The hum of ventilators, the rhythmic beeping of cardiac monitors, and the silent, intense focus of a nurse observing a patient's every subtle neurological shift—this is the world of the Neuroscience Intensive Care Unit (Neuro ICU). It's a career path that calls to those with a unique blend of intellectual curiosity, unwavering compassion, and profound resilience. If you're drawn to the intricate complexities of the human brain and have the fortitude for high-stakes critical care, a career as a Neuro ICU nurse is not only one of the most challenging and rewarding in medicine but also one with significant financial potential. The average neuro icu nurse salary in the United States reflects this high level of specialization, often ranging from $85,000 to over $130,000 annually, depending on a variety of key factors we will explore in detail.
I once stood by the bedside of a family member who had suffered a severe traumatic brain injury. Amid the chaos and fear, the calm, knowledgeable presence of the Neuro ICU nurse was our anchor. She didn't just manage the complex machinery; she explained every neurological exam, translated the neurologist's jargon into human terms, and offered a steady hand in our darkest hour. That experience solidified my understanding that these professionals are not just clinicians; they are expert navigators of the most complex human organ and compassionate guides for families in crisis.
This guide is designed to be your comprehensive roadmap to understanding every facet of a Neuro ICU nurse's career, with a special focus on salary and earning potential. We will dissect national salary data, explore the factors that can dramatically increase your income, and lay out the precise steps you need to take to enter and excel in this elite field.
### Table of Contents
- [What Does a Neuro ICU Nurse Do?](#what-does-a-neuro-icu-nurse-do)
- [Average Neuro ICU Nurse Salary: A Deep Dive](#average-neuro-icu-nurse-salary-a-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors-that-influence-your-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Become a Neuro ICU Nurse: A Step-by-Step Guide](#how-to-become-a-neuro-icu-nurse-a-step-by-step-guide)
- [Conclusion: Is a Neuro ICU Career Right for You?](#conclusion-is-a-neuro-icu-career-right-for-you)
---
What Does a Neuro ICU Nurse Do?
A Neuro ICU nurse is a highly specialized registered nurse (RN) who provides intensive care to patients with life-threatening neurological conditions. This goes far beyond the scope of a general floor nurse and even adds a layer of complexity to the role of a general ICU nurse. These professionals are the frontline experts in managing patients suffering from conditions like severe traumatic brain injuries (TBIs), ischemic and hemorrhagic strokes, brain tumors, complex seizures (status epilepticus), spinal cord injuries, and post-operative neurosurgical complications.
Their core responsibility is to continuously monitor and assess a patient's neurological status, recognizing minute changes that could signal a catastrophic decline. They are masters of the neurological exam, meticulously checking pupillary response, motor function, level of consciousness using scales like the Glasgow Coma Scale (GCS), and cranial nerve function. This constant vigilance is critical, as a change in pupil size or a new-onset weakness could be the first sign of rising intracranial pressure (ICP) or an expanding brain hemorrhage.
Key responsibilities and daily tasks include:
- Advanced Neurological Assessments: Performing hourly or even more frequent, detailed neurological exams to detect subtle changes.
- Managing Intracranial Pressure (ICP): Operating and troubleshooting external ventricular drains (EVDs) and other ICP monitoring devices to drain excess cerebrospinal fluid (CSF) and prevent brain herniation.
- Titrating Potent Medications: Administering and carefully adjusting continuous infusions of powerful drugs like vasopressors (to maintain cerebral perfusion pressure), sedatives, and anti-seizure medications.
- Post-Operative Neurosurgical Care: Managing patients after complex procedures like craniotomies, aneurysm clippings, or tumor resections.
- Hemodynamic Monitoring: Interpreting data from arterial lines and central venous catheters to ensure adequate blood flow and oxygenation to the brain.
- Collaboration: Working in lockstep with neurologists, neurosurgeons, pharmacists, and respiratory therapists to create and execute a complex plan of care.
- Patient and Family Education: Translating complex medical information into understandable terms for distressed family members, providing emotional support, and facilitating difficult end-of-life discussions when necessary.
- Emergency Response: Leading the immediate response to acute neurological events, such as a "code stroke" or a sudden spike in ICP.
### A Day in the Life of a Neuro ICU Nurse
Imagine starting your 12-hour shift at 7:00 AM. Your first thirty minutes are spent getting a detailed, bedside report from the night shift nurse on your two assigned patients. One is a 55-year-old man recovering from a craniotomy for a brain tumor, and the other is a 28-year-old woman with a severe TBI from a car accident, who has an EVD in place to manage her intracranial pressure.
From 7:30 AM to 9:00 AM, you conduct your first comprehensive head-to-toe assessments. You meticulously document GCS scores, check pupil responses with a penlight, and test motor strength. You zero the EVD, measure the CSF output, and ensure the ICP reading is within the parameters set by the neurosurgeon.
By 10:00 AM, the multidisciplinary team rounds begin. You present your patients to the neurologist, neurosurgeon, pharmacist, and case manager, providing your expert assessment and collaborating on the plan for the day. You might advocate for a change in sedation to perform a better neuro exam or suggest a specific lab test based on your observations.
The afternoon could bring an emergency. Your TBI patient's ICP suddenly spikes. You immediately raise the head of the bed, ensure her head is in a neutral position, and administer a pre-ordered dose of hypertonic saline, all while alerting the neurosurgery resident. Your swift, calculated actions can be the difference between recovery and irreversible brain damage. The rest of the day is a whirlwind of administering medications, documenting every detail in the electronic health record, supporting a worried family, and preparing for the next shift change, ensuring the next nurse has all the information needed to continue your vigilant watch.
---
Average Neuro ICU Nurse Salary: A Deep Dive
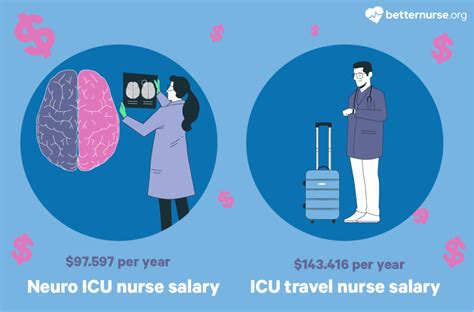
The compensation for a Neuro ICU nurse reflects their advanced skill set, the high-stress environment, and the critical nature of their work. While the U.S. Bureau of Labor Statistics (BLS) provides data for "Registered Nurses" as a broad category, we can analyze data from salary aggregators and professional reports to pinpoint the specific earning potential for this specialty.
The BLS reports that the median annual wage for all Registered Nurses was $81,220 in May 2022. However, nurses working in critical care specialties, particularly in hospitals, earn significantly more.
For a more specialized view, we turn to leading salary data aggregators. According to Salary.com (2024), the average salary for a "Critical Care Nurse" in the United States is approximately $90,360, with a typical range falling between $81,560 and $102,020. Neuro ICU nurses, due to their sub-specialization, often land at the higher end of this range or exceed it, especially with relevant certifications and experience.
Payscale.com (2024) reports a similar trend, showing an average base salary for a Critical Care Nurse (ICU) of around $81,500 per year, but this figure does not typically include the substantial additions from overtime, shift differentials, and bonuses, which can add $10,000 to $30,000+ to the total annual compensation.
### Salary by Experience Level
Your salary as a Neuro ICU nurse will grow substantially as you accumulate experience and expertise. The career path involves a clear and rewarding financial progression.
| Experience Level | Typical Years of Experience | Estimated Annual Base Salary Range | Notes |
| ----------------------- | --------------------------- | ----------------------------------- | ---------------------------------------------------------------------------------------------------------------------------------- |
| Entry-Level | 0-2 Years in ICU | $75,000 - $90,000 | Often requires 1-2 years of med-surg or step-down experience before entering the ICU. Salary is at the lower end of the specialty range. |
| Mid-Career | 3-9 Years in ICU | $90,000 - $115,000 | Likely holds CCRN certification. May be taking on charge nurse or preceptor roles. Comfortable managing complex neurological cases. |
| Senior/Lead | 10+ Years in ICU | $110,000 - $135,000+ | Often holds both CCRN and CNRN certifications. Acts as a unit leader, mentor, and clinical expert. May be on unit-based committees. |
| Advanced Practice | Varies | $125,000 - $180,000+ | Roles like Clinical Nurse Specialist (CNS) or Acute Care Nurse Practitioner (ACNP) with a neuro focus, requiring an MSN or DNP. |
*(Note: These are estimated national averages. Actual salaries can be significantly higher or lower based on the factors discussed in the next section. Data synthesized from Salary.com, Payscale, and Glassdoor as of early 2024.)*
### Beyond the Base Salary: Understanding Total Compensation
A Neuro ICU nurse's W-2 is composed of much more than just their base hourly rate. Understanding the full compensation package is crucial for evaluating a job offer.
- Shift Differentials: This is one of the most significant additions to a nurse's pay. Working night shifts can add 10-20% to your base rate, while weekend shifts can add a similar amount. A nurse working a permanent night shift schedule can see their annual income increase by $15,000 or more.
- Overtime Pay: ICU staffing is critical, and opportunities for overtime are common. All hours worked over 40 in a week (or over a specific daily hour limit, depending on the state and employer) are paid at 1.5 times the base rate.
- On-Call Pay: Some units require nurses to be on-call for emergencies. This involves a small hourly stipend for being available, and if called in, you are paid at an overtime or premium rate.
- Certification Pay: Many hospitals offer a direct pay differential or an annual bonus for nurses who hold specialty certifications like the CCRN (Critical Care Registered Nurse) or CNRN (Certified Neuroscience Registered Nurse). This can range from an extra $1-3 per hour.
- Clinical Ladder Programs: Hospitals often have structured "clinical ladders" that allow nurses to advance and earn more without leaving the bedside. By taking on projects, precepting new nurses, or joining committees, a nurse can climb from a "Clinical Nurse I" to a "Clinical Nurse IV," with each step bringing a significant pay raise.
- Bonuses: Sign-on bonuses for experienced critical care nurses are common, especially in high-demand areas, and can range from $5,000 to $25,000 or more. Annual performance or retention bonuses may also be offered.
- Benefits Package: Don't underestimate the value of a strong benefits package. This includes health, dental, and vision insurance; a robust retirement plan (like a 401(k) or 403(b) with employer matching); paid time off (PTO); and tuition reimbursement, which can be invaluable if you plan to pursue an advanced degree.
When considering a job, always calculate the total compensation, not just the advertised hourly rate. A job with a slightly lower base pay but a massive night shift differential and generous tuition reimbursement may be far more lucrative in the long run.
---
Key Factors That Influence Your Salary
Your earning potential as a Neuro ICU nurse is not a single, fixed number. It's a dynamic figure influenced by a combination of your personal qualifications, where you work, and the specific demands of the healthcare market. Mastering these factors is the key to maximizing your income over the course of your career.
###
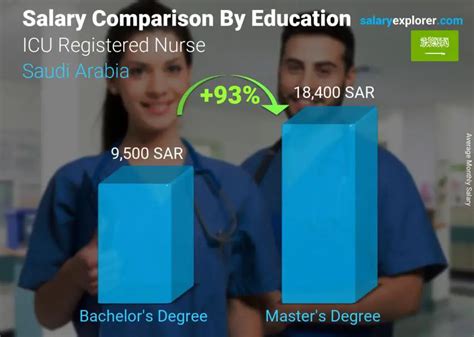
1. Level of Education and Certification
Your educational foundation is the first major determinant of your salary. While you can become an RN with an Associate's Degree in Nursing (ADN), the Bachelor of Science in Nursing (BSN) is the industry standard and a significant factor in pay and opportunity.
- ADN vs. BSN: Most major hospitals, especially Magnet-designated facilities and academic medical centers (where most Neuro ICUs are located), strongly prefer or require a BSN. BSN-prepared nurses are often placed on a higher pay scale from day one. An analysis by Payscale.com consistently shows that BSN-prepared RNs earn several thousand dollars more per year than their ADN-prepared counterparts. Furthermore, a BSN is a prerequisite for nearly all advanced nursing roles.
- Master of Science in Nursing (MSN) / Doctor of Nursing Practice (DNP): Pursuing a graduate degree opens up the highest echelons of nursing pay. An MSN or DNP can qualify you to become a Clinical Nurse Specialist (CNS) or an Acute Care Nurse Practitioner (ACNP). A Neuro-focused ACNP, for example, can perform advanced procedures, manage a caseload of patients under a physician's supervision, and prescribe medications. According to the BLS, the median pay for Nurse Practitioners in 2022 was $121,610, with those in critical care specialties often earning significantly more. This represents a substantial leap in both autonomy and salary.
- Specialty Certifications: This is arguably the most impactful way to increase your salary and marketability as a bedside Neuro ICU nurse. Certifications validate your expertise and are highly valued by employers.
- CCRN (Critical Care Registered Nurse): Offered by the American Association of Critical-Care Nurses (AACN), this is the gold standard for any ICU nurse. It demonstrates a comprehensive knowledge of critical care physiology and practice. Holding a CCRN can add $1 to $3 per hour to your base pay or result in a significant annual bonus. It is a non-negotiable for any serious critical care nurse.
- CNRN (Certified Neuroscience Registered Nurse): Offered by the American Board of Neuroscience Nursing (ABNN), this certification is specific to your specialty. It validates your expertise in managing patients with neurological disorders. Holding *both* the CCRN and CNRN makes you an elite candidate. It signals to employers that you are a dedicated expert, which often translates directly into higher pay, preference for competitive positions, and opportunities for leadership roles like charge nurse or preceptor.
###
2. Years of Experience
Experience is king in critical care. The salary growth trajectory for a Neuro ICU nurse is steep in the first decade of practice. A new graduate RN cannot step directly into a Neuro ICU; they must first build a foundation.
- The Foundation (Years 0-2): A new nurse will typically spend 1-2 years on a Medical-Surgical or Telemetry/Step-down unit. Here, they master fundamental skills like time management, medication administration, and basic patient assessment. The salary is that of a general RN.
- The Transition (Years 2-4): After gaining foundational experience, a nurse can transition into a general or Neuro ICU. During these early years in the ICU, your learning curve is immense. Your salary sees a significant jump from the general floor, moving into the specialized critical care pay bracket. You'll focus on mastering ICU skills and preparing for your CCRN.
- The Expert (Years 5-10): This is where earning potential truly accelerates. As a mid-career Neuro ICU nurse, you are proficient, confident, and efficient. You can handle the most complex patients with minimal supervision. You've likely earned your CCRN and possibly your CNRN. You begin precepting new nurses and taking on charge nurse shifts, both of which come with pay differentials. Your base salary is now firmly in the upper-tier of nursing pay.
- The Leader (Years 10+): A senior Neuro ICU nurse with over a decade of experience is an invaluable asset. They are clinical leaders, mentors, and troubleshooters. Their salary reflects this deep expertise. Many nurses at this stage are at the top of their hospital's clinical ladder, earning the highest possible bedside pay. Others leverage this experience to move into roles like unit educator, manager, or pursue an advanced practice degree.
###
3. Geographic Location
Where you choose to work is one of the single largest factors influencing your salary. Nursing pay varies dramatically by state, city, and even between urban and rural areas within the same state. This variation is often tied to the local cost of living, the strength of nursing unions, and regional demand.
According to the BLS (May 2022 data), the top-paying states for Registered Nurses overall are:
1. California: Annual mean wage of $133,340
2. Hawaii: Annual mean wage of $113,220
3. Oregon: Annual mean wage of $106,610
4. Washington: Annual mean wage of $104,110
5. Alaska: Annual mean wage of $103,310
Neuro ICU nurses in these states, particularly in high-cost-of-living metropolitan areas like the San Francisco Bay Area, Los Angeles, or Seattle, can earn significantly more than these averages. It is not uncommon for an experienced, certified Neuro ICU nurse in California to earn well over $150,000 per year with differentials and overtime.
Conversely, states in the Southeast and parts of the Midwest tend to have lower average nursing salaries. However, it's crucial to balance salary with the cost of living. A $95,000 salary in a city with a low cost of living may provide a better quality of life than a $125,000 salary in a city where housing costs are exorbitant.
Highest-Paying Metropolitan Areas for RNs (BLS, May 2022):
- San Jose-Sunnyvale-Santa Clara, CA: $173,530
- San Francisco-Oakland-Hayward, CA: $164,760
- Vallejo-Fairfield, CA: $158,540
- Napa, CA: $152,700
- Sacramento--Roseville--Arden-Arcade, CA: $147,490
###
4. Facility Type and Size
The type of hospital you work for also plays a major role in your compensation.
- Large Academic Medical Centers / Level I Trauma Centers: These facilities, often affiliated with universities, handle the most complex neurological cases in a region. They require the highest level of skill and specialization, and their pay reflects this. They are also more likely to be unionized, which generally leads to higher wages, better benefits, and structured pay scales. These are typically the highest-paying employers for Neuro ICU nurses.
- Private, For-Profit Hospitals: These can be a mixed bag. Some large, for-profit hospital systems offer competitive salaries and large sign-on bonuses to attract top talent. Others may prioritize cost-cutting, which can impact staffing and compensation.
- Non-Profit Hospitals: This is the most common type of hospital in the U.S. Salaries are generally competitive and often fall in line with regional averages. Many prestigious institutions like the Mayo Clinic or Cleveland Clinic are non-profits.
- Government Facilities (e.g., VA Hospitals): The Department of Veterans Affairs (VA) is a major employer of nurses. VA hospitals offer excellent federal benefits, robust retirement plans (pensions), and often have competitive pay scales that are publicly available. For many, the benefits package at a VA hospital can outweigh a slightly higher base salary elsewhere.
###
5. In-Demand Clinical and Soft Skills
Beyond formal certifications, possessing specific, high-level skills can make you a more valuable and thus higher-paid nurse.
- Advanced Device Management: Expertise in managing complex devices like EVDs, ICP monitors, and continuous EEG monitoring is fundamental. Nurses who can troubleshoot these devices independently are highly sought after.
- CRRT (Continuous Renal Replacement Therapy): Many critically ill neuro patients also develop acute kidney injury. Nurses who are trained and certified to operate CRRT machines are extremely valuable to an ICU and often receive a pay differential for running the therapy.
- ECMO (Extracorporeal Membrane Oxygenation): While less common in a purely neuro setting, some larger centers use ECMO. Being an ECMO-trained specialist is an elite skill that commands premium pay.
- Leadership and Communication: These "soft skills" have a tangible impact on pay. The ability to remain calm and communicate clearly during a crisis, effectively mentor new nurses as a preceptor, and lead the team as a charge nurse are all pathways to higher pay through formal role differentials and advancement on the clinical ladder.
- Tech Savviness: Proficiency with electronic health records (EHRs) and other hospital information systems is crucial. Nurses who become "super-users" or help with system implementation can often find additional paid opportunities.
---
Job Outlook and Career Growth

The career outlook for Neuro ICU nurses is exceptionally strong. This optimism is driven by several powerful, long-term trends in healthcare and demographics, ensuring high demand and job security for the foreseeable future.
The U.S. Bureau of Labor Statistics (BLS) projects that overall employment for Registered Nurses will grow by 6 percent from 2022 to 2032, which is faster than the average for all occupations. This will result in about 177,400 openings for registered nurses each year, on average, over the decade. Many of those openings are projected to result from the need to replace workers who transfer to different occupations or exit the labor force, such as to retire.
For Neuro ICU nurses, the outlook is even more robust for several key reasons:
1. The Aging Population: The large baby boomer generation is aging, leading to a higher incidence of age-related neurological conditions. Strokes, which are a primary reason for admission to a Neuro ICU, are far more common in older adults. Likewise, neurodegenerative diseases, brain tumors, and other conditions requiring intensive neurological care are on the rise.
2. Advancements in Medical Technology and Treatment: Decades ago, many of the conditions treated in a Neuro ICU today were considered untreatable. Advances in neuro-interventional radiology (like mechanical thrombectomy for strokes), neurosurgery, and critical care medicine mean that more patients are surviving previously fatal events. These survivors require prolonged, highly specialized intensive care, directly fueling the demand for Neuro ICU nurses.
3. Increased Emphasis on Specialized Care: Hospitals and healthcare systems recognize that specialized units lead to better patient outcomes. As a result, more hospitals are developing dedicated Neuro ICU or Neuro-critical Care units, creating a specific demand for nurses with this unique skill set. General ICU nurses are valuable, but facilities will always prefer a nurse with proven neuroscience expertise for these roles.
4. High Acuity and Nurse Burnout: The intensity of the Neuro ICU environment contributes to a higher rate of burnout and turnover compared to less acute settings. While a challenge for the profession, this unfortunately ensures a constant demand for new, resilient nurses to fill vacancies.
### Emerging Trends and Future Challenges
To stay relevant and continue to advance, Neuro ICU nurses must be aware of the evolving landscape of their specialty.
- Tele-ICU (eICU): This trend is growing rapidly. Experienced critical care nurses can work from a remote command center, monitoring patients in multiple ICUs via cameras and real-time data streams. They act as a second set of expert eyes, assisting bedside nurses with complex cases and emergency response. This creates new career pathways for senior nurses who may want to move away from the physical demands of 12-hour bedside shifts.
- AI and Predictive Analytics: Artificial intelligence is beginning to play a role in the ICU. New algorithms can analyze streams of data from monitors to predict which patients are at high risk for sepsis or neurological decline, allowing for earlier intervention. Nurses of the future will need to be comfortable working alongside these technologies.
- Focus on Post-ICU Syndrome (PICS): There is a growing recognition of the long-term cognitive, psychological, and physical impairments that patients face after a critical illness. Neuro ICU nurses are on the front lines of preventing and mitigating these issues, requiring a more holistic, long-term view of patient recovery.
The primary challenge remains burnout. The emotional and mental toll of caring for critically ill patients and their families is immense. Successful long-term Neuro ICU nurses are those who develop strong coping mechanisms, maintain a healthy work-life balance, and work in supportive environments with adequate staffing and resources.
### How to Advance in the Field
- Never Stop Learning: Commit to lifelong learning. Regularly read professional publications like the *Journal of Neuroscience Nursing*. Attend national conferences like the AANN Annual Conference or the AACN National Teaching Institute & Critical Care Exposition.
- Pursue Advanced Roles: Don't view bedside nursing as the only endpoint. Plan your career trajectory. Consider becoming a Charge Nurse, Unit Educator, Nurse Manager, or pursuing an advanced practice degree to become a CNS or ACNP.
- Join Professional Organizations: Membership in the **American Association of Neuroscience