Are you a nurse driven by a profound desire to alleviate suffering? Do you possess a unique blend of clinical acumen, deep empathy, and unwavering patience? If so, a career in pain management nursing might not only be your calling but also a pathway to a highly rewarding and financially stable profession. This specialized field is at the forefront of healthcare, tackling one of medicine's most complex and universal challenges: human pain. As demand for skilled pain specialists grows, the pain management nurse salary reflects the critical value these professionals bring to patients and healthcare systems alike.
This guide is designed to be your definitive resource, whether you're a nursing student charting your future, a seasoned RN seeking a new specialization, or simply curious about this vital career. We will dissect every facet of compensation, explore the factors that can significantly boost your earnings, and lay out a clear, actionable roadmap to enter and excel in this field. I once had a family member whose life was completely transformed by a pain management nurse. After years of struggling with debilitating chronic back pain, it was a dedicated nurse who finally coordinated a plan—blending physical therapy, minimally invasive procedures, and patient education—that gave him his life back. That experience solidified my belief that these nurses are not just caregivers; they are architects of hope and restoration.
Here's everything we'll cover to help you build your own successful career in this impactful specialty.
### Table of Contents
- [What Does a Pain Management Nurse Do?](#what-does-a-pain-management-nurse-do)
- [Average Pain Management Nurse Salary: A Deep Dive](#average-pain-management-nurse-salary-a-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors-that-influence-your-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Become a Pain Management Nurse: A Step-by-Step Guide](#how-to-become-a-pain-management-nurse-a-step-by-step-guide)
- [Conclusion: Is a Career in Pain Management Nursing Right for You?](#conclusion-is-a-career-in-pain-management-nursing-right-for-you)
What Does a Pain Management Nurse Do?

A Pain Management Nurse is a registered nurse (RN) who specializes in the assessment, treatment, and management of patients experiencing pain. This can range from acute pain, such as that following surgery or trauma, to complex, long-term chronic pain resulting from conditions like arthritis, fibromyalgia, cancer, or nerve damage. Their primary goal is not just to medicate but to improve a patient's overall quality of life, function, and well-being through a comprehensive, and often interdisciplinary, approach.
These nurses are expert communicators and patient advocates. They work closely with a team that may include physicians (anesthesiologists, physiatrists), surgeons, physical therapists, occupational therapists, psychologists, and social workers to create holistic and individualized care plans. They are the crucial link who translates complex medical strategies into practical, day-to-day relief for the patient.
Core Responsibilities and Daily Tasks:
The duties of a pain management nurse are diverse and require a high level of clinical skill and emotional intelligence. Key responsibilities include:
- Comprehensive Patient Assessment: Conducting detailed assessments of a patient's pain, including its location, intensity, duration, and character. They use standardized pain scales (like the 0-10 numeric rating scale) but also delve deeper into how the pain impacts the patient's daily activities, sleep, mood, and relationships.
- Developing Care Plans: Collaborating with the interdisciplinary team to create, implement, and continuously evaluate a patient's pain management plan.
- Administering Treatments: This can include a wide array of interventions:
- Pharmacological: Administering oral, intravenous, or topical pain medications, including non-opioids, adjuvants, and, when appropriate, opioids, while carefully monitoring for side effects and efficacy.
- Interventional: Assisting physicians with procedures such as nerve blocks, epidural steroid injections, joint injections, and the placement of spinal cord stimulators or intrathecal pain pumps.
- Non-Pharmacological: Implementing and teaching complementary therapies like Transcutaneous Electrical Nerve Stimulation (TENS), heat/cold therapy, relaxation techniques, and mindfulness.
- Patient and Family Education: This is a cornerstone of the role. They educate patients about their condition, the purpose of their medications, potential side effects, and self-management strategies. This empowerment is critical for long-term success, especially in chronic pain.
- Advocacy and Coordination: Acting as the patient's primary advocate, ensuring their pain is taken seriously and their care is well-coordinated across different providers and settings.
- Meticulous Documentation: Charting all assessments, interventions, patient responses, and communications to ensure continuity of care and legal compliance.
### A Day in the Life of an Outpatient Pain Clinic Nurse
To make this role more tangible, let's walk through a typical day for a pain management nurse in an outpatient clinic:
- 8:00 AM - Morning Huddle: The day begins with a team meeting. The nurse, physicians, and medical assistants review the day's patient schedule, flagging complex cases, upcoming procedures, and any patients who require follow-up calls.
- 8:30 AM - First Patient: New Consultation: The nurse meets with a new patient suffering from chronic sciatica. She spends 30 minutes conducting a thorough history and pain assessment, building rapport, and explaining the clinic's philosophy.
- 9:30 AM - Procedure Assist: The nurse preps a patient for a lumbar epidural steroid injection. She reviews the consent form, takes vital signs, establishes IV access, and positions the patient. During the procedure, she monitors the patient's vital signs and comfort level, assisting the physician as needed.
- 10:30 AM - Post-Procedure Recovery & Education: The nurse monitors the patient from the previous procedure, assessing for any adverse effects and providing detailed post-procedure instructions on activity, potential side effects, and when to call the clinic.
- 11:15 AM - Follow-up Appointment: A patient with fibromyalgia comes in for a 3-month follow-up. The nurse reviews their medication log, discusses the effectiveness of their current regimen, and explores how their non-pharmacological strategies (like gentle yoga and a sleep routine) are working. They collaboratively set new goals for the next three months.
- 12:30 PM - Lunch & Charting: A much-needed break to eat and catch up on detailed documentation from the morning's encounters.
- 1:30 PM - Patient Phone Calls: The nurse spends an hour returning calls. One patient needs a prescription refill, another is reporting a flare-up and needs advice on short-term management, and a third has a question about a new medication.
- 2:30 PM - Assisting with a Spinal Cord Stimulator Trial: A patient is undergoing a trial for a spinal cord stimulator. The nurse assists with the procedure and then spends significant time educating the patient on how to use the device's remote control to manage their pain over the next week.
- 4:00 PM - Care Coordination: The nurse calls a patient's physical therapist to provide an update on a recent medication change and discuss how to modify their therapy plan accordingly.
- 4:30 PM - Prep for Tomorrow: The nurse reviews charts for the next day's patients, ensuring all necessary lab results and imaging reports are available. She flags any urgent issues for the morning huddle.
- 5:00 PM - End of Shift: After a final round of charting, the nurse's day is complete, having directly impacted the comfort and well-being of over a dozen individuals.
Average Pain Management Nurse Salary: A Deep Dive
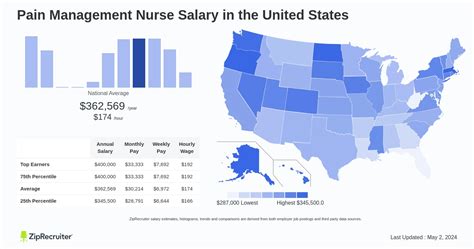
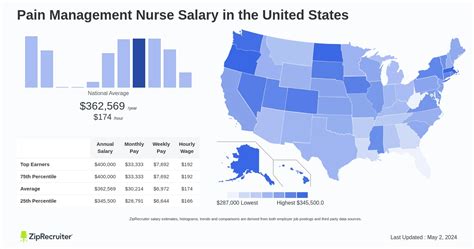
The compensation for a pain management nurse is highly competitive, reflecting the specialized skills, advanced knowledge, and emotional resilience required for the role. While salaries can vary significantly based on the factors we'll explore in the next section, we can establish a strong baseline using data from leading compensation aggregators.
As a specialized role, the pain management nurse salary is often higher than that of a generalist Registered Nurse. The U.S. Bureau of Labor Statistics (BLS) reports that the median annual wage for all Registered Nurses was $86,070 as of May 2023. However, specialists in high-demand fields like pain management typically earn a premium.
According to data from Salary.com updated in late 2023, the average Pain Management Nurse salary in the United States is approximately $101,570 per year. The typical salary range falls between $90,120 and $114,350. This demonstrates that the majority of practicing pain management nurses earn well into the six figures.
Payscale.com, which aggregates self-reported salary data, indicates a similar average base salary of around $80,000 per year, but this often doesn't include bonuses or overtime, which can be significant. Their data does show a clear and rewarding progression with experience.
### Salary by Experience Level
One of the most compelling aspects of this career is the strong potential for salary growth as you accumulate experience and expertise. Your value to an organization increases dramatically as you move from a novice practitioner to a seasoned expert who can handle the most complex cases and mentor junior staff.
Here is a breakdown of the typical salary progression for a Pain Management Nurse, compiled from industry data:
| Experience Level | Typical Years of Experience | Average Annual Salary Range | Key Responsibilities & Skills |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $75,000 - $90,000 | Performing basic pain assessments, administering medications under supervision, learning to assist with minor procedures, focusing on patient education fundamentals. |
| Mid-Career | 3-9 Years | $90,000 - $110,000 | Independently managing a caseload of patients, assisting with complex interventional procedures, developing comprehensive care plans, beginning to mentor new nurses. |
| Senior/Lead | 10-19 Years | $110,000 - $125,000+ | Managing the most complex patient cases, leading quality improvement projects, acting as a charge nurse or team lead, precepting students and new hires, often holding specialty certification. |
| Advanced Practice | 10+ Years (with MSN/DNP) | $120,000 - $160,000+ | Working as a Nurse Practitioner (NP) or Clinical Nurse Specialist (CNS) with prescriptive authority, performing certain procedures independently, designing and leading pain programs. |
*Sources: Salary.com, Payscale.com, and analysis of job postings on Glassdoor and Indeed.*
### Beyond the Base Salary: Understanding Total Compensation
Your annual salary is only one piece of the puzzle. To get a true picture of your earning potential, you must consider the total compensation package, which can add substantial value. When evaluating a job offer, look closely at these components:
- Bonuses: Many healthcare systems offer annual performance-based bonuses tied to patient satisfaction scores, quality metrics, or financial targets. Sign-on bonuses, sometimes reaching $10,000-$20,000 or more in high-demand areas, are also common for experienced nurses.
- Overtime Pay: In hospital or 24/7 care settings, opportunities for overtime are common. Nursing pay structures typically mandate time-and-a-half for hours worked beyond 40 per week, which can significantly increase your take-home pay.
- On-Call Pay & Call-Back Pay: Nurses in roles requiring on-call availability (e.g., for acute pain services in a hospital) receive a small hourly stipend just for being on-call. If they are called into work, they receive a higher rate of pay, often time-and-a-half, for a guaranteed minimum number of hours.
- Shift Differentials: Nurses who work evenings, nights, or weekends almost always earn a "shift differential," which is an extra dollar amount added to their hourly base rate. This can add up to several thousand dollars per year.
- Health and Wellness Benefits: A comprehensive benefits package is worth thousands of dollars. This includes medical, dental, and vision insurance. Look for low-premium, low-deductible plans.
- Retirement Savings Plans: Most employers offer a retirement plan like a 401(k) or, for non-profits, a 403(b). The most valuable part of this is the employer match. A common match is 50% of your contribution up to 6% of your salary—this is essentially free money and a critical component of your long-term financial health.
- Paid Time Off (PTO): This includes vacation days, sick leave, and holidays. Generous PTO policies are a hallmark of a good employer and contribute to a healthy work-life balance.
- Tuition Reimbursement & Professional Development Funds: Many healthcare systems invest in their nurses' growth. They may offer tuition reimbursement for pursuing a BSN, MSN, or DNP, and provide an annual stipend to cover the cost of conferences, continuing education units (CEUs), and certification fees. This is a direct investment in your future earning potential.
When comparing job offers, it's essential to look beyond the base salary and calculate the total value of the entire compensation package. A job with a slightly lower base salary but an excellent retirement match, low-cost health insurance, and generous tuition reimbursement may be the better long-term financial choice.
Key Factors That Influence Your Salary
While national averages provide a useful benchmark, your personal pain management nurse salary will be determined by a specific set of interconnected factors. Understanding these variables empowers you to make strategic career decisions that maximize your earning potential. This is the most critical section for anyone looking to not just enter the field, but to thrive in it financially.
###
1. Level of Education and Certification
Your educational foundation is the single most powerful lever you can pull to influence your salary trajectory over the course of your career.
Associate Degree in Nursing (ADN) vs. Bachelor of Science in Nursing (BSN):
While you can become an RN with an ADN, the industry has a strong and growing preference for BSN-prepared nurses. Many major hospital systems, particularly Magnet-designated hospitals, now require a BSN for specialty roles like pain management. This preference is reflected in pay. Nurses with a BSN can expect to earn $5,000 to $10,000 more per year on average than their ADN-prepared colleagues in similar roles. A BSN is also the required stepping stone for all advanced practice nursing roles.
Master of Science in Nursing (MSN) / Doctor of Nursing Practice (DNP):
This is where salary potential truly skyrockets. Earning an MSN or DNP allows you to become an Advanced Practice Registered Nurse (APRN), such as a Nurse Practitioner (NP) or a Clinical Nurse Specialist (CNS). In a pain management context, an NP can:
- Diagnose and treat pain conditions.
- Prescribe medications, including controlled substances.
- Perform certain interventional procedures (e.g., trigger point injections).
- Bill insurance directly for their services.
Because of this expanded scope of practice, the compensation is significantly higher. According to the BLS, the median salary for Nurse Practitioners was $128,490 per year as of May 2023, with many in specialized fields like pain management earning well over $150,000.
Specialty Certification: The Gold Standard
For RNs, the most important credential for maximizing salary and demonstrating expertise is professional certification. The premier credential is the Pain Management Nursing Certification (PMGT-BC®) offered by the American Nurses Credentialing Center (ANCC).
To be eligible for this exam, you must have:
- An active RN license.
- Two years of full-time practice as an RN.
- A minimum of 2,000 hours of clinical practice in pain management nursing within the last 3 years.
- 30 hours of continuing education in pain management within the last 3 years.
Holding the PMGT-BC credential is a clear signal to employers that you possess a validated, high-level body of knowledge in the specialty. Many institutions offer a direct salary differential or an annual bonus (often $1,000 - $3,000 per year) for certified nurses. More importantly, it makes you a far more competitive candidate for higher-paying jobs and leadership positions.
###
2. Years of Experience
As detailed in the salary progression table, experience is a primary driver of income. Clinical experience is not just about time served; it's about the accumulation of wisdom, confidence, and skill.
- Novice (0-2 years): In this phase, you are building foundational skills and confidence. Your focus is on mastering assessment techniques, understanding medication protocols, and learning procedural workflows.
- Competent (3-5 years): You can now manage common pain scenarios independently and efficiently. Your speed, critical thinking, and ability to anticipate patient needs have improved, making you a more valuable team member. Salary growth is steady during this period.
- Proficient/Expert (5-15+ years): You have seen a vast range of cases, including the rare and complex. You are a go-to resource for others, adept at handling difficult patient conversations, and capable of mentoring junior nurses. You may take on informal leadership roles (like precepting) or formal ones (like charge nurse), both of which come with pay bumps. At this stage, your salary often enters the top quartile for the profession. Senior nurses with 20+ years of experience in top-paying locations can command salaries exceeding $130,000 even without an advanced degree.
###
3. Geographic Location
Where you choose to work has a massive impact on your paycheck. Salaries are not uniform across the country; they are heavily influenced by local market demand, cost of living, and the presence of unions or powerful healthcare systems.
Highest-Paying States for Nurses:
States with a high cost of living and strong nursing unions consistently offer the highest salaries. According to BLS data for all Registered Nurses (which serves as a strong proxy for specialist roles), the top-paying states are:
| State | Annual Mean Wage (for all RNs) |
| :--- | :--- |
| California | $137,690 |
| Hawaii | $119,710 |
| Oregon | $109,620 |
| Washington | $107,720 |
| Alaska | $106,690 |
A pain management nurse in San Francisco, CA, could easily earn $140,000 - $160,000 or more, whereas the same role in a rural part of a lower-paying state might offer $75,000.
Highest-Paying Metropolitan Areas:
The salary premium is even more pronounced at the city level. The top-paying metro areas are almost exclusively in California:
| Metropolitan Area | Annual Mean Wage (for all RNs) |
| :--- | :--- |
| San Jose-Sunnyvale-Santa Clara, CA | $175,370 |
| San Francisco-Oakland-Hayward, CA | $166,130 |
| Vallejo-Fairfield, CA | $158,540 |
| Salinas, CA | $152,650 |
| Sacramento-Roseville-Arden-Arcade, CA | $148,680 |
It is crucial, however, to balance these high salaries against the equally high cost of living in these areas. A high salary in San Francisco may not give you more purchasing power than a good salary in a city with a lower cost of living, like Houston, TX, or Phoenix, AZ.
###
4. Work Setting & Type of Employer
The type of facility you work in directly correlates with your salary, benefits, and work-life balance.
- Large, Urban Academic Medical Centers: These institutions, often affiliated with universities, typically offer competitive salaries and excellent benefits packages, including robust tuition reimbursement. They handle the most complex cases, providing unparalleled learning opportunities.
- Private Hospitals & Health Systems: Compensation can be very high, especially in for-profit systems competing for talent. They often offer substantial sign-on bonuses and performance-based incentives.
- Outpatient Pain Management Clinics: These are a common setting for pain nurses. Salaries are generally strong, and a major benefit is the work schedule—typically regular business hours with no nights, weekends, or major holidays. This work-life balance can be a significant non-monetary benefit.
- Government/Veterans Affairs (VA) Hospitals: VA and other federal government positions operate on the General Schedule (GS) pay scale. While the base salary may sometimes start lower than the top private sector jobs, the benefits are often superior, including a generous pension plan (FERS), excellent job security, and ample paid leave.
- Surgical Centers (Ambulatory Surgery Centers): These facilities focus on acute, post-operative pain. The work is fast-paced, and the compensation is often competitive, with a schedule similar to outpatient clinics.
###
5. Area of Sub-Specialization
Within the broad field of pain management, further specialization can lead to higher pay, particularly in procedure-heavy areas.
- Interventional Pain Management: This is one of the highest-paying sub-specialties for an RN. These nurses work directly with physicians performing minimally invasive procedures like spinal cord stimulator placements, radiofrequency ablation, and nerve blocks. The high level of technical skill required commands a salary premium.
- Acute Pain Service (APS): Working on an APS team within a hospital involves managing complex post-operative and trauma pain, often using advanced techniques like epidurals and patient-controlled analgesia (PCA) pumps. The critical nature of this work is often well-compensated.
- Oncology Pain Management: Specializing in managing pain for cancer patients is a highly respected and demanding role. Nurses with expertise in both oncology and pain are valuable assets to cancer centers.
- Chronic Pain/Neuropathic Pain: While all pain nurses manage chronic conditions, those who become experts in specific, hard-to-treat areas like complex regional pain syndrome (CRPS) or diabetic neuropathy can become highly sought-after specialists.
###
6. In-Demand Skills
Beyond credentials, specific, demonstrable skills can make you a more attractive candidate and give you leverage in salary negotiations.
- Technical Skills: Proficiency with advanced equipment and procedures is a major plus. This includes experience with ultrasound guidance for injections, programming and troubleshooting intrathecal pain pumps and spinal cord stimulators, and managing complex infusions.
- Bilingualism: In diverse areas, being fluent in a second language (especially Spanish) is a huge asset and can sometimes come with a pay differential. It breaks down communication barriers and improves patient safety and satisfaction.
- Leadership and Mentoring: Experience as a charge nurse, preceptor, or team lead demonstrates leadership capabilities that are valuable for any organization and can justify a higher salary.
- **Knowledge of