the base salary might be standard, the potential for productivity bonuses can be very high for an efficient PA managing a large patient panel.
###
Area of Sub-Specialization Within Neurology
Just as PAs specialize in neurology, they can further sub-specialize within it. Developing expertise in a niche, high-demand area can significantly boost earning potential, especially in procedural sub-specialties.
- Movement Disorders (e.g., Parkinson's, Dystonia): Involves complex medication management and often includes performing Botox injections for dystonia or programming Deep Brain Stimulation (DBS) devices, which are valuable, billable skills.
- Multiple Sclerosis (MS): Requires expertise in managing complex and expensive disease-modifying therapies (DMTs), many of which are administered via infusion. PAs who run or help manage an infusion suite are valuable assets.
- Epilepsy: PAs with the ability to perform initial readings of EEGs (always confirmed by a neurologist) are highly sought after, particularly in epilepsy monitoring units (EMUs).
*