In a fast-paced world that glorifies hustle and often sacrifices rest, the silent epidemic of sleep deprivation and sleep disorders has reached a critical point. Millions of people suffer from conditions that disrupt their sleep, damaging their health, safety, and overall quality of life. In this landscape, a unique and increasingly vital medical specialist emerges: the Sleep Medicine Physician. For those drawn to a medical career that offers profound patient impact, intellectual challenge, and significant financial reward, understanding the realities of a sleep doctor salary and career path is the first step toward a fulfilling future. This career isn't just about interpreting charts; it's about giving people back their days by fixing their nights.
The financial prospects are compelling, with average salaries for sleep medicine physicians comfortably ranging from $250,000 to well over $400,000 annually, depending on a host of factors we will explore in detail. During my time analyzing healthcare compensation trends, I once spoke with a seasoned sleep physician who described her work not just as treating snoring, but as "restoring marriages, preventing car accidents, and giving patients the energy to play with their grandchildren." This profound impact, coupled with a highly competitive compensation package, makes sleep medicine one of the most uniquely rewarding subspecialties in modern medicine.
This guide will serve as your definitive resource, whether you're a medical student contemplating specialties or a seasoned physician considering a fellowship. We will dissect every component of a sleep doctor's career, from daily responsibilities and salary benchmarks to the specific skills and choices that can maximize your earning potential and professional growth.
### Table of Contents
- [What Does a Sleep Doctor Do?](#what-does-a-sleep-doctor-do)
- [Average Sleep Doctor Salary: A Deep Dive](#average-sleep-doctor-salary-a-deep-dive)
- [Key Factors That Influence a Sleep Doctor Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth in Sleep Medicine](#job-outlook-and-career-growth)
- [How to Become a Sleep Doctor: Your Step-by-Step Guide](#how-to-get-started-in-this-career)
- [Is a Career in Sleep Medicine Right for You?](#conclusion)
---
What Does a Sleep Doctor Do? An In-Depth Look

The term "sleep doctor" is a common way to describe a Sleep Medicine Physician, also known as a Somnologist. This is a highly specialized medical doctor (MD or DO) who has completed extensive training to become an expert in diagnosing, managing, and treating the full spectrum of sleep-related disorders. This is not a standalone residency; rather, it is a subspecialty fellowship undertaken *after* completing a full residency in a primary field such as internal medicine, pulmonology, neurology, psychiatry, otolaryngology (ENT), or family medicine.
A sleep doctor's primary mission is to solve complex puzzles related to a patient's sleep. Their work is a fascinating blend of clinical consultation, diagnostic interpretation, and long-term patient management. They address a wide array of conditions, including:
- Sleep Apnea: The most common disorder they treat, characterized by repeated pauses in breathing during sleep.
- Insomnia: Difficulty falling asleep, staying asleep, or experiencing non-restorative sleep.
- Narcolepsy: A chronic neurological condition involving overwhelming daytime sleepiness and sudden attacks of sleep.
- Restless Legs Syndrome (RLS): An uncontrollable urge to move the legs, typically in the evening.
- Parasomnias: Abnormal behaviors during sleep, such as sleepwalking, night terrors, or REM sleep behavior disorder.
- Circadian Rhythm Disorders: Problems with the internal body clock, often seen in shift workers or from jet lag.
The core responsibilities of a sleep medicine physician are multifaceted and require a diverse skill set. They don't just ask patients if they're tired; they delve deep into their health history, lifestyle, and symptoms to uncover the root cause of their sleep issues.
Daily Tasks and Responsibilities:
- Patient Consultations: Conducting thorough initial evaluations of new patients and managing follow-up appointments to track treatment progress.
- Interpreting Diagnostic Studies: This is a cornerstone of the specialty. Sleep doctors are experts at reading and interpreting polysomnograms (PSGs), which are overnight sleep studies that record brain waves, heart rate, breathing patterns, blood oxygen levels, and muscle activity. They also interpret home sleep apnea tests (HSATs) and other diagnostic tools.
- Developing Treatment Plans: Creating comprehensive, individualized treatment plans that may include:
- Prescribing Positive Airway Pressure (PAP) therapy, such as CPAP or BiPAP machines, for sleep apnea.
- Recommending oral appliances or surgical options.
- Prescribing medications for conditions like narcolepsy, RLS, or insomnia.
- Implementing behavioral therapies, most notably Cognitive Behavioral Therapy for Insomnia (CBT-I).
- Collaboration: Working closely with a multidisciplinary team of healthcare professionals, including primary care physicians, cardiologists, neurologists, dentists, and ENT surgeons, to provide holistic care.
- Patient Education: Spending significant time educating patients about their condition and the importance of treatment adherence, which is critical for long-term success.
### A Day in the Life of a Sleep Doctor
To make this tangible, let's imagine a typical day for Dr. Evelyn Reed, a hospital-employed sleep medicine physician.
- 7:30 AM - 9:00 AM: Interpreting Sleep Studies: Dr. Reed arrives at her office and logs into the hospital's electronic health record system. Her first task is to review the half-dozen polysomnograms that were conducted in the hospital's sleep lab the previous night. She meticulously analyzes the data, identifying apneic events, oxygen desaturations, and unusual brain wave patterns to finalize her diagnoses.
- 9:00 AM - 12:00 PM: Morning Clinic: She moves to her clinic to see patients. Her schedule includes a new patient with suspected narcolepsy, a follow-up with a truck driver to ensure his CPAP compliance meets Department of Transportation regulations, and a consultation with a patient suffering from chronic insomnia who is seeking non-pharmacological treatment options.
- 12:00 PM - 1:00 PM: Lunch and Administrative Time: Dr. Reed has a quick lunch while responding to patient messages, signing prescription refills, and calling a referring primary care physician to discuss a complex case.
- 1:00 PM - 4:00 PM: Afternoon Clinic: The afternoon brings more patients. She sees a patient for a "mask fitting" clinic to troubleshoot issues with their CPAP interface and consults with a patient who is a candidate for Inspire therapy, a hypoglossal nerve stimulator for sleep apnea.
- 4:00 PM - 5:30 PM: Charting and Follow-Up: The last part of her day is dedicated to completing her patient charts, dictating notes from the day's visits, and reviewing lab results. She also spends time preparing for a presentation she's giving to the internal medicine residents on screening for sleep apnea in patients with hypertension.
This "day in the life" illustrates that the career is far more than just prescribing CPAP machines. It is a dynamic, patient-focused, and intellectually stimulating field that sits at the intersection of multiple medical disciplines.
---
Average Sleep Doctor Salary: A Deep Dive
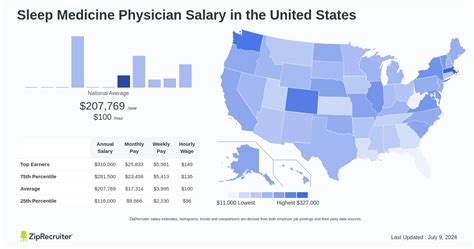
The compensation for a sleep medicine physician is among the highest in the medical field, reflecting the extensive training required and the high demand for their expertise. While salaries can vary significantly based on the factors we'll discuss in the next section, we can establish reliable benchmarks using data from leading industry sources.
It's important to note that salary aggregators often group sleep medicine with related specialties like Pulmonology or Neurology. The most accurate data comes from physician-specific compensation reports.
National Average Salary and Typical Range
According to the 2023 Medscape Physician Compensation Report, which surveys thousands of physicians across the United States, specialists in fields that commonly include sleep medicine report highly competitive incomes. While Medscape does not list "Sleep Medicine" as a standalone category, it provides data for the primary specialties from which sleep doctors emerge:
- Pulmonology: Average annual compensation of $378,000.
- Neurology: Average annual compensation of $313,000.
Other reputable sources provide more direct estimates for sleep medicine physicians.
- Salary.com reports that the average Sleep Medicine Physician salary in the United States is $299,021 as of late 2023, with a typical range falling between $262,442 and $353,243. This source is valuable as it captures a broad spectrum of employed physicians.
- Doximity's 2023 Physician Compensation Report notes that Sleep Medicine ranks among the top-paying specialties, with an average advertised salary on their platform often exceeding $300,000.
Based on a consolidation of these sources, a realistic and comprehensive national average salary for a full-time sleep medicine physician in the United States is approximately $320,000 per year. The overall salary spectrum is wide, starting around $240,000 for new graduates in lower-paying settings and reaching upwards of $500,000 or more for experienced physicians in private practice or high-demand locations.
### Salary by Experience Level
Like all professions, compensation in sleep medicine grows significantly with experience, expertise, and efficiency. As physicians build their patient base, refine their diagnostic skills, and become more proficient, their productivity—and thus their value to a practice or hospital—increases.
Here is a typical salary progression, combining data from various industry reports:
| Experience Level | Years in Practice | Typical Annual Salary Range | Key Characteristics |
| ----------------------- | ----------------- | --------------------------------- | ---------------------------------------------------------------------------------------------------------------- |
| Entry-Level | 0-3 years | $240,000 - $290,000 | Post-fellowship; often includes a guaranteed salary for the first 1-2 years before transitioning to a productivity-based model. |
| Mid-Career | 4-10 years | $290,000 - $380,000 | Established patient panel, high efficiency in clinic and sleep study interpretation, strong referral network. Peak productivity. |
| Senior / Experienced| 11+ years | $350,000 - $500,000+ | Often hold leadership roles (e.g., Medical Director of a sleep center), may be a partner in a private practice, or have a highly specialized niche. |
*Source: Synthesized data from Medscape, Doximity, Salary.com, and Merritt Hawkins physician salary reports.*
### Deconstructing the Compensation Package
A sleep doctor's total compensation is more than just their base salary. Understanding the full package is crucial for evaluating job offers.
- Base Salary: This is the guaranteed, fixed portion of your pay. In hospital-employed models, this is often the largest component, especially in the first few years.
- Production Bonuses (RVU-Based): This is the most common form of incentive pay. RVU stands for Relative Value Unit, a standardized measure used by Medicare to determine the value of physician services. Physicians are often given a target number of RVUs to generate, and they earn a bonus for every RVU produced above that threshold. A sleep physician generates RVUs from clinic visits, sleep study interpretations, and procedures. This model directly rewards hard work and efficiency.
- Quality Bonuses: An increasing number of health systems are tying a portion of compensation to quality metrics. This could include patient satisfaction scores, treatment adherence rates (e.g., CPAP compliance), or achieving specific clinical outcomes.
- Profit Sharing / Partnership Track (Private Practice): For those in private practice, the ultimate financial goal is often partnership. Partners share in the profits of the entire practice, leading to significantly higher income potential than an employed physician model. This also comes with the responsibilities of business ownership.
- Ancillary Income: Some physicians earn extra income from roles like:
- Medical Directorship: Serving as the Medical Director of a sleep lab carries a stipend, typically ranging from $20,000 to $60,000 per year, on top of clinical income.
- Expert Witness Testimony: Providing legal consultation in cases related to sleep disorders (e.g., accidents caused by drowsy driving).
- Consulting: Advising medical device or pharmaceutical companies.
- Comprehensive Benefits: The value of a benefits package can be substantial, often worth an additional $50,000-$80,000 per year. This typically includes:
- Malpractice Insurance: Almost always covered by the employer.
- Health, Dental, and Vision Insurance: For the physician and their family.
- Retirement Plans: Generous 401(k) or 403(b) plans with employer matching.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $3,000-$5,000) and paid time off to attend conferences and stay current.
- Paid Time Off (PTO): Typically 4-6 weeks per year.
- Relocation Bonus / Sign-On Bonus: Often offered to attract physicians, sometimes ranging from $10,000 to $50,000.
---
Key Factors That Influence a Sleep Doctor Salary

A national average provides a useful benchmark, but an individual's actual salary is determined by a complex interplay of several key factors. Aspiring and practicing sleep physicians can strategically leverage these variables to maximize their earning potential throughout their careers. This section provides a granular analysis of what truly moves the needle on compensation.
###
1. Level of Education and Board Certification
While all sleep medicine physicians must complete medical school (MD or DO), a residency, and a fellowship, the specific pathway and certifications have a significant impact on employability and salary.
- The Foundation: MD or DO: The path begins with a Doctor of Medicine or Doctor of Osteopathic Medicine degree.
- Residency Training: The choice of residency sets the foundation. The most common pathways are Internal Medicine, Pulmonology/Critical Care, Neurology, and Psychiatry. Otolaryngology (ENT) and Family Medicine are also viable routes. Physicians from specialties that are procedure-heavy or deal with more complex comorbidities (like Pulmonology or Neurology) may have a slight edge in certain practice settings.
- The Sleep Medicine Fellowship: This one-year, ACGME-accredited program is mandatory. Successful completion makes a physician "fellowship-trained."
- Board Certification: The Crucial Differentiator: Being "board certified" in Sleep Medicine is the gold standard and a non-negotiable for most high-paying jobs. After fellowship, a physician must pass the Sleep Medicine Certification Examination offered by their primary board (e.g., the American Board of Internal Medicine, the American Board of Psychiatry and Neurology). Board certification signifies the highest level of expertise and is essential for hospital credentialing and optimal insurance reimbursement. An uncertified physician will earn significantly less and have fewer job opportunities.
###
2. Years of Experience and Career Trajectory
Experience is arguably the most powerful driver of salary growth in a productivity-based environment. The earning curve for a sleep physician is not linear; it often follows a distinct arc.
- Years 1-3 (The Building Phase): A new graduate is often on a guaranteed salary. Their focus is on building a patient roster, establishing relationships with referring physicians, and becoming efficient with clinic workflow and sleep study interpretation. Their RVU production will be at its lowest point during this phase. Projected Salary: $240,000 - $290,000.
- Years 4-15 (The Peak Earning Phase): By this stage, the physician has a full patient panel, a robust referral network, and has mastered the art of efficient practice. They can interpret a higher volume of sleep studies and manage a busy clinic schedule, leading to maximum RVU production. This is the period of highest clinical income. Projected Salary: $300,000 - $450,000.
- Years 16+ (The Leadership/Legacy Phase): While clinical productivity may plateau or slightly decrease, senior physicians often transition into higher-value roles that supplement their income. They may become the Medical Director of the sleep center, take on system-wide administrative duties, become a partner in a private practice, or dedicate more time to research and teaching. This shift maintains or even increases their overall compensation. Projected Salary: $350,000 - $500,000+.
###
3. Geographic Location: The Power of Place
Where you choose to practice has a profound impact on your salary, often creating variations of $100,000 or more for the same job. The core principle is supply and demand. Areas with a high cost of living and a saturation of specialists (e.g., major coastal cities) tend to offer lower salaries than less populated regions desperate for specialized medical care.
- Highest Paying Regions: According to Merritt Hawkins' 2023 review of physician recruiting incentives, the Midwest, Southeast, and other non-coastal rural regions consistently offer the highest salaries. States like North Dakota, Wisconsin, Alabama, Oklahoma, and Indiana often top the list. A sleep physician in a mid-sized Midwestern city might be offered a starting salary of $350,000, whereas the same position in Boston might start at $280,000.
- Lower Paying Regions: The Northeast (e.g., Massachusetts, New York) and the West Coast (e.g., California) are generally more competitive markets with a high density of physicians. While the nominal salaries are still high, they are often lower than in other regions when adjusted for the staggering cost of living.
- Cost of Living Adjustment is Key: A $400,000 salary in Jackson, Mississippi, provides a vastly different lifestyle than a $420,000 salary in Los Angeles. Aspiring physicians must analyze compensation packages in the context of local housing costs, taxes, and overall expenses to understand their true earning power.
Illustrative State-Level Salary Data (Estimates):
| State | Estimated Average Annual Salary | Commentary |
| ---------------- | ------------------------------- | ---------------------------------------------- |
| Wisconsin | $385,000+ | High demand, strong health systems, lower CoL. |
| Alabama | $370,000+ | Significant need for specialists in the region. |
| Texas | $350,000+ | Large state with many underserved areas. |
| Florida | $340,000+ | Large aging population drives demand. |
| New York | $295,000+ | Saturated market, especially in NYC. |
| California | $310,000+ | High CoL, desirable location lowers salary leverage. |
*Source: Consolidated data from physician recruiting firms and job board postings.*
###
4. Practice Setting and Employment Model
The type of organization a sleep doctor works for is a critical determinant of both their salary structure and overall career experience.
- Private Practice (Group or Solo): This model offers the highest income potential. After an initial period as an employee, a physician can become a partner. Partners not only earn from their own clinical work but also share in the profits from the entire practice, including the sleep lab's technical fees, DME (Durable Medical Equipment) revenue from CPAP sales, and the work of other providers. However, this comes with the risks and responsibilities of a business owner: managing overhead, staff, billing, and marketing. Potential Income: $400,000 - $700,000+ for a successful partner.
- Hospital or Health System Employment: This is the most common model today. It offers a more predictable and stable career path. The hospital handles all administrative burdens, providing a steady stream of referrals. The compensation is typically a base salary plus a productivity bonus. While the ceiling is lower than private practice, the floor is higher and the benefits are often superior. Potential Income: $280,000 - $450,000.
- Academic Medical Center: Physicians in academic settings (university hospitals) typically earn less than their private practice or even general hospital-employed counterparts. A portion of their time is "protected" for non-clinical activities like teaching medical students, conducting research, and publishing papers. The tradeoff for a lower salary is often a better lifestyle, intellectual stimulation, and robust benefits, including excellent retirement plans and tuition assistance for dependents. Potential Income: $240,000 - $350,000.
- Veterans Affairs (VA) / Government: Working for the VA or other government entities generally offers lower base salaries. However, the benefits are exceptional, including a generous federal pension plan, outstanding job security, and a strong emphasis on work-life balance with little to no weekend or call duties. Potential Income: $230,000 - $320,000.
###
5. Area of Primary Specialty
A sleep physician's original residency training can influence their practice scope and, consequently, their salary. Practices that can offer integrated care are often more profitable.
- **Pulmonology