Introduction

For those drawn to the intricate challenges of medicine and the profound responsibility of caring for its most vulnerable patients, the field of pediatric anesthesiology stands as a pinnacle of professional achievement. It is a career that demands an exceptional blend of scientific expertise, technical precision, and deep compassion. You are not just a physician; you are the guardian of a child’s safety and comfort during their most frightening moments. This immense responsibility is met with significant professional rewards, including a highly competitive salary that reflects the years of dedicated training and the critical nature of the work. For those considering this path, the average salary pediatric anesthesiologist professionals command often ranges from $400,000 to well over $600,000 annually, depending on a host of factors we will explore in detail.
This is more than just a job; it’s a calling. I recall standing in a sterile hospital corridor, my own heart pounding, as my young nephew was wheeled into surgery. The person who calmed not just him, but my entire family, was the pediatric anesthesiologist. With a calm demeanor and gentle confidence, she explained every step, transforming a moment of terror into one of trust. In that moment, I understood that her role was as much about managing fear as it was about managing physiology.
This guide is designed to be your definitive resource, whether you are a medical student dreaming of this specialty, a resident weighing your fellowship options, or simply curious about one of medicine’s most demanding and rewarding careers. We will dissect every component of a pediatric anesthesiologist's professional life, from their daily duties to the intricate factors that shape their substantial income.
### Table of Contents
- [What Does a Pediatric Anesthesiologist Do?](#what-does-a-pediatric-anesthesiologist-do)
- [Average Pediatric Anesthesiologist Salary: A Deep Dive](#average-pediatric-anesthesiologist-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Pediatric Anesthesiologist Do?

To understand the compensation, one must first appreciate the complexity of the role. A pediatric anesthesiologist is a perioperative physician who provides anesthesia and pain management for infants, children, and adolescents. Their expertise extends far beyond simply administering medication to induce sleep. Children are not "little adults"; their physiology, anatomy, and psychological needs are fundamentally different and change dramatically from a one-day-old neonate to a seventeen-year-old teenager.
The core of the job revolves around three critical phases of surgical care:
1. Preoperative Evaluation: This is where the anesthesiologist's work begins. They meet with the child and their parents/guardians to conduct a thorough medical history review, perform a physical examination, and assess any underlying conditions (e.g., congenital heart disease, asthma, developmental delays). This is also a crucial time for building rapport and trust, explaining the anesthesia plan in age-appropriate terms, and alleviating the anxieties of both the patient and their family. They determine the safest anesthesia plan, considering the type of surgery, the child's health status, and their unique physiological needs.
2. Intraoperative Management: Inside the operating room, the pediatric anesthesiologist is the child's silent, vigilant protector. They induce anesthesia, secure the airway (which can be incredibly challenging in small infants), and then meticulously monitor the patient’s vital signs throughout the entire procedure. This includes managing heart rate, blood pressure, oxygen levels, temperature, and fluid balance. They must be prepared to respond instantly to any complication, from an allergic reaction to major blood loss, making life-or-death decisions in seconds.
3. Postoperative Care: The job doesn’t end when the surgery is over. The anesthesiologist ensures the child emerges from anesthesia safely and comfortably in the Post-Anesthesia Care Unit (PACU). They are experts in pediatric pain management, employing a variety of techniques from intravenous medications to complex regional nerve blocks to minimize postoperative discomfort. They follow the patient's recovery, managing any side effects like nausea and ensuring a smooth transition back to the hospital ward or home.
### A Day in the Life of a Pediatric Anesthesiologist
To make this tangible, consider a typical day at a children's hospital:
- 6:30 AM: Arrive at the hospital. Change into scrubs, grab a coffee, and review the day’s surgical list. The first case is a 2-year-old undergoing a hernia repair, followed by a 6-month-old with a congenital heart defect, and an 8-year-old for an emergency appendectomy.
- 7:00 AM: Head to the preoperative holding area to meet the first patient and their family. The toddler is crying and scared. You use a calm voice, a bubble wand, and a tablet with cartoons to build rapport. You speak with the parents, answer their questions, confirm the child hasn't eaten, and get their final consent.
- 7:45 AM: You accompany the child to the operating room. To avoid a traumatic separation, you allow the child to breathe anesthetic gas through a flavored mask while sitting on your lap until they are gently asleep.
- 8:00 AM - 9:00 AM: You expertly place an IV and a breathing tube. Throughout the surgery, your eyes are glued to the monitors. You adjust anesthetic depth, administer fluids, and keep the patient perfectly stable.
- 9:15 AM: The surgery is complete. You wake the child up gently and transfer them to the PACU, giving a detailed report to the recovery nurse. You stay until you are certain the child is stable and their initial pain is well-managed.
- 9:30 AM - 4:00 PM: The cycle repeats. You move to the next operating room to care for the infant with the complex heart condition, a case requiring advanced monitoring like an arterial line. Later, you manage the emergency appendectomy, which involves a rapid assessment and plan. In between cases, you might handle consultations for pain management on the pediatric floor or supervise residents.
- 4:30 PM: You complete your final case of the day. You do one last round on your patients in the PACU, ensuring their pain is controlled and they are recovering well.
- 5:30 PM: You complete your charting for the day, detailing the anesthetic records for each patient. You then hand over any ongoing patient care issues to the on-call anesthesiologist before heading home—unless you are the one on call.
This is a profession of immense focus, resilience, and medical acumen, where a calm head and steady hand directly translate into a child’s well-being.
Average Pediatric Anesthesiologist Salary: A Deep Dive
Given the extensive training—at least 13 years post-high school—and the high-stakes nature of the job, pediatric anesthesiologists are among the highest-paid medical specialists. While exact figures fluctuate, a comprehensive analysis of recent data provides a clear picture of their earning potential.
Anesthesiology, as a specialty, consistently ranks in the top 10 for physician compensation. According to the Medscape Physician Compensation Report 2023, the average salary for an anesthesiologist is $448,000. It's crucial to note that pediatric anesthesiology is a sub-specialty, and this specialization often commands a premium, placing practitioners at or above this average.
More specific data from salary aggregators reflects this. Salary.com, which allows for filtering by specialty, reports the median salary for a Pediatric Anesthesiologist in the United States as $451,101 as of late 2023, with a typical range falling between $390,701 and $511,501.
However, these numbers only tell part of the story. The "average" can be misleading as it blends starting salaries with the earnings of highly experienced partners in private practice. A more granular look reveals a clear progression.
### Salary by Experience Level
The career trajectory for a pediatric anesthesiologist shows significant financial growth, particularly in the first decade of practice.
| Experience Level | Typical Timeframe | Average Annual Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level | Years 1-3 (Post-Fellowship) | $350,000 - $425,000 | Often salaried positions in hospitals or academic centers. May include sign-on bonuses. |
| Mid-Career | Years 4-15 | $425,000 - $550,000+ | Potential for partnership in private practice. Productivity bonuses (RVU-based) become a major factor. |
| Senior/Experienced | Years 15+ | $500,000 - $650,000+ | Peak earning years. Often includes income from partnership, administrative stipends (e.g., Medical Director), and investment returns from the practice. |
*(Source: Data compiled and synthesized from Medscape, Doximity, Salary.com, and Merritt Hawkins reports, 2022-2024.)*
### A Closer Look at the Total Compensation Package
The base salary is just one piece of a complex compensation puzzle. A pediatric anesthesiologist's total earnings are a combination of several components that can add tens or even hundreds of thousands of dollars to their annual income.
- Base Salary: This is the guaranteed income paid for fulfilling the core duties of the job description. In academic and hospital-employed models, this makes up the bulk of the compensation.
- Productivity Bonuses: This is a major driver of income, especially in private practice and many hospital-employed models. Compensation is often tied to Relative Value Units (RVUs), a measure used by Medicare to value the work involved in a medical procedure. The more cases or the more complex the cases an anesthesiologist handles, the more RVUs they generate, and the higher their bonus.
- Sign-On Bonus: To attract top talent, particularly in less-desirable locations or competitive markets, hospitals and practices often offer substantial sign-on bonuses. These can range from $25,000 to $100,000 or more.
- Call Pay: Anesthesiologists are required to be "on call" for nights, weekends, and holidays to handle emergencies. This is often compensated separately, either as a daily stipend (e.g., $1,000 - $2,500 per night) or through extra pay for any cases performed while on call. Taking more call is a direct way to increase income.
- Partnership/Profit Sharing: In private practice, after a few years as an employee, an anesthesiologist may be offered the opportunity to "buy-in" and become a partner. This is a significant financial milestone. Partners not only receive their clinical salary but also share in the profits of the entire group, which can dramatically increase their total compensation.
- Retirement Benefits: Strong retirement plans are standard. This typically includes a 401(k) or 403(b) with a generous employer match. Private practices may offer more advanced options like profit-sharing or defined-benefit plans.
- Other Benefits: The value of a comprehensive benefits package cannot be overstated. This almost always includes:
- Full malpractice insurance coverage.
- Family health, dental, and vision insurance.
- Life and disability insurance.
- Continuing Medical Education (CME) allowance (typically $5,000 - $15,000 per year for conferences and educational materials).
- Generous paid time off (often 6-10 weeks per year).
When evaluating a job offer, it's essential to look at the total compensation, not just the base salary. A lower base salary with a strong productivity bonus structure and partnership track can be far more lucrative in the long run than a high salaried position with no upside.
Key Factors That Influence a Pediatric Anesthesiologist's Salary

The wide salary ranges presented above are driven by a predictable set of variables. Understanding these factors is crucial for any aspiring or practicing pediatric anesthesiologist looking to maximize their earning potential and make informed career decisions.
###
Level of Education and Board Certification
In medicine, the educational path is standardized and rigorous, serving as a baseline qualification rather than a variable for salary negotiation at the attending level. To become a pediatric anesthesiologist, one must complete:
1. A four-year bachelor's degree.
2. Four years of medical school (earning an M.D. or D.O.).
3. A four-year anesthesiology residency.
4. A one-year pediatric anesthesiology fellowship.
Upon completion, the final and most critical step is achieving board certification. This involves passing rigorous written and oral examinations administered by the American Board of Anesthesiology (ABA). A physician first becomes board-certified in general Anesthesiology and then obtains a subspecialty certification in Pediatric Anesthesiology.
Impact on Salary: Being board-certified is non-negotiable for any top-tier position. It is the gold standard that signifies a physician has met the highest standards of knowledge and practice. Virtually all hospitals and reputable private practices require it for employment and credentialing. Lacking board certification would severely limit job prospects and relegate a physician to lower-paying, less desirable positions.
Further sub-specialization, such as completing a second fellowship in pediatric cardiac anesthesia or pediatric pain medicine, can make a candidate exceptionally valuable to specialized children's hospitals, often leading to a salary premium or access to more coveted and complex (and thus higher-RVU) cases.
###
Years of Experience
As illustrated in the previous section, experience is a primary driver of salary growth. This progression is not merely a reward for loyalty; it reflects a genuine increase in skill, efficiency, and value to the practice or hospital.
- Early Career (Years 1-3): Physicians fresh out of fellowship are highly skilled but are still refining their efficiency and speed. Their salaries are high but are on the lower end of the spectrum. They are typically in salaried roles while they build their reputation and clinical volume. A 2023 Merritt Hawkins report noted that starting salaries for anesthesiologists can range from $350,000 to over $400,000, often with a sign-on bonus and relocation assistance.
- Mid-Career (Years 4-15): This is where the most significant income jump occurs. In a private practice setting, this is the typical timeframe for making partner. Once a partner, the physician's income is no longer just a salary; it's a share of the group's overall profits. Their clinical speed and confidence are at a peak, allowing them to handle a higher volume of cases and more complex procedures efficiently, thus maximizing RVU generation.
- Late Career (Years 15+): At this stage, physicians are at their peak earning potential. Their base compensation may be similar to mid-career colleagues, but their total income is often augmented by leadership roles. Many senior anesthesiologists take on administrative responsibilities, such as Medical Director of Anesthesia, Chief of Staff, or serving on key hospital committees. These roles typically come with a substantial annual stipend (e.g., $50,000 - $150,000+) on top of their clinical income.
###
Geographic Location
Where you practice has a monumental impact on your salary. This is largely governed by the law of supply and demand.
- Highest Paying Regions: According to Doximity's 2023 Physician Compensation Report, states in the Midwest and Southeast often offer the highest compensation for physicians. Cities like Milwaukee, Charlotte, and St. Louis report some of the highest average physician salaries. This is because these regions may have fewer anesthesiologists per capita, forcing hospitals and practices to offer more lucrative packages to attract and retain talent. For anesthesiologists, states like Wisconsin, Alabama, and Oklahoma are often cited as top-paying.
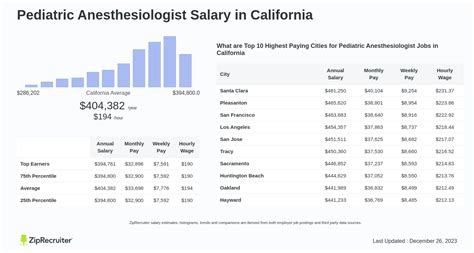
- Lower Paying Regions: Conversely, major metropolitan areas in the Northeast and on the West Coast (e.g., New York City, Boston, Los Angeles, San Francisco) tend to have lower average salaries. While this seems counterintuitive given the high cost of living, these areas are saturated with academic medical centers and are highly desirable places to live, creating a surplus of physicians competing for positions. This competition drives down compensation.
- Rural vs. Urban: There is a significant pay premium for working in a rural or underserved area. A hospital in rural Wyoming or North Dakota might offer a salary $50,000 to $100,000 higher than a comparable position in Chicago to compensate for the location. This "rural premium" is a powerful recruitment tool.
Here's a sample of how location can affect average anesthesiologist salaries (note: pediatric specialists are typically at or above these figures):
| State/Region | Average Anesthesiologist Salary | Why? |
| :--- | :--- | :--- |
| Wisconsin | ~$550,000+ | High demand, lower saturation of specialists. |
| California | ~$430,000 | High desirability, market saturation, managed care penetration. |
| Texas | ~$480,000 | Favorable business environment, mix of large urban centers and underserved areas. |
| New York | ~$415,000 | Highly saturated market, dominated by academic centers with lower pay scales. |
*(Source: Data synthesized from Doximity, Medscape, and various recruitment firm reports.)*
###
Practice Type and Setting
The structure of your employer is arguably the most significant factor determining both your salary and your day-to-day life.
- Private Practice (Physician-Owned Group): This model traditionally offers the highest earning potential. After a 1-3 year track, associates are offered partnership. As a partner, you are a business owner. Your income is directly tied to the group's performance and profits. This also means taking on business risks and administrative responsibilities. The compensation model is almost always based on productivity (RVUs). Top-earning pediatric anesthesiologists in successful private practice groups can earn upwards of $700,000 annually.
- Hospital-Employed (Large Health System): This is an increasingly common model. The hospital directly employs the physician. This offers more stability, predictable hours (in theory), and less administrative headache. The salary is competitive and often includes strong benefits, but the ceiling is typically lower than in private practice, as there is no profit-sharing component. Compensation models are often a mix of a base salary plus a productivity bonus. This is a great option for those who want to focus solely on clinical medicine without the burdens of running a business.
- Academic Medical Center: Working at a university-affiliated hospital involves a tripartite mission: clinical work, teaching, and research. Compensation is almost always lower than in private practice or even some hospital-employed settings. The median salary in academia might be 15-25% lower than in private practice. However, this is offset by non-monetary benefits: the prestige of a university appointment, the intellectual stimulation of teaching medical students and residents, opportunities for groundbreaking research, and often better benefits and more generous time off.
- Locum Tenens: This means "to hold a place." Locum tenens anesthesiologists are independent contractors who work temporary assignments (from a few days to several months) to fill in for physicians who are on vacation, on leave, or to cover staffing shortages. The pay is extremely high on a per-diem basis (often $2,500 - $4,000+ per day), but these positions do not include benefits, paid time off, malpractice "tail" coverage, or retirement contributions. It offers ultimate flexibility but lacks stability.
###
In-Demand Skills and Additional Responsibilities
Beyond the standard job description, certain skills and roles can add a significant premium to a pediatric anesthesiologist's salary.
- Leadership and Administrative Roles: As mentioned, taking on a leadership position like Medical Director, Department Chair, or Chief of Anesthesiology comes with an administrative stipend that can be very substantial. These roles require a significant time commitment for meetings, scheduling, quality control, and personnel management.
- Expertise in High-Acuity Sub-specialties: While pediatric anesthesia is already a specialty, deep expertise in even more niche areas increases one's value. A physician who is the go-to expert for neonatal surgery, pediatric cardiac cases, or complex spine surgery for scoliosis can command a higher salary or a greater share of high-RVU cases.
- Proficiency in Regional Anesthesia: Advanced skills in ultrasound-guided regional anesthesia are highly sought after. Placing complex nerve blocks (e.g., epidurals, spinal blocks, peripheral nerve blocks) for postoperative pain management can improve patient outcomes, reduce hospital stays, and decrease reliance on opioids. Anesthesiologists with these skills are a major asset to any surgical service.
- Productivity and Efficiency: In any model tied to RVUs, speed and efficiency are money. An anesthesiologist who can safely manage a quick turnover of cases—getting the next patient ready as the previous one is finishing—can generate significantly more RVUs over the course of a day than a slower colleague, directly impacting their bonus and overall value to the group.
Job Outlook and Career Growth

For those investing the immense time and effort required to enter this field, the long-term career outlook is exceptionally bright and stable. The demand for skilled anesthesiologists, particularly those with pediatric sub-specialty training, is projected to remain strong for the foreseeable future.
The U.S. Bureau of Labor Statistics (BLS), in its Occupational Outlook Handbook, projects that employment for all physicians and surgeons will grow by 3% from 2022 to 2032. While this is about the average for all occupations, the specifics for anesthesiology are more nuanced and robust. The BLS groups anesthesiologists with other physicians, but industry-specific data highlights a more pressing need.
A key driver of demand is the aging U.S. population, which will continue to require more surgical procedures. While this primarily affects adult care, it has a ripple effect on the entire healthcare system. Furthermore, advances in surgical techniques are making procedures possible for younger and sicker children who previously would have been considered inoperable, increasing the need for highly skilled pediatric anesthesiologists.
The Association of American Medical Colleges (AAMC) has consistently projected a significant physician shortage over the next decade, with specialty fields like anesthesiology being particularly affected. The long training pipeline means that the supply of new anesthesiologists cannot be rapidly increased to meet rising demand, which helps ensure both job security and strong salary leverage for those in the field.
### Emerging Trends and Future Challenges
The profession is not static. Several trends are shaping the future of pediatric anesthesiology:
- Shift to Ambulatory Surgery Centers (ASCs): An increasing number of pediatric procedures (e.g., ENT, urology, orthopedic) are moving from inpatient hospital settings to outpatient ASCs. This trend requires anesthesiologists who are skilled in techniques that allow for rapid recovery and discharge.
- Focus on Perioperative Surgical Home (PSH): This is a patient-centered, team-based model of care in which an anesthesiologist leads the entire perioperative experience, from pre-op optimization to post-discharge follow-up. This expands the role of the anesthesiologist beyond the OR and can improve outcomes and reduce costs.
- Technological Integration: The field is becoming more technologically advanced. This includes the use of advanced ultrasound for vascular access and regional blocks, new monitoring devices, and the potential for AI to assist in data interpretation and risk assessment.
- Scope of Practice: A persistent challenge and point of discussion in the field is the relationship with and role of Certified Registered Nurse Anesthetists (CRNAs). While most pediatric anesthesiologists work in a physician-led Anesthesia Care Team model, supervising CRNAs and residents, debates over independent practice for nurses continue in various state legislatures. Staying involved in professional advocacy through societies like the ASA is critical.
- Physician Burnout: The high-stress environment, long hours, and life-or-death responsibility place anesthesiologists at high risk for burnout.
